That familiar dull ache in your lower back signaling your period’s arrival isn’t just in your head—it’s a monthly reality for nearly half of all menstruating people. When this pain strikes, simple tasks like sitting through meetings or bending to tie your shoes can become exhausting challenges. The good news? You don’t have to resign yourself to suffering. This guide delivers immediate, actionable solutions to relieve menstrual back pain effectively, backed by medical research and physical therapy expertise. Within minutes, you’ll discover practical techniques to reduce that throbbing discomfort without relying solely on medication.
Menstrual back pain typically starts 1-2 days before your period and lasts through the first few days of bleeding. Understanding why it happens is your first step toward relief. Your body releases prostaglandins—chemical messengers that trigger uterine contractions to shed the lining. When levels spike, these contractions intensify and radiate pain into your lower back. Compounding this, fluid retention creates extra pressure on your spine, while hormonal shifts subtly alter your posture. This perfect storm turns what should be routine days into a battle against discomfort. But armed with the right strategies, you can disrupt this cycle starting today.
Why Your Dyson V7 Brush Suddenly Stops Spinning
Why Your Back Hurts During Periods
Your body produces prostaglandins—chemical messengers that trigger uterine contractions to shed its lining. When these levels spike, the contractions intensify and the pain radiates outward, creating that familiar lower back ache. Fluid retention adds extra pressure, while hormonal shifts can alter your posture, creating a perfect storm of discomfort that typically starts a few days before your period and lasts for one to two days.
Immediate Pain Relief Methods
Heat Therapy That Works
Apply heat directly to your lower back using a heating pad, hot water bottle, or warm bath. The heat relaxes tense muscles and improves blood flow, providing relief within minutes. Use as needed throughout the day, especially when pain peaks.
Over-the-Counter Medications
NSAIDs like ibuprofen or naproxen reduce prostaglandin production and inflammation. Start taking them a day or two before your period begins for maximum effectiveness. Acetaminophen works as an alternative if you can’t take NSAIDs, but it won’t address the prostaglandin issue directly.
Quick Movement Fix
Avoid prolonged sitting during your period. Even gentle walking improves circulation and reduces muscle tension. Stand up and stretch every 30-60 minutes if you have a desk job.
Essential Stretches for Period Back Pain
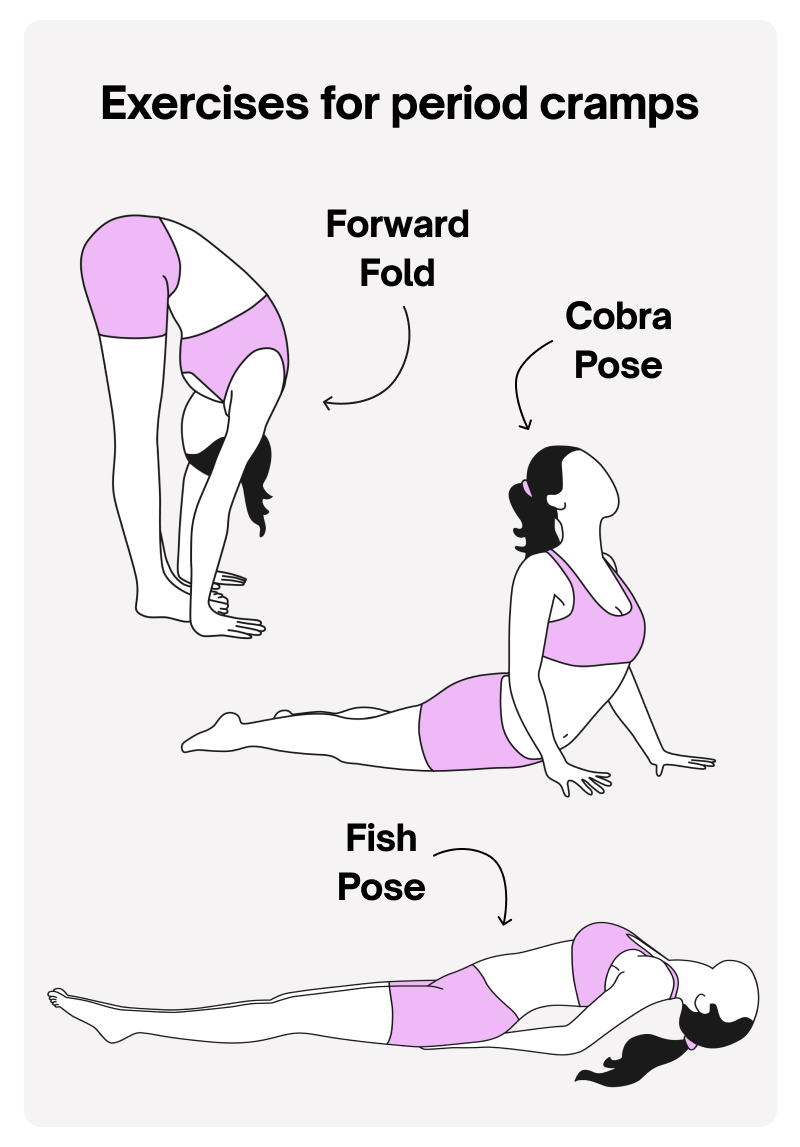
Cat-Cow Stretch
Start on hands and knees. Inhale while arching your back (lifting head and tailbone), exhale while rounding your spine (tucking chin and pelvis). Perform 5-10 slow repetitions to release spinal tension.
Child’s Pose
Kneel with toes touching and knees apart. Sit back on your heels and stretch your arms forward, lowering your torso between your thighs. Hold for 30 seconds to 1 minute to gently stretch your lower back.
Supine Twist
Lie on your back, hug knees to chest. Lower both knees to one side while keeping shoulders grounded. Hold as long as feels beneficial, then switch sides. Use a pillow under your knees if needed.
Supported Bridge
Lie on your back with feet flat on the floor. Lift your hips and place a yoga block or stacked pillows underneath for support. Stay as long as comfortable, then lower slowly.
Dead Bug Pose
Lie on your back, extending arms and legs toward the ceiling. This gentle spinal traction helps decompress your lower back. Rotate wrists and ankles while holding the position.
Professional Treatment Options
When to See a Doctor
Seek immediate medical attention if you experience:
– Pain lasting longer than 10 days
– Numbness or tingling in legs or feet
– Weakness in legs or feet
– Loss of bladder control
– Fever accompanying back pain
– Pain persisting beyond your menstrual cycle
Prescription Solutions
Birth control pills containing estrogen and progestin can significantly reduce prostaglandin production. Progesterone therapy offers another hormonal approach. For endometriosis-related pain, gonadotropin-releasing hormone agonists may be prescribed.
Virtual Physical Therapy
Programs like Hinge Health provide personalized exercise plans and expert guidance tailored specifically to menstrual back pain, making professional help accessible from home.
Prevention Strategies That Work
Pre-Period Preparation
Start taking NSAIDs two days before your expected period. Begin your stretching routine preemptively rather than waiting for pain to strike. Track symptoms in a diary to identify your personal patterns and triggers.
Long-Term Lifestyle Changes
Exercise regularly—research shows women who maintain consistent fitness routines experience less painful periods. Focus on activities you enjoy, whether that’s walking, swimming, or yoga. Stay hydrated to reduce bloating and cramping. Maintain a balanced diet rich in vitamin B and magnesium throughout your cycle, not just during your period.
Red Flag Conditions
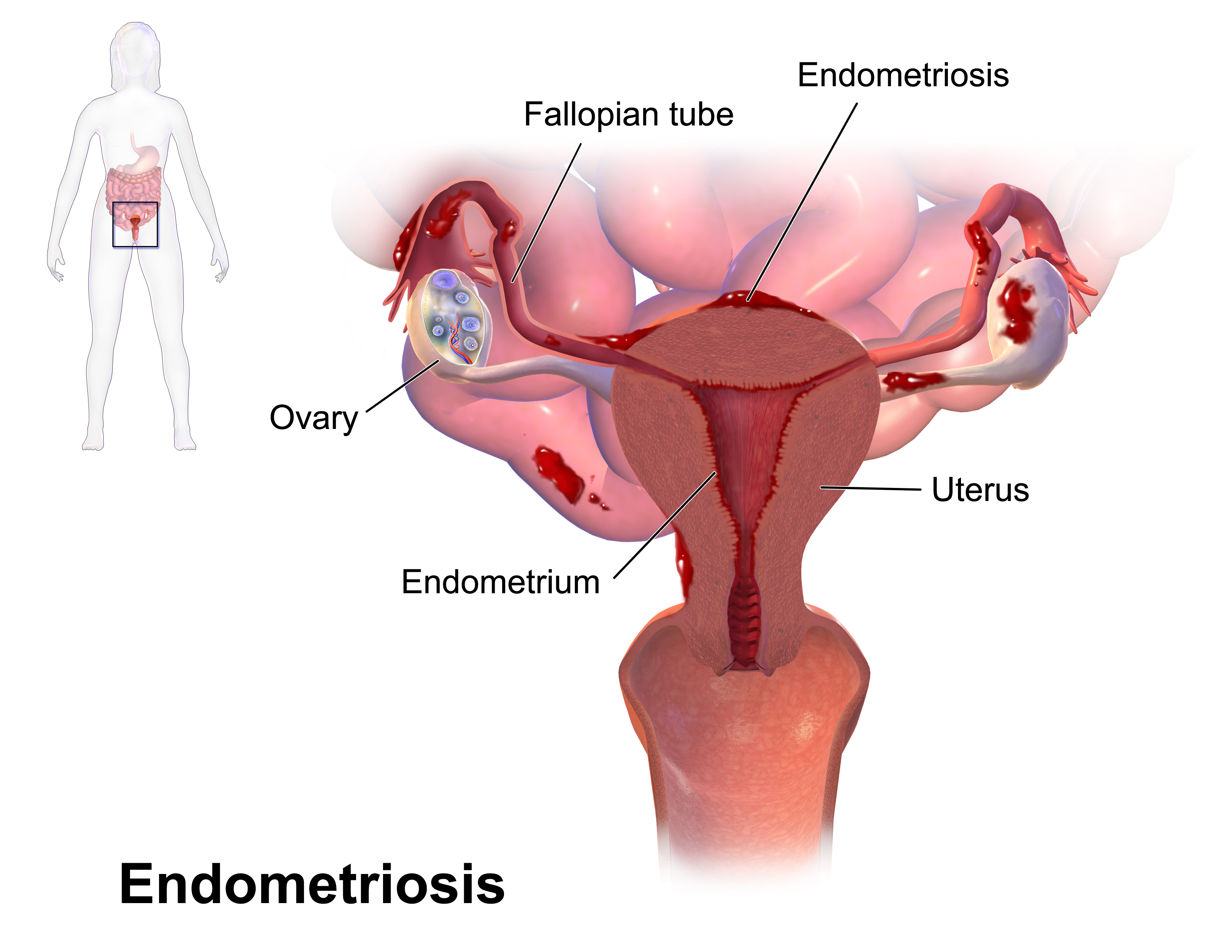
Endometriosis Warning Signs
Tissue similar to uterine lining growing outside the uterus often causes severe lower back pain during menstruation. Watch for additional symptoms or unusually intense pain that worsens over time.
Fibroid Factors
These non-cancerous uterine growths can create back pressure during periods. If your pain seems to intensify with age or includes heavy bleeding, consult your doctor.
Infection Indicators
Pelvic Inflammatory Disease (PID), often from STIs or tampon use, causes lower back pain with additional discomfort. This requires immediate medical treatment.
Exercise Modifications for Period Days

Listen to Your Body
Stop any movement causing sharp pain. Focus on slow, mindful stretches rather than intense workouts. Use gentler variations of your usual exercises. If Child’s Pose feels too intense, try lying flat on your back instead.
Supported Restorative Poses
Supported Reclined Butterfly: Sit with soles of feet together, using pillows under knees and a bolster along your spine. This releases tension in your glutes while supporting your lower back.
Simple Lying Down: Lie on a firm surface with arms and legs slightly spread. Add soft lighting and calming music to reduce period-related anxiety while your back decompresses naturally.
Diet and Supplement Guide
Hydration Strategy
Drink water consistently throughout the day, not just when you feel thirsty. Proper hydration reduces muscle cramping and stiffness. Add electrolytes if you’re experiencing significant bloating.
Supplement Support
Magnesium helps reduce muscle tension and cramping. Vitamin B complex supports nerve function and may decrease pain perception. Start these supplements consistently, not just during your period, for best results.
Age-Related Changes
Your menstrual back pain won’t necessarily worsen with age. Some people experience reduced discomfort as they approach menopause, while others develop increased pain due to conditions like endometriosis or fibroids. Track your patterns to understand your body’s unique trajectory.
Differentiating Pain Types
Lower back pain dominates menstrual discomfort, but upper back pain can also occur from referred abdominal pain. Distinguish menstrual pain from other causes by noting its cyclical pattern—if it consistently appears 1-2 days before your period and subsides afterward, it’s likely menstrual-related.
Quick Reference Action Plan
Day 1-2 Before Period: Start NSAIDs, begin gentle stretching routine, increase water intake
Day 1-3 of Period: Apply heat therapy, continue stretches, modify activities as needed
Ongoing: Maintain regular exercise, track symptoms, adjust prevention strategies based on patterns
Remember, menstrual back pain is common but not inevitable. With the right combination of immediate relief techniques and long-term prevention strategies, you can significantly reduce or even eliminate this monthly discomfort. Start with the simplest solutions—heat and gentle movement—and build your personalized toolkit from there.

