That sharp twinge when you bend to tie your shoes. The dull ache that turns sleep into torture. Lower back pain hijacks your life without warning, making basic movements feel impossible. If you’re searching for real relief right now, you’re not alone—nearly 23% of adults worldwide battle chronic lower back pain that disrupts work, sleep, and daily joy. The good news? Most cases respond dramatically to targeted strategies you can start today. This guide delivers clinically proven steps to reduce lower back pain fast, prevent future flare-ups, and get you moving freely again—no expensive treatments required.
Stop guessing which remedies actually work. You’ll discover exactly how to apply ice versus heat for maximum relief, perform doctor-approved exercises that strengthen your spinal armor, and adjust daily habits causing silent damage. Most importantly, you’ll learn to recognize danger signs requiring immediate medical help before minor pain becomes permanent damage. Let’s transform your discomfort into control.
Why Your Lumbar Region Bears the Brunt of Daily Stress
Your lower back handles extraordinary forces daily—it supports your entire upper body weight while enabling twisting, bending, and lifting. When this complex system of muscles, disks, and vertebrae gets overloaded, pain becomes your body’s urgent warning signal. Understanding your specific pain trigger is the first step toward effective relief.
Muscle Strains Versus Structural Damage
Sudden movement injuries cause most acute pain episodes. Lifting groceries with a twisted torso or sneezing violently can tear overstretched back muscles, creating sharp localized pain that worsens with movement. These typically heal within 2-6 weeks with proper care.
Disk-related nerve compression delivers different misery. A bulging or herniated disk presses on spinal nerves, causing electric-shock sensations radiating down your leg (sciatica). You’ll feel this as burning pain that intensifies when sitting or coughing.
Arthritis-driven stiffness creeps in gradually. Degenerative joint changes cause morning rigidity that improves slightly with movement but returns after prolonged sitting. Unlike strains, this pain builds steadily throughout the day.
Hidden Risk Factors Accelerating Your Pain
Excess body weight multiplies spinal stress—each extra pound adds four pounds of pressure on your lumbar disks during walking. This isn’t just theory; imaging studies show visibly narrower disk spaces in overweight patients.
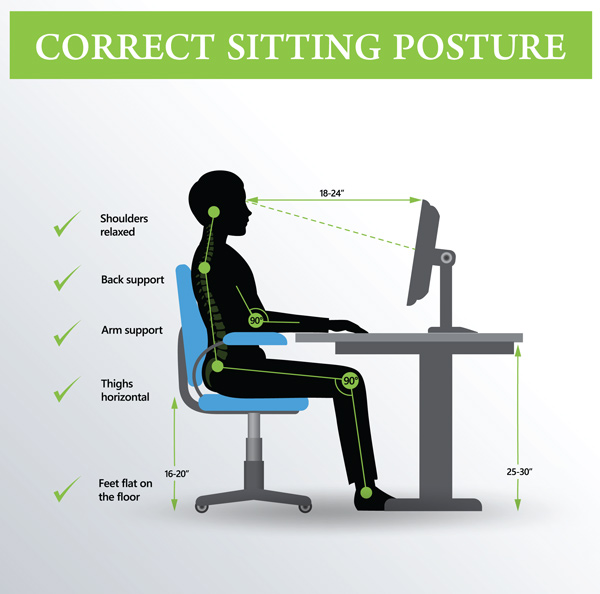
Sedentary work habits silently weaken core stabilizers. Sitting more than 30 minutes without posture checks causes your deep abdominal muscles to “shut off,” forcing your lower back to bear unsupported upper body weight. Within hours, this triggers muscle spasms.
Immediate Pain Relief Protocol (First 72 Hours)

When pain strikes, your first actions determine recovery speed. Skip the “wait and see” approach—these evidence-based steps reduce inflammation and prevent minor strains from becoming chronic issues.
Ice and Heat Application Timeline
Apply ice immediately for 15 minutes every 2 hours during the first 24 hours. Wrap frozen peas or an ice pack in thin cloth—direct skin contact risks frostbite. You’ll know it’s working when the area feels numb, not painfully cold. Critical mistake: Never ice longer than 20 minutes per session; extended exposure restricts blood flow needed for healing.
Switch to moist heat after 48 hours if stiffness dominates. Use a microwaveable rice sock or warm shower for 15-20 minutes. Heat relaxes knotted muscles but never apply it to fresh injuries—it worsens inflammation.
Movement That Accelerates Healing
Walk every 90 minutes for 5-10 minutes. Start slowly on flat surfaces—your goal is gentle circulation, not exercise. Proper gait reduces disk pressure by 25% compared to sitting. Stop immediately if pain shoots down your leg.
Avoid these common errors:
– Complete bed rest (weakens supporting muscles)
– Reaching for painkillers before trying movement
– Forcing stretches that increase pain
Core Strengthening Exercises That Target Pain at the Source
Weak core muscles force your lower back to overwork. These three precision exercises rebuild your natural spinal support system without straining injured tissues. Perform daily for 4 weeks to cut recurrence risk by 50%.
Pelvic Tilts: The Foundational Stabilizer
Lie on your back with knees bent, feet flat on floor. Inhale deeply, then exhale while gently drawing your belly button toward your spine. Press your lower back flat against the floor—you should feel deep abdominal engagement, not back strain. Hold 5 seconds, relax. Complete 3 sets of 15 repetitions daily. Pro tip: Place a phone book under your sacrum (tailbone area) for instant feedback—successful tilts lift your tailbone slightly off the surface.
Bird Dog: Balance Without Back Strain
Start on hands and knees with wrists under shoulders, knees under hips. Engage your core as in pelvic tilts. Slowly extend right arm forward and left leg back until parallel with floor—keep hips level; don’t let them rock. Hold 3 seconds, return to start. Alternate sides for 10 repetitions per side. Warning: If you feel lower back arching, reduce extension distance. Proper form prevents reinjury.
Wall Sits: Functional Strength Builder
Stand with back against wall, feet shoulder-width apart 24 inches from wall. Slide down slowly until knees form 45-degree angles (not 90 degrees—this strains lumbar spine). Check alignment: Your tailbone should touch the wall throughout. Hold 20 seconds, rest 10 seconds. Build to 5 repetitions. Time-saver: Do this while brushing teeth—multitasking that delivers results.
Daily Habit Adjustments Preventing Recurring Pain
Small consistent changes outperform occasional heroic efforts. These evidence-based tweaks address the root causes of 80% of recurring back pain episodes.
Weight Management: The Silent Pain Amplifier
Lose just 5 pounds to remove 20 pounds of pressure from your lumbar spine during walking. Focus on anti-inflammatory foods: fatty fish (salmon, mackerel), berries, leafy greens, and walnuts. Avoid the trap: Sugary drinks and processed snacks increase inflammation markers linked to chronic pain.
Track progress visually with a posture mirror. Stand sideways daily—excess abdominal weight shifts your center of gravity forward, forcing lower back muscles into constant overdrive. Even modest weight loss visibly improves alignment within 3 weeks.
Smart Sitting and Lifting Modifications
Set a phone timer for every 25 minutes of sitting. When it chimes:
1. Stand up immediately
2. Perform 5 pelvic tilts
3. Take 10 steps forward
This prevents the “sitting slump” that compresses spinal disks by 40% compared to standing.
Master the safe lift:
– Stand within 6 inches of object
– Bend knees deeply while keeping back straight
– Hug item close to chest
– Pivot feet (don’t twist torso) when turning
Red flag: If you can’t see your feet while lifting, you’re straining your back.
Emergency Warning Signs Requiring Immediate Medical Help

Most back pain resolves with self-care, but certain symptoms indicate urgent intervention. Ignoring these could cause permanent nerve damage.
Nerve Compression Danger Signals
Seek ER care immediately if you experience:
– Numbness in “saddle area” (inner thighs, genitals)
– Loss of bladder or bowel control
– Progressive leg weakness (tripping while walking)
These indicate cauda equina syndrome—a surgical emergency where disk material compresses critical nerves.
Schedule same-day appointment for:
– Pain radiating below the knee
– Tingling in feet
– Symptoms worsening at night
These suggest significant nerve root compression needing professional evaluation.
Long-Term Pain Prevention Roadmap
True recovery means breaking the cycle of recurring pain. This phased approach builds resilience while adapting to your unique physiology.
6-Week Core Transformation Plan
Weeks 1-2: Focus on pain-free movement. Walk 10 minutes daily, perform pelvic tilts hourly. Goal: Reduce acute pain by 50%.
Weeks 3-4: Add bird dogs and wall sits. Increase walking to 20 minutes. Goal: Eliminate pain during basic activities.
Weeks 5-6: Introduce gentle yoga poses (child’s pose, cat-cow). Goal: Full participation in daily routines without pain medication.
Track progress: Note pain levels (1-10 scale) before/after each exercise. Consistent improvement confirms you’re rebuilding correctly.
Professional Support Worth Investing In
Physical therapy delivers 3x better long-term outcomes than self-treatment. A specialist identifies your specific movement flaws—like hip stiffness forcing your back to over-rotate during golf swings—and designs targeted corrections.
Pain journaling reveals hidden triggers. Log daily:
– Activities before pain onset
– Pain location/intensity
– Sleep quality
Patterns emerge within 2 weeks, guiding precise prevention.
Reducing lower back pain starts with your very next movement. That ice pack applied within the hour, the pelvic tilt performed while waiting for coffee, the conscious decision to lift with bent knees—these micro-actions compound into life-changing relief. Remember the Cleveland Clinic’s insight: 80% of people achieve significant improvement within 6-12 weeks using these evidence-based approaches. Your spine’s remarkable resilience means today’s smart choices create tomorrow’s pain-free reality. Don’t wait for “someday”—download a posture reminder app now, set your first movement timer, and take that first healing walk. Your back’s recovery begins the moment you choose action over agony.

