That sudden jolt of electricity shooting from your lower back down your leg isn’t just a regular ache—it’s the unmistakable signature of lower back nerve pain. When everyday movements like bending to tie your shoes or sitting at your desk trigger sharp, radiating discomfort, you’re experiencing what millions of adults face annually. Lower back nerve pain, commonly called sciatica, affects up to 40% of people during their lifetime and transforms simple tasks into painful challenges.
This condition occurs when something compresses or irritates the sciatic nerve—the largest nerve in your body stretching from your lower spine to your feet. While the pain feels overwhelming, understanding the root cause is your first step toward effective relief. The good news? Approximately 80-90% of lower back nerve pain cases improve without surgery within weeks when addressed properly.
In this guide, you’ll discover how to identify your specific nerve compression pattern, implement immediate pain relief strategies that work, and determine when to seek professional help. Most importantly, you’ll learn proven exercises and long-term prevention techniques to keep your sciatic nerve free from compression.
Sharp Leg Pain Patterns Revealed
Lower back nerve pain creates a distinctive pain signature that helps identify nerve involvement. This pain typically starts in your lower back or buttock, then radiates down one leg following specific nerve pathways. Patients describe it as “knife-like,” electrical, or severe cramping that can persist for weeks and intensifies with movement—especially bending forward, twisting, or even coughing and sneezing.
Unlike general back pain, lower back nerve pain follows precise anatomical routes. The classic pattern runs from your hip through the back of your thigh, sometimes reaching your calf or foot. This isn’t random discomfort; it maps directly to which specific nerve root (L4, L5, or S1) is being compressed in your lumbar spine.
Herniated Discs: The Leading Cause Under 40
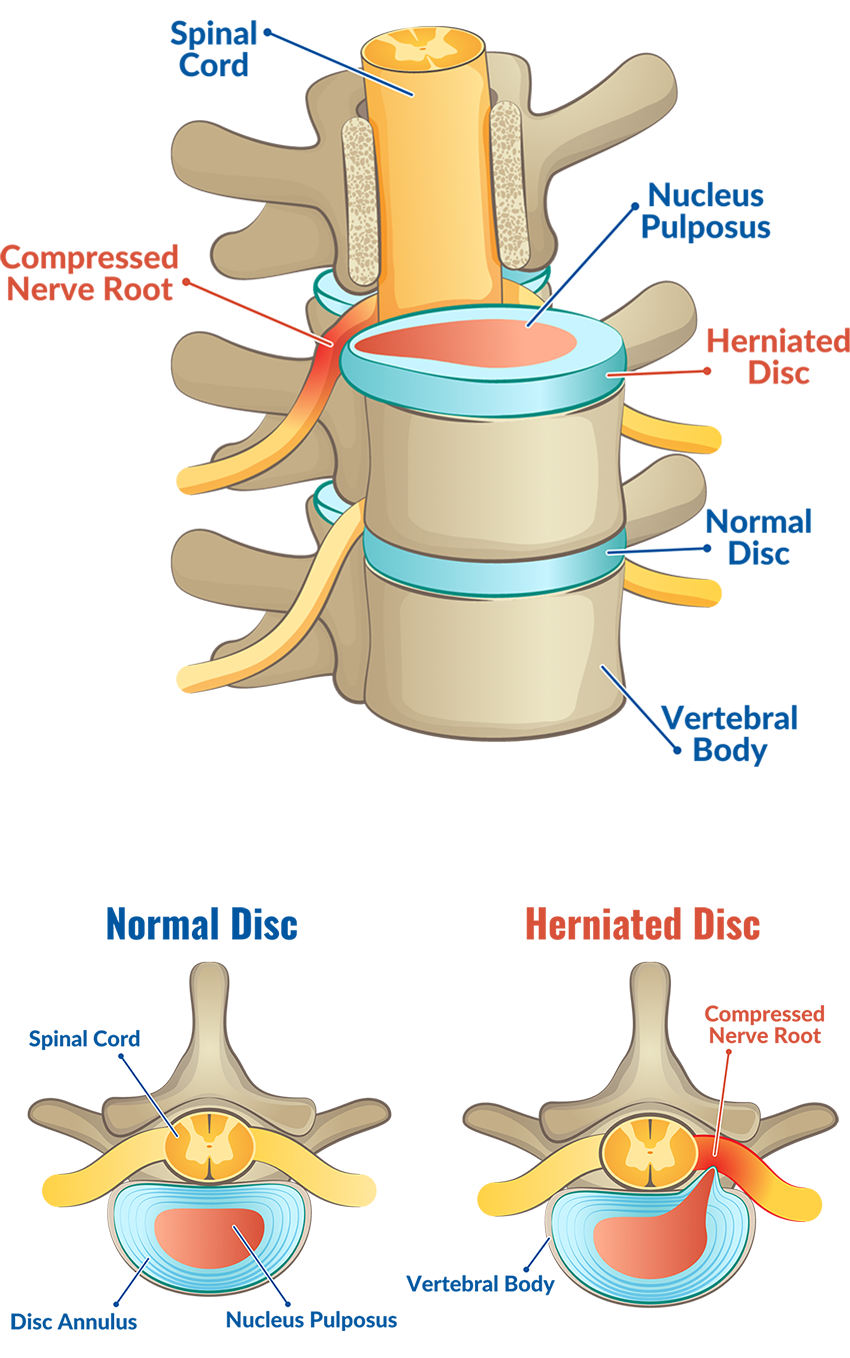
Bulging or herniated discs cause 90% of lower back nerve pain cases in people under 40. When the soft inner portion of a spinal disc pushes through its tougher exterior, it can press directly against nerve roots. This creates the classic sciatica pattern—sharp pain radiating down the leg that worsens with sitting, coughing, or straining.
Age dramatically influences your likely cause. Under 40, herniated discs dominate as the primary culprit. After 40, bone spurs and arthritis become more common, gradually narrowing the spaces where nerves exit the spine. This age-related shift explains why treatment approaches must be tailored to your specific condition.
Straight Leg Raise: Your At-Home Diagnostic Test
Lie flat on your back and slowly raise your affected leg straight up while keeping your knee extended. If lower back nerve pain shoots down your leg between 30-70 degrees of elevation, this strongly suggests sciatic nerve compression. The crossed straight leg test adds diagnostic power—pain in your symptomatic leg when raising your unaffected leg indicates significant nerve root compression.
Functional Movement Screening
Try these simple tests to assess nerve involvement:
– Walk on your heels (tests L4/L5 nerve roots)
– Walk on your toes (tests S1 nerve root)
– Squat and rise slowly (identifies functional limitations)
Difficulty with any movement points to specific nerve root involvement. Note which activities trigger your worst symptoms—this information guides treatment selection. Remember, these tests support but don’t replace professional evaluation. Persistent symptoms lasting over a week warrant medical assessment.
Immediate Ice and Heat Relief Protocol
During the first 48 hours of an acute flare-up, apply ice packs to your lower back for 15-20 minutes every 2-3 hours. This reduces inflammation around the compressed nerve. After the initial 48-hour period, switch to heat therapy using a heating pad on medium heat for 15-20 minutes, 3-4 times daily to promote blood flow and healing.
Critical positioning strategy: Find your pain-relieving position immediately. Many find relief lying on their back with knees elevated on pillows. Others prefer side-lying with a pillow between knees. Avoid prolonged sitting—stand and walk every 30 minutes to prevent nerve compression from worsening. These simple position changes can reduce pain intensity within hours.
McKenzie Extension Protocol: First-Line Exercise
Start with prone lying: lie face down for 2-3 minutes. Progress to prone on elbows for 2-3 minutes. Finally, perform press-ups—keeping your hips down while pushing up with your arms, holding 10 seconds, repeating 10 times. This sequence centralizes leg pain back toward the spine, indicating disc material is moving away from the nerve.
Piriformis Stretching for Quick Relief
Tight piriformis muscles can compress the sciatic nerve, causing lower back nerve pain. Perform figure-4 stretches: lie on your back, cross your affected leg over the opposite thigh, and gently pull toward your chest until you feel a stretch in your buttocks. Hold 30 seconds, repeat 3 times daily. This simple stretch often provides noticeable relief within days for piriformis-related nerve compression.
When Surgery Moves from Option to Necessity
Surgery becomes a serious consideration when leg pain remains disabling after 3+ months of conservative treatment. Failed physical therapy, persistent weakness, or worsening nerve compression on imaging indicate surgical evaluation may be necessary. However, remember that 80-90% of patients improve without surgery—exhaust all conservative options first before considering surgical intervention.
Microdiscectomy vs. Laminectomy: What Works Best
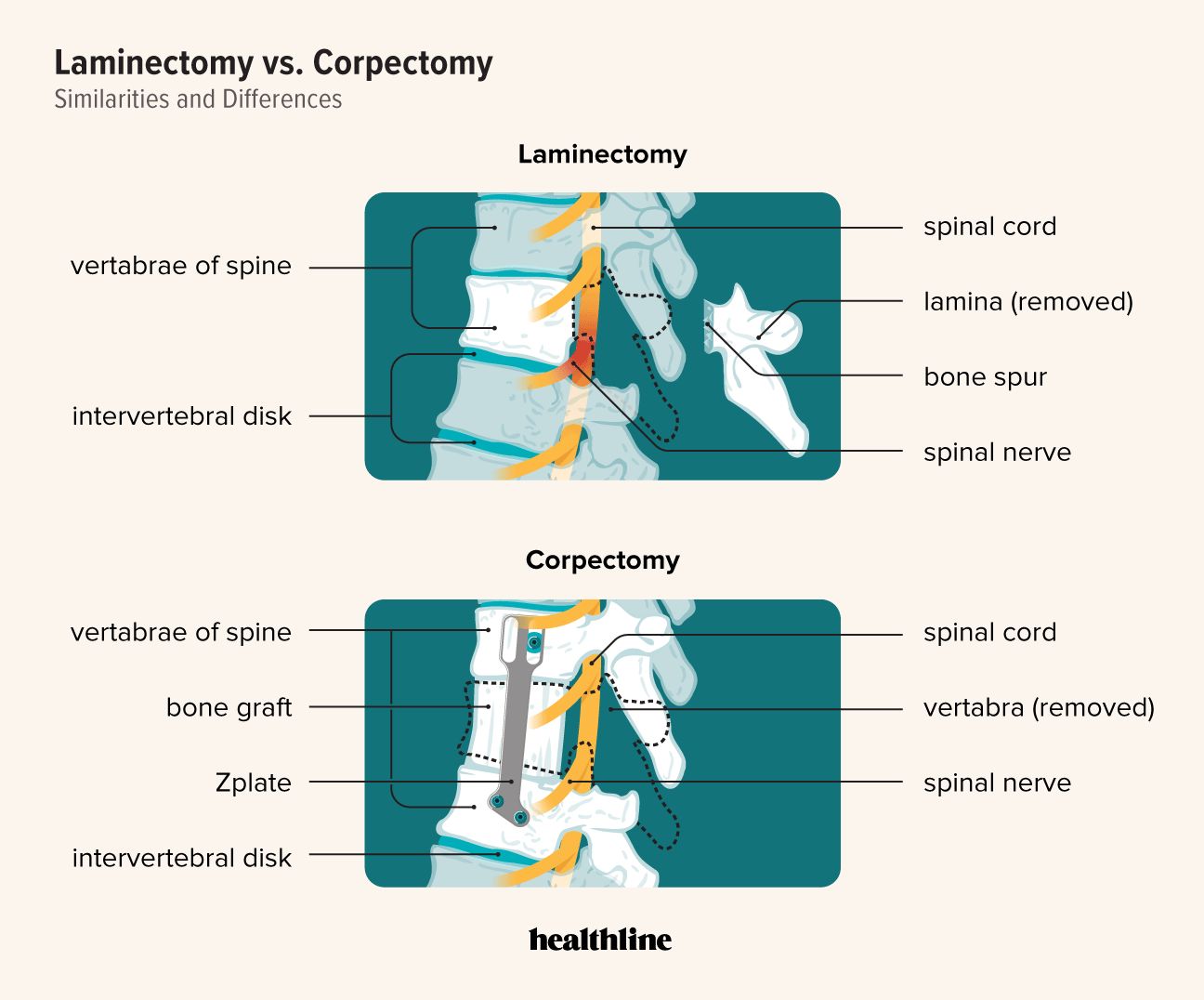
Microdiscectomy removes herniated disc portions compressing nerves through a small incision, while laminectomy creates more space by removing bone spurs or ligament overgrowth. Both procedures typically use small incisions with minimal tissue disruption. Success rates exceed 70% for leg-dominant pain, though results vary significantly by underlying cause and patient factors.
Emergency Red Flags You Can’t Ignore
Seek immediate medical attention if you experience:
– Loss of bladder or bowel control
– Numbness in the “saddle” area (groin, inner thighs)
– Severe progressive weakness in both legs
– Fever, chills, or night sweats accompanying your nerve pain
These symptoms indicate potentially serious conditions like cauda equina syndrome or spinal infection requiring treatment within 24-48 hours to prevent permanent nerve damage. Don’t dismiss these warning signs—they represent medical emergencies that need immediate professional evaluation.
Long-Term Prevention: Your Nerve Protection Plan
Maintain a healthy weight—every extra pound adds approximately 4 pounds of pressure on your lower spine. Quit smoking immediately; nicotine reduces blood flow to spinal discs, accelerating degeneration. Optimize your workspace ergonomics—keep feet flat on the floor, knees at 90 degrees, and your monitor at eye level to minimize spinal stress throughout your workday.
Your Lifetime Exercise Prescription
Commit to lifelong core strengthening with these nerve-protective exercises:
– Planks: Start with 20-second holds, building to 60 seconds
– Bridges: Lie on back, lift hips while squeezing glutes
– Bird-dogs: On hands and knees, extend opposite arm and leg
Incorporate regular walking—start with 10-15 minutes daily, building to 30 minutes. Swimming and cycling provide cardiovascular benefits without spinal impact. Consistent exercise reduces recurrence risk by 50% compared to sedentary lifestyles.
Two-Week Recovery Timeline: What to Expect
First 72 hours: Expect significant pain fluctuations—this is normal. Focus on gentle movement within pain limits, anti-inflammatory measures, and avoiding activities that worsen symptoms. Most acute cases show 30-50% improvement within this critical window.
Days 4-14: Gradually increase walking distance while continuing McKenzie exercises. Pain should gradually centralize toward your spine rather than radiating down your leg. If pain isn’t improving or worsens during this phase, consult a physical therapist for personalized guidance.
Three-Month Recovery Milestones
By the three-month mark, most lower back nerve pain cases show substantial improvement with proper conservative management. Progressive strengthening becomes key as pain subsides. You should be able to return to modified work duties and daily activities with minimal restrictions.
Recurrent flare-ups remain common during this phase—have a management plan ready with your immediate relief strategies. If you haven’t seen at least 70% improvement by three months, consult a spine specialist for advanced treatment options before considering surgical evaluation.
Lower back nerve pain responds best to early, comprehensive treatment. Start with conservative measures—most cases resolve within weeks with proper self-care. Stay active within pain limits, strengthen your core gradually, and seek professional help when symptoms persist beyond two weeks or worsen despite home treatment. Your spine supports your entire body—invest in its care today to prevent chronic pain tomorrow.

