That deep throb in your lower back arriving like clockwork each month isn’t “just part of being a woman”—it’s a physiological response affecting 72% of women with period pain. While often dismissed as normal, understanding why back pain from menstrual cycles strikes can transform your relief strategy. This isn’t merely referred uterine cramping; it’s a complex interplay of chemicals, hormones, and pressure that can range from annoying stiffness to pain forcing you to cancel plans. The good news? Most cases respond dramatically to targeted interventions once you know the triggers.
Your back pain from menstrual symptoms typically start 1-2 days before bleeding, peak during heavy flow days, and fade as your period ends. But when it crosses from uncomfortable to debilitating—keeping you home from work or doubling you over mid-task—it’s time to move beyond “toughing it out.” By identifying whether your pain stems from normal prostaglandin surges or signals something more serious, you’ll unlock faster relief and prevent years of unnecessary suffering.
Why Your Lower Back Aches During Periods
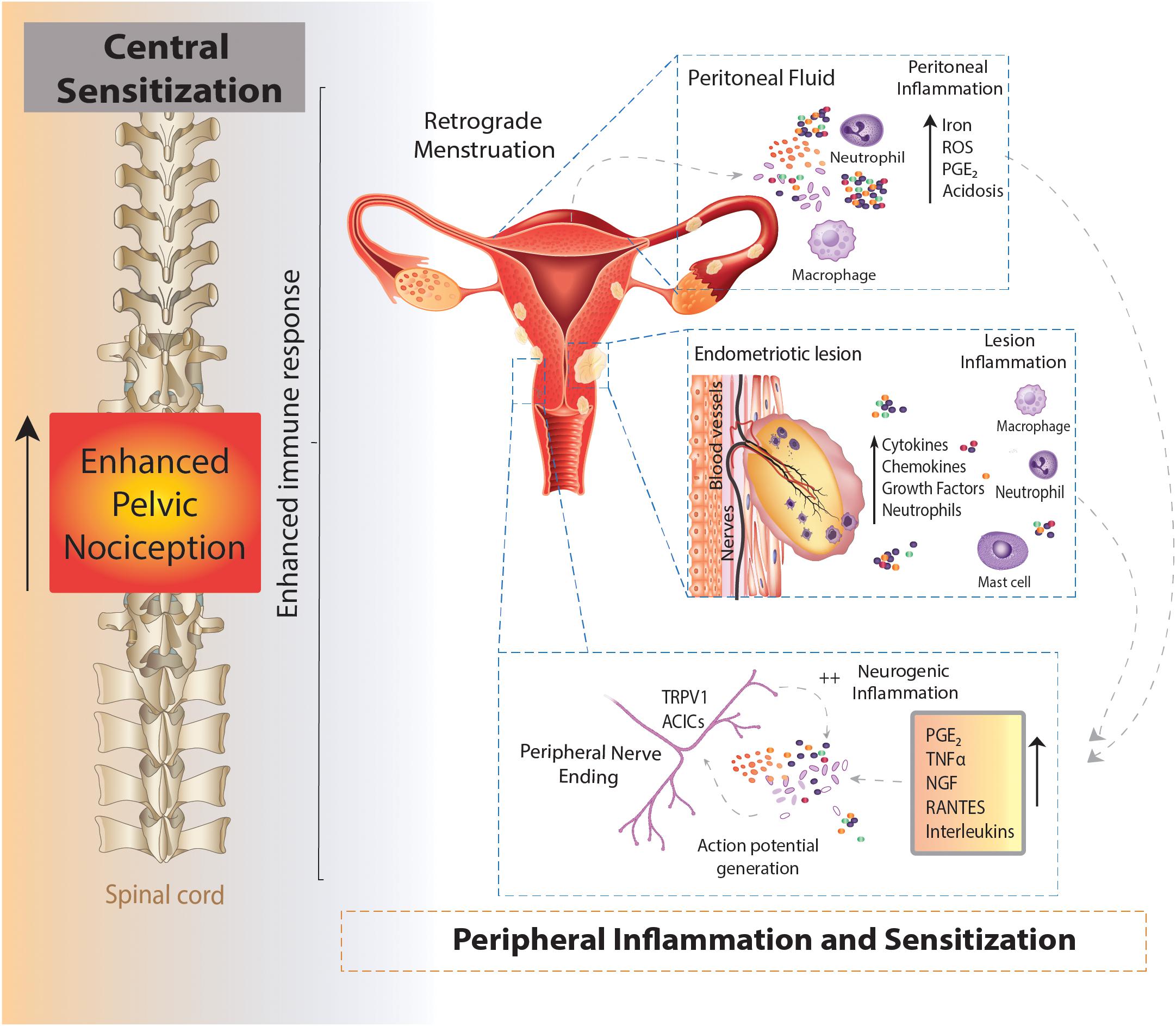
Prostaglandins Trigger Spinal Muscle Spasms
Your uterus releases prostaglandins—chemicals that contract uterine muscles to shed its lining. When levels spike too high, these contractions intensify and pain radiates backward through shared nerve pathways. This isn’t imagination; it’s a biochemical domino effect where uterine spasms create tension in your lower back muscles. Women with high prostaglandin levels often describe a deep, constant ache that worsens with movement, peaking during heaviest flow days. These chemicals also heighten pelvic sensitivity, turning minor strains into significant discomfort.
Hormonal Shifts Destabilize Your Spine
As estrogen and progesterone plummet before your period, collagen production drops throughout your body—including spinal ligaments. This temporary laxity makes your lower back feel unstable, similar to pregnancy-related joint looseness but compressed into days. The result? Ligaments that normally support your spine become less effective, forcing back muscles to overcompensate. This explains why simple actions like bending to tie shoes suddenly trigger sharp pain during your cycle.
Pelvic Congestion Pressures Nerves
Your uterus swells during menstruation, creating pelvic “traffic jams” that push against surrounding structures. This congestion directly impacts the sacral nerves at your spine’s base, causing a heavy, dragging sensation that worsens when standing. Inflammation from this pressure makes every movement feel like grinding. Unlike typical cramps, this back pain from menstrual congestion often radiates upward along your spine and intensifies with prolonged sitting or standing.
Primary vs. Secondary Dysmenorrhea: Spot the Difference
Typical Menstrual Back Pain Patterns
Primary dysmenorrhea starts soon after your first period and follows predictable rhythms. Your back aches 1-2 days before bleeding begins, peaks during the first 48 hours, then fades as flow decreases. Pain feels like deep muscle cramping centered above your tailbone, sometimes radiating to hips. Crucially, over-the-counter NSAIDs and heat provide noticeable relief within 30-60 minutes. While uncomfortable, it rarely stops you from light activities once managed. This type affects 95% of women with period pain but becomes manageable with targeted strategies.
Red Flags for Serious Underlying Conditions
Secondary dysmenorrhea behaves differently—and dangerously. Pain starts mid-cycle or persists beyond your period, intensifies yearly, or feels sharp/stabbing rather than crampy. If your back pain from menstrual cycles includes any of these, seek evaluation:
– Pain lasting >2 days after bleeding stops
– Numbness/tingling in legs or feet
– Worsening pain during bowel movements
– Painful intercourse unrelated to your cycle
Endometriosis often causes knife-like back pain from spinal lesions, while fibroids create constant pressure as if “someone sits on your lower back.” These conditions require medical intervention, not just painkillers.
Immediate Back Pain Relief During Your Period

Heat Therapy That Works in Minutes
Apply heat at the first twinge—not when pain becomes severe. Place a heating pad on medium setting directly over your lower back for 15-20 minutes. Heat reduces prostaglandin production by 30% and relaxes tense muscles within minutes. For mobile relief, use disposable heat patches in your waistband. Pro tip: Combine heat with gentle movement—while lying on the pad, slowly rock knees side-to-side to boost pelvic blood flow.
3 Stretches for Instant Spinal Release
1. Cat-Cow Flow: On hands and knees, inhale while dropping belly (cow), exhale while rounding spine upward (cat). Repeat 10x slowly. Visual cue: Feel vertebrae move individually like a caterpillar.
2. Supported Child’s Pose: Knees wide, big toes touching, sit back on heels while resting forehead on stacked hands. Hold 2 minutes. Visual cue: Notice lower back softening with each exhale.
3. Pelvic Tilts: Lie knees bent, flatten lower back against floor by tightening abs. Hold 5 seconds, release. Repeat 15x. Visual cue: Imagine pressing a coin into the floor with your spine.
Medication Timing Secrets
Take NSAIDs like ibuprofen before pain peaks—ideally 1-2 days pre-period. This blocks prostaglandin production rather than fighting existing pain. Standard dose (400mg) works for most, but if ineffective, consult your doctor about prescription-strength options. Critical mistake: Waiting until you’re doubled over. Once prostaglandins flood your system, medication becomes 40% less effective. Never exceed 1,200mg daily without medical supervision.
When Back Pain Means See a Doctor Now
Emergency Warning Signs
Seek immediate care if back pain from menstrual cycles includes:
– Loss of bladder/bowel control (spinal nerve emergency)
– Fever >101°F with pelvic pain (possible infection)
– Leg weakness or foot numbness
– Pain lasting >10 days post-period
– Vomiting/fainting from pain intensity
These signal conditions like spinal endometriosis, pelvic inflammatory disease, or nerve compression requiring urgent intervention. Don’t dismiss severe symptoms as “bad cramps”—early treatment prevents permanent damage.
What Your Doctor Will Check
Your provider will start with a pelvic exam to check for uterine tenderness or abnormalities. An ultrasound can detect fibroids or adenomyosis, while MRI identifies endometriosis lesions. For persistent cases, laparoscopy (minimally invasive surgery) both diagnoses and treats conditions like endometriosis. Key insight: Track symptoms for 2-3 cycles first—note when pain starts relative to bleeding, what worsens it, and what relieves it. This data helps pinpoint causes faster.
Long-Term Prevention Strategies That Work
Pre-Period Proactive Care
Start prevention 3-5 days before your expected period:
– Take magnesium glycinate (200-400mg daily) to reduce muscle tension
– Begin NSAIDs 48 hours pre-bleeding
– Swap caffeine/alcohol for ginger tea (natural anti-inflammatory)
– Do 10 minutes of walking daily to boost circulation
Cycle-Specific Lifestyle Tweaks
Adjust habits weekly based on your cycle phase:
– PMS week: Avoid high-salt foods to reduce pelvic pressure
– Period week: Sleep with pillow between knees to maintain spinal alignment
– Ovulation week: Strengthen core with planks to support spine year-round
Document what works in a symptom tracker app—patterns reveal personalized solutions within 2-3 cycles.
Your back pain from menstrual cycles doesn’t have to dictate your monthly rhythm. By targeting prostaglandin surges with preemptive heat and NSAIDs, recognizing red flags for secondary conditions, and implementing cycle-specific prevention, most women achieve 70-90% pain reduction. Remember: while common, debilitating back pain isn’t “normal.” If conservative measures fail after 2-3 cycles, seek specialized care—today’s treatments for endometriosis, fibroids, and hormonal imbalances offer real relief. Start tracking your symptoms now, implement one immediate relief strategy during your next period, and reclaim your month. Your future self will thank you for refusing to accept preventable pain as the price of having a period.