That persistent lower back throb showing up days after your period ends isn’t normal menstrual fallout—it’s your body signaling something’s wrong. While 30% of women experience post-menstrual back pain, this discomfort often points to underlying issues like endometriosis or muscle dysfunction rather than routine cycle changes. Ignoring this symptom allows temporary pain to escalate into chronic daily discomfort, disrupting work, exercise, and sleep cycles month after month.
Unlike typical period cramps that fade with bleeding, post-period back pain exploits hormonal shifts and neural pathways that keep pain signals active. Understanding why your spine aches after menstruation ends—when relief should come—is critical for targeting treatment. This guide reveals the specific conditions triggering your discomfort and provides time-tested relief strategies you can implement immediately.
Why Your Back Aches Days After Menstruation Ends
Your uterus and lower back share nerve pathways originating from spinal segments T10-L1, creating direct communication channels for pain signals. When estrogen plummets after your period, uterine contractions continue triggering referred pain in your back through these shared nerves. This neural cross-talk explains why some women develop chronic back issues from habitual period hunching that tightens protective muscle guarding long after bleeding stops.
Hormonal shifts compound this effect significantly. The post-period drop in estrogen and relaxin leaves joints temporarily unstable, forcing back muscles to overcompensate for pelvic support. Simultaneously, lingering prostaglandin inflammation from menstrual shedding creates a perfect storm for persistent pain. Women with pre-existing back conditions often experience amplified discomfort during this phase due to the “priming effect” where sensitized uterine tissues heighten pain perception in connected regions.
Medical Conditions Causing Post-Period Back Pain
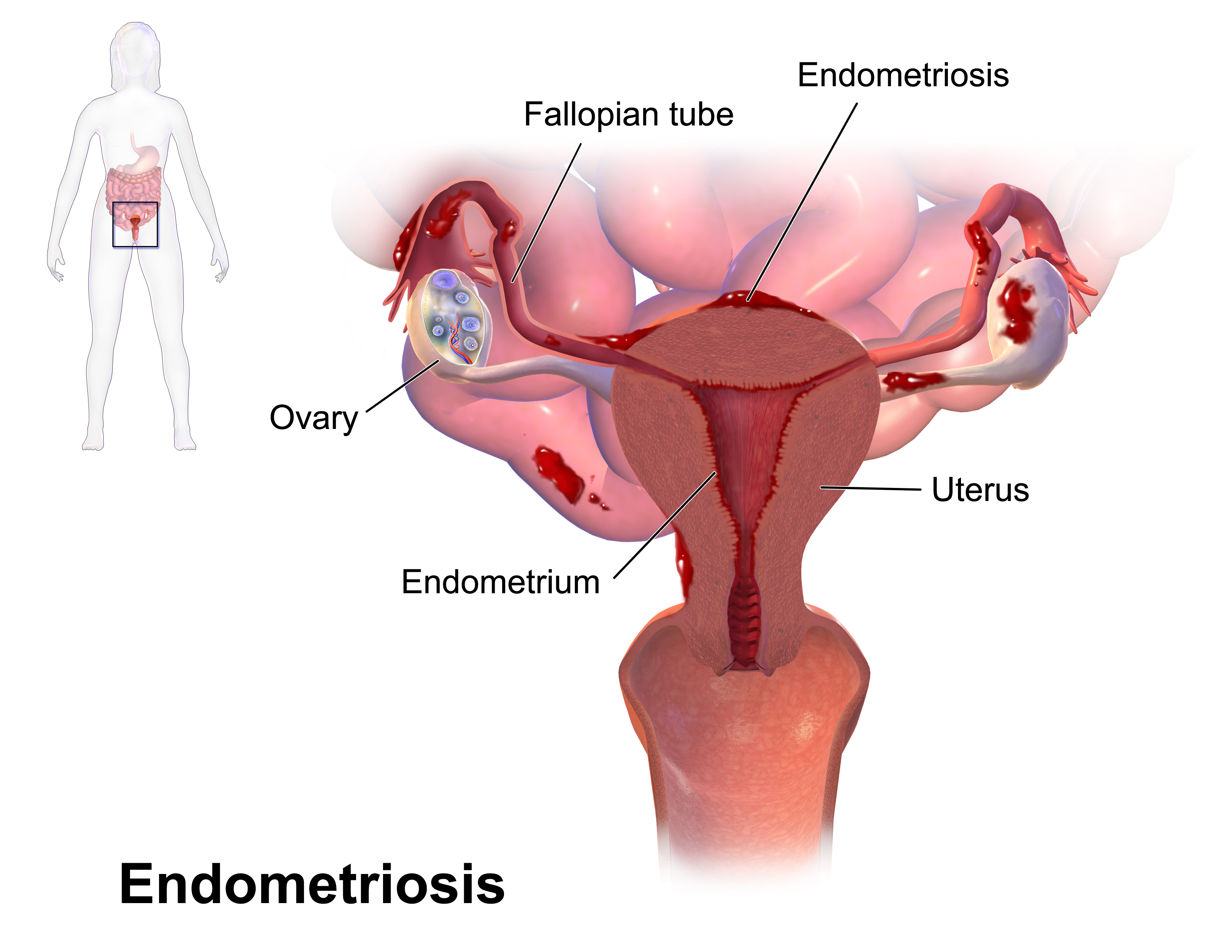
Endometriosis: The Silent Back Pain Trigger
When uterine-like tissue grows outside the uterus (affecting 1 in 10 reproductive-age women), it responds to hormonal cycles even after menstruation ends. This displaced tissue causes inflammation that radiates to the lower back, often worsening 2-5 days post-period. Key red flags include pain during intercourse, bowel movements, and infertility alongside your back discomfort. Laparoscopic surgery remains the gold standard for diagnosis when these symptoms cluster together.
Adenomyosis: Uterine Wall Dysfunction Spreading Pain
In adenomyosis, endometrial tissue invades the uterine muscle wall, creating a thickened, tender organ that generates intense cramping. This muscle dysfunction spreads to surrounding structures, causing lower back pain that peaks 3-7 days after your period concludes. Heavy bleeding with large clots and persistent pelvic pressure typically accompany this condition, distinguishing it from ordinary menstrual issues.
Fibroids Pressing on Nerve Pathways
Subserosal fibroids—those growing on the uterus’s outer surface—exert direct pressure on pelvic nerves and spinal structures. After your period, as the uterus contracts to expel residual blood, this pressure intensifies, causing persistent lower back pain. Women with multiple fibroids often describe a deep pelvic heaviness extending upward along the spine, particularly noticeable when sitting for prolonged periods.
Ovarian Cysts Rupturing Post-Menstruation
Functional cysts (follicular or corpus luteum) typically resolve spontaneously but can rupture days after your period ends. This causes sudden, sharp back pain localized to one side, often accompanied by bloating or spotting between cycles. The pain feels distinctly different from menstrual cramps—more stabbing and less rhythmic—and may require medical evaluation if severe.
Ectopic Pregnancy: The Emergency You Can’t Ignore
Though rare (1-2% of pregnancies), ectopic pregnancy presents as severe cramping and back pain after a missed or abnormal period. This life-threatening condition requires immediate care when paired with shoulder pain (from internal bleeding irritating the diaphragm), dizziness, or positive pregnancy tests with intense pelvic discomfort. Never dismiss post-period back pain if you’ve had unprotected sex.
Quick Symptom Assessment for Accurate Diagnosis
Match your pain pattern to these triggers:
– Days 1-3 post-bleeding: Hormonal fluctuations or uterine contractions (adenomyosis/fibroids)
– Mid-cycle (around day 14): Ovulation-related mittelschmerz
– Persistent beyond 5 days: Endometriosis or chronic pelvic inflammatory disease
Critical symptom combinations:
– Heavy bleeding + large clots → Adenomyosis or fibroids
– Painful intercourse + infertility → Endometriosis
– Fever + foul discharge → Pelvic inflammatory disease
– Missed period + shoulder pain → Ectopic pregnancy
Immediate Relief Strategies That Work in 24 Hours
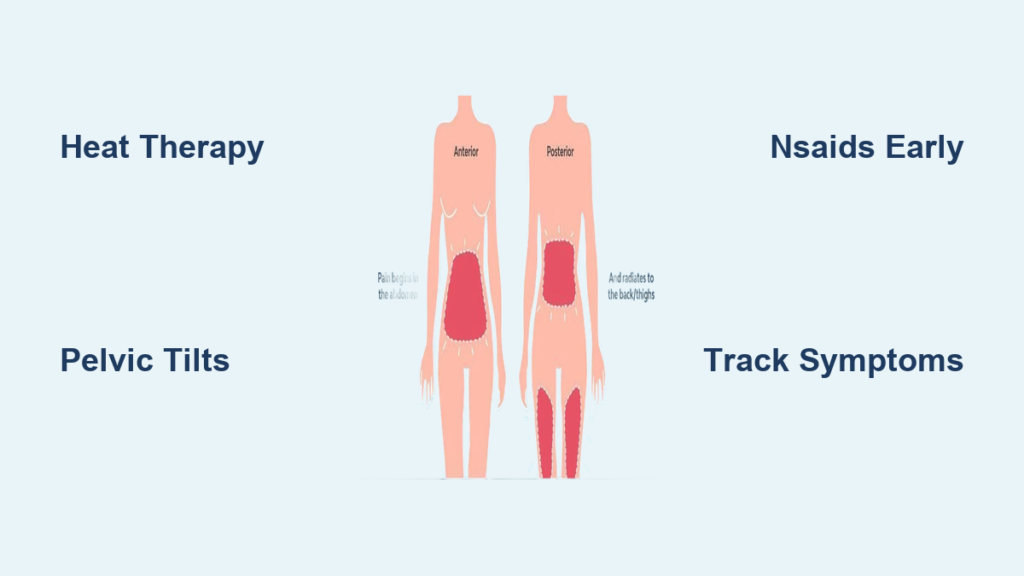
Heat Therapy Protocol for Post-Period Back Pain
Apply moist heat directly to your lower back for 15-20 minutes, 2-3 times daily using a microwavable pad or warm bath. This relaxes muscles tightened by referred uterine contractions and increases blood flow to flush inflammation. For all-day relief at work, use adhesive heat patches delivering consistent 104°F warmth for 8-12 hours—proven to reduce muscle guarding within hours.
Targeted Stretching Routine for Back Muscle Release
Perform these stretches daily during your post-period phase:
– Child’s pose: Kneel, sit back on heels, and stretch arms forward while lowering chest toward floor. Hold 45 seconds to lengthen tight lower back muscles.
– Pelvic tilts: Lie on back with knees bent. Flatten lower back against floor by tightening abdominal muscles. Hold 5 seconds, repeat 12 times to stabilize core support.
– Knee-to-chest: Hug one knee to chest for 30 seconds, then switch legs. Repeat 3 times per side to relieve sacroiliac joint pressure.
Anti-Inflammatory Nutrition Plan
Combat prostaglandin-driven inflammation by prioritizing:
– Omega-3 rich foods: Wild salmon, chia seeds, or walnuts at every meal
– Deep-colored berries: Blueberries and cherries in morning smoothies
– Leafy greens: Spinach or kale sautéed with garlic for dinner
Avoid processed foods, excess salt, and caffeine for 5 days post-period. Drink 8-10 glasses of water daily to support muscle recovery—dehydration worsens uterine cramping and back tension.
Effective Pain Management Options
Over-the-Counter Medication Timing
Take ibuprofen (400mg) or naproxen (220mg) at the first sign of post-period pain—not when it peaks. These NSAIDs block prostaglandin production most effectively when initiated early. Limit use to 3 consecutive days to prevent stomach irritation, and always take with food. For nerve-related pain, combine with heat therapy for synergistic relief.
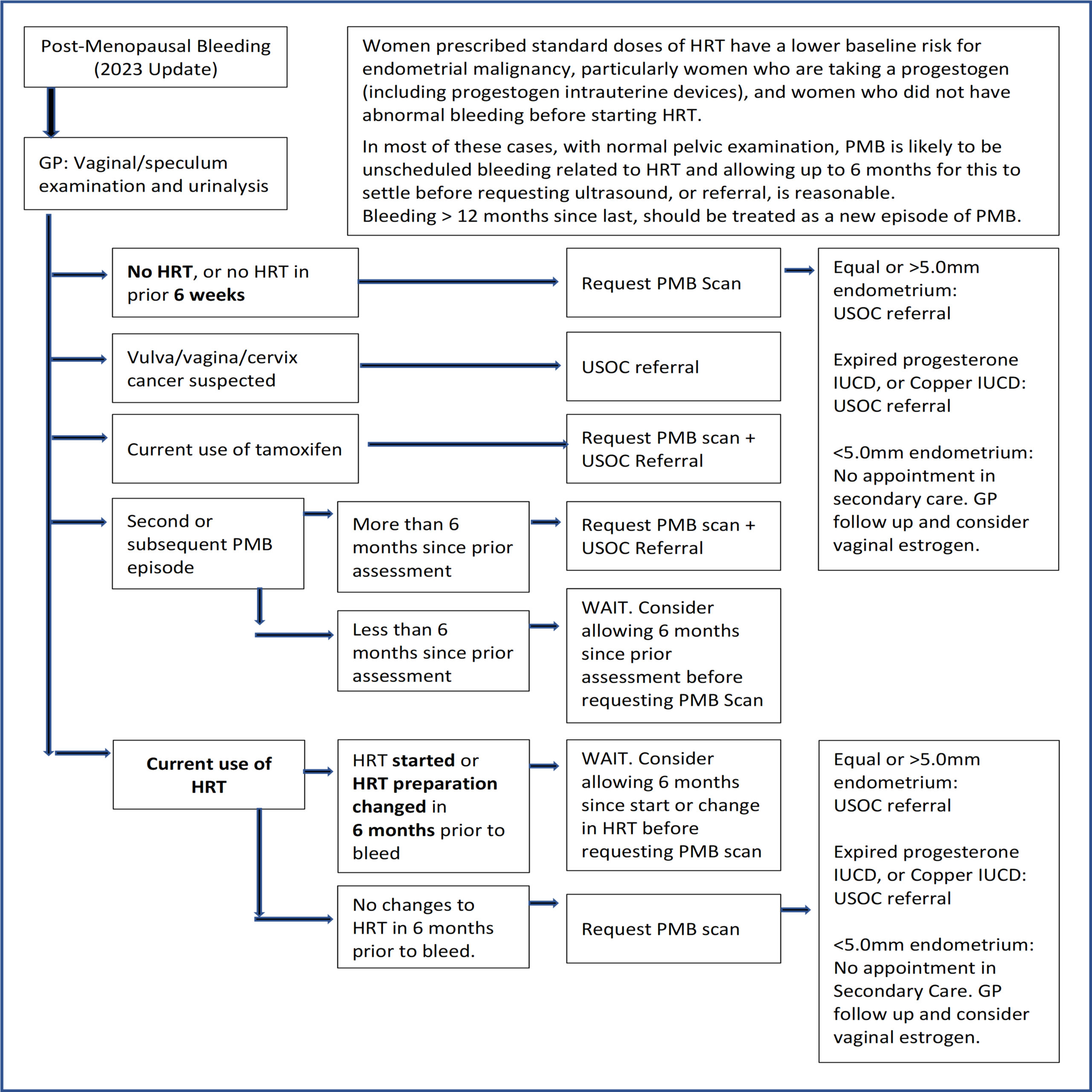
Prescription Solutions for Chronic Cases
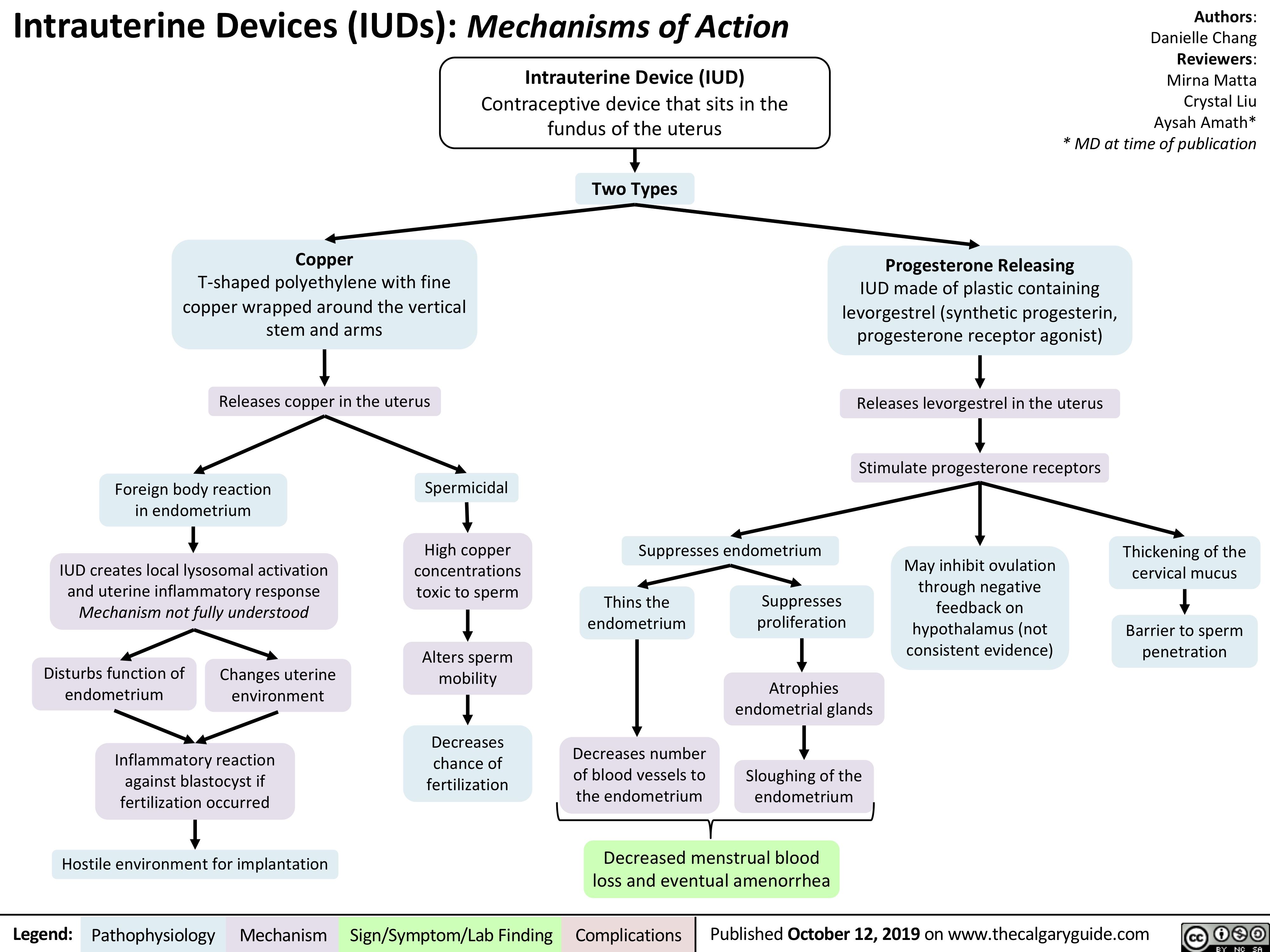
Hormonal therapies target root causes by regulating cycles:
– Hormonal IUDs: Release localized progestin to thin uterine lining, reducing contractions
– Combined oral contraceptives: Stabilize hormone fluctuations triggering uterine spasms
– GnRH analogues: Create temporary medical menopause for severe endometriosis
These treatments require 3-6 months for full effect but significantly reduce post-period back pain in 70% of users.
Pelvic Floor Physical Therapy Protocol
Specialized physical therapists address the muscle dysfunction linking your uterus and back:
– Transverse abdominis activation: 10-second holds, 15 repetitions daily
– Kegels with release: Squeeze pelvic floor for 5 seconds, fully relax for 10 seconds (3 sets daily)
– Diaphragmatic breathing: 5 minutes twice daily to reduce protective muscle guarding
Most women see improvement within 8 sessions when combined with posture correction exercises.
When to Seek Emergency Medical Care
Visit the ER immediately if you experience:
– Back pain unrelieved by 600mg ibuprofen within 1 hour
– Fever above 101°F (38.3°C) with pelvic pressure
– Dizziness or shoulder pain alongside menstrual symptoms
– Heavy bleeding soaking more than one pad hourly
– Leg weakness or numbness with your back pain
These indicate possible ectopic pregnancy, ruptured cyst, or severe pelvic infection requiring urgent intervention. Don’t wait—these conditions can become life-threatening within hours.
Long-Term Prevention Strategies
Core Strengthening Routine to Stop Pain Cycles
Build back resilience with:
– Daily planks: Start with 20-second holds, build to 60 seconds (3 sets)
– Bird-dog exercises: Extend opposite arm/leg while on hands and knees (10 reps/side)
– Swimming: 30 minutes 3x weekly to support spine without joint stress
Consistent core work prevents the protective hunching that turns temporary period pain into chronic back issues.
Symptom Tracking for Personalized Treatment
Use period-tracking apps to log:
– Pain location/intensity (0-10 scale) daily for 3 cycles
– Associated symptoms: bloating, fatigue, bowel changes
– Relief methods tried and effectiveness
This data helps your doctor distinguish between endometriosis, adenomyosis, or musculoskeletal causes—critical for targeted treatment.
Realistic Recovery Timeline
Most women achieve significant reduction in post-period back pain within 3-6 months of consistent treatment. Those addressing symptoms within six months of onset report 80% improvement versus 40% in those delaying care. Success depends on early diagnosis, daily core exercises, and hormonal management when indicated. Don’t accept monthly back pain as inevitable—your body responds dramatically to the right interventions.
Persistent back pain after your period ends signals treatable conditions, not normal cycle variations. By matching your symptoms to specific causes and implementing these targeted strategies, you can break the cycle of monthly discomfort. Start with heat therapy and pelvic tilts today, but seek medical evaluation if pain disrupts daily activities for more than two consecutive cycles—relief is possible with precise diagnosis and consistent care.