That familiar ache crawling across your lower back right before your period isn’t just “part of being a woman”—it’s your body signaling real, treatable inflammation. Up to 90% of women experience terrible back pain with period, yet most suffer in silence, assuming it’s inevitable. This guide breaks down why your back rebels during menstruation and delivers proven strategies to reclaim those days from pain. You’ll discover how to distinguish normal discomfort from warning signs and implement targeted solutions starting today.
Why Your Lower Back Rebels During Menstruation
Your uterus becomes ground zero for a prostaglandin storm right before bleeding starts. These inflammatory chemicals trigger powerful contractions that don’t just stay localized—they create a ripple effect of pain that radiates straight to your lower back. The higher your prostaglandin levels spike, the more intense your terrible back pain with period becomes. This isn’t random suffering; it’s a biological chain reaction you can interrupt.
Primary vs Secondary Pain Triggers
Primary dysmenorrhea begins at menarche and involves no structural problems—just overly enthusiastic uterine contractions. Pain peaks days 1-2 of bleeding and fades as prostaglandin levels drop naturally. If your back pain follows this pattern and responds to NSAIDs, it’s likely primary.
Secondary causes signal underlying reproductive disorders. These pains feel different—deeper, more gnawing, and often persist after bleeding ends. Endometriosis, fibroids, or adenomyosis could be fueling your terrible back pain with period. Key indicators include pain worsening before your period starts or continuing beyond day 5.
Endometriosis-Specific Back Pain Patterns
Endometrial tissue growing outside your uterus inflames pelvic nerves and ligaments. The resulting back pain feels distinct—more constant and pressure-like than typical cramps. Women report it “doesn’t ease with heat or NSAIDs” and may shoot down legs. If your terrible back pain with period lasts longer than your bleeding or occurs mid-cycle, discuss endometriosis screening with your doctor.
Decode Your Pain Pattern Like a Specialist
Understanding your specific pain signature guides targeted treatment. Track these details for three cycles to identify your triggers:
Location mapping: Mark whether pain stays midline lower back, radiates to sacrum/hips, or shoots down legs. Midline pain suggests uterine contractions; radiating pain may indicate nerve involvement from endometriosis.
Timing clues: Note when pain starts relative to bleeding. Starting 1-2 days before flow points to prostaglandin spikes. Beginning 7-10 days earlier suggests PMS-related fluid retention and muscle tension.
Quality descriptors: Use specific words—aching, cramping, gnawing, or pressure. Muscular tension feels “aching,” while nerve inflammation feels “sharp” or “gnawing.” This precision helps your doctor pinpoint solutions.
Immediate Relief Strategies That Deliver Results

Heat Therapy Protocol
Apply heat within 20 minutes of pain onset for maximum effectiveness. Use a heating pad set to medium (not high) for 20-minute sessions, 3-4 times daily during peak pain days. Pro tip: Layer a warm towel over the pad to distribute heat evenly. For work situations, adhesive heat patches provide discreet relief without restricting movement.
NSAID Timing Secrets
Start NSAIDs 1-2 days before expected bleeding if your cycle is predictable. This blocks prostaglandin production before it ramps up. Effective dosing: ibuprofen 400-600mg every 6-8 hours, or naproxen 220-440mg every 8-12 hours. Critical warning: Always take with food to prevent stomach irritation. If NSAIDs fail after three cycles, consult your doctor—your terrible back pain with period may need hormonal intervention.
Quick Stretch Routine
Perform these 5-minute moves every 2-3 hours during heavy pain days:
- Cat-cow: On hands and knees, arch and round spine slowly 10 times
- Child’s pose: Hold 30-60 seconds, breathing deeply into lower back
- Seated spinal twist: Gentle rotation left/right while seated (30 seconds each side)
These stretches reduce muscle tension and improve blood flow to inflamed areas within minutes.
Hormonal Solutions for Chronic Sufferers
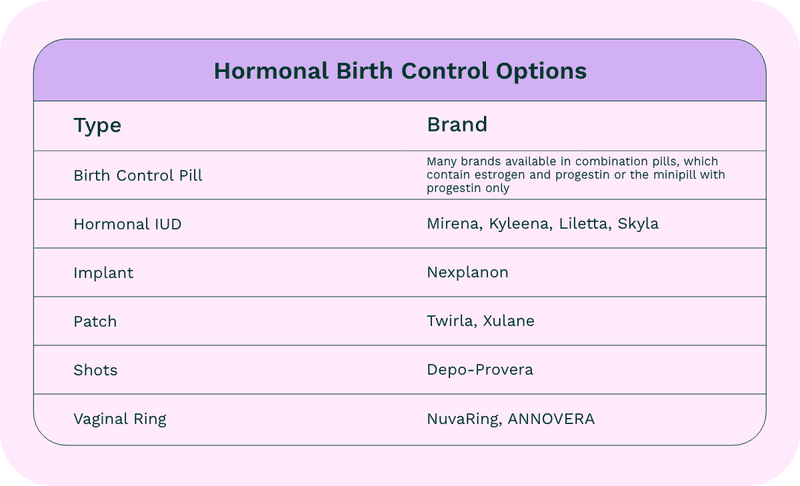
Birth Control That Targets Back Pain
Combined oral contraceptives thin the uterine lining, reducing prostaglandin production by 60-80%. Many women see significant back pain reduction within 2-3 cycles. Key insight: The levonorgestrel IUD offers longer-term relief—reducing menstrual flow and associated back pain for 3-5 years without daily pill management.
GnRH Agonists for Severe Cases
For endometriosis-related terrible back pain with period unresponsive to other treatments, short-term GnRH agonists provide temporary ovarian suppression. These eliminate periods entirely for 3-6 months, giving inflamed tissues time to heal. Important: Use requires careful monitoring due to bone density concerns—never self-prescribe.
Lifestyle Modifications That Reduce Monthly Suffering
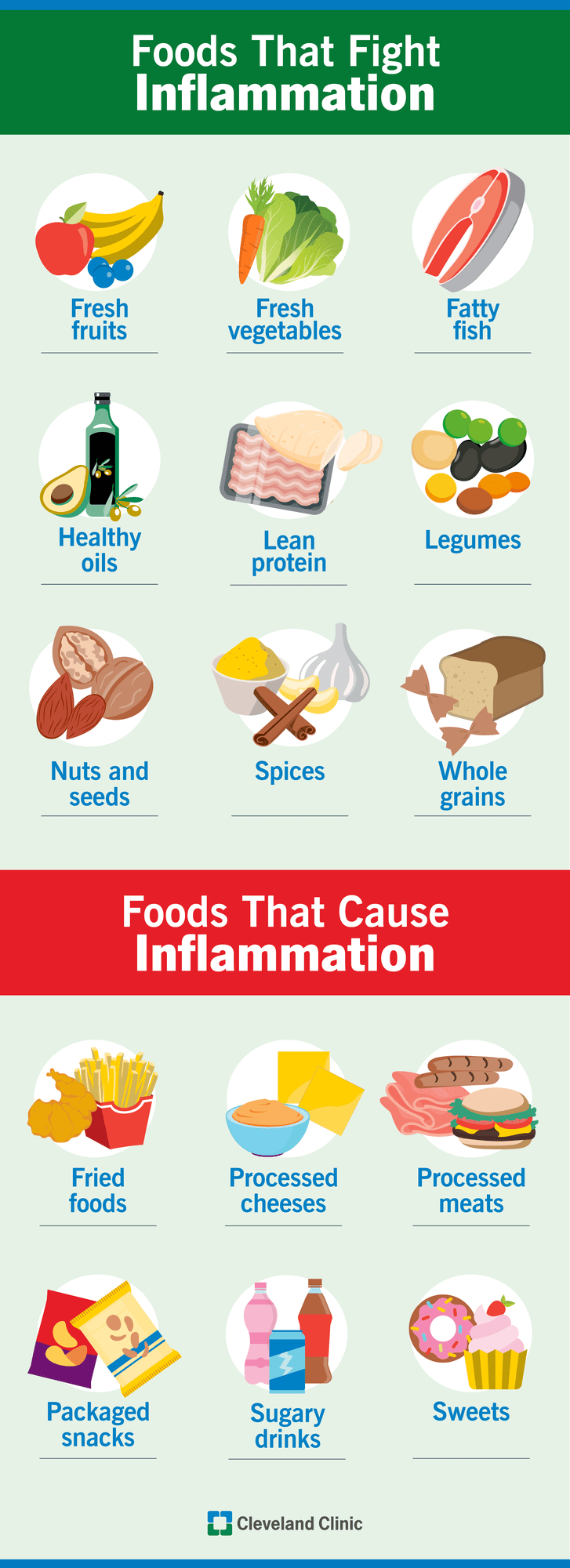
Anti-Inflammatory Diet Plan
Increase: Omega-3 rich foods (salmon, walnuts), leafy greens, berries, calcium-rich dairy
Decrease: Processed foods, caffeine, alcohol, high-salt items that increase inflammation
Supplement strategy: Magnesium 310-360mg daily reduces muscle tension. Vitamin D 15-20mcg supports pain modulation. Start 2 weeks before expected period for best results—this isn’t instant relief but builds resilience over cycles.
Exercise Timing Strategy
Avoid high-impact exercise during peak pain days (typically days 1-2). Instead, focus on gentle movement—walking, swimming, or restorative yoga. Game-changer: Resume normal workouts day 3-4 when prostaglandin levels drop. Build baseline fitness with 150 minutes of weekly aerobic exercise—it reduces overall dysmenorrhea incidence by 25-30%.
When to Seek Emergency Help
Call your doctor immediately if you experience:
– Pain so severe you vomit or faint
– Numbness/tingling in legs or feet
– Loss of bladder/bowel control
– Fever with back pain
– Pain lasting longer than 10 days
These red flags may indicate ectopic pregnancy, severe infection, or nerve compression requiring urgent intervention. Don’t dismiss “just period pain” when these symptoms appear.
Build Your Period Pain Survival Kit
Prepare a “go bag” for painful days:
- Medications: Pre-counted NSAID doses in labeled baggies, acetaminophen backup
- Heat relief: Portable USB heating pad (fits in purse) or adhesive patches
- Hydration: Electrolyte packets to mix with water—dehydration worsens cramps
- Comfort: Lumbar support pillow and loose waistband clothing
- Documentation: Pain scale cards (0-10) for quick tracking during appointments
Keep this kit stocked in your desk, car, and bathroom—accessibility prevents suffering through preventable pain.
Long-Term Outlook and Prevention
Primary dysmenorrhea often improves after childbirth and naturally decreases approaching menopause. Secondary causes like endometriosis require ongoing management but become highly controllable. Most women using combined strategies reduce back pain by 50-80% within 6 months. Track your patterns consistently—your body’s signals hold the key to personalized relief.
Key takeaway: Your terrible back pain with period isn’t inevitable suffering—it’s treatable inflammation. Start with immediate heat and NSAID protocols while building long-term solutions through diet and hormonal management. If conservative measures fail after three cycles, or if red flag symptoms appear, schedule a gynecological evaluation immediately. With the right approach, you can transform period days from agony to manageable—and possibly pain-free—experiences.
Final reminder: While 90% of period back pain stems from benign causes, persistent or worsening symptoms deserve medical evaluation. Track your pain patterns for three cycles, then bring your symptom diary to your appointment—it provides crucial data for accurate diagnosis. Your relief journey starts with recognizing that severe back pain during periods isn’t normal, and you deserve solutions.

