That persistent ache in your lower back might not be from your new mattress or weekend gardening. When you’re constipated with back pain, it’s often because hardened stool pressing against your spine is irritating the sacral nerves that control both bowel function and lower back sensation. This uncomfortable duo affects millions yet most people treat them as separate issues, wasting precious time on ineffective remedies. If you’ve had fewer than three bowel movements this week alongside nagging lower back discomfort that eases after bathroom visits, you’re likely trapped in this painful cycle.
The connection is straightforward: backed-up stool swells your colon, creating outward pressure that radiates to surrounding structures including your spine. Unlike muscular back pain, this discomfort typically improves immediately after successful bowel movements. The good news? Targeted interventions can break this cycle within days. This guide delivers the exact steps to relieve both symptoms simultaneously while preventing future episodes.
How Hardened Stool Creates Lower Back Pressure
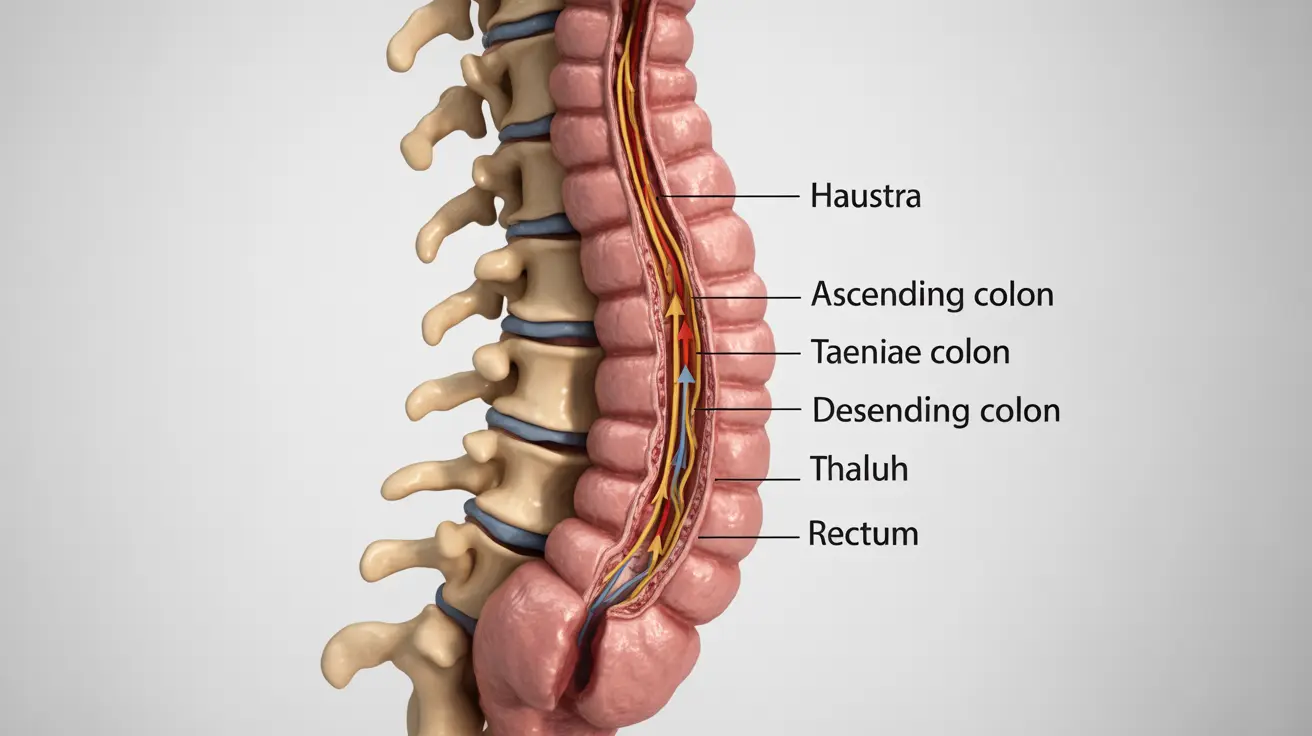
When stool remains in your colon longer than normal, it absorbs excess water and hardens. This creates physical pressure that expands your intestines outward, compressing nearby nerves and muscles. The sacral nerves running through your lower spine become irritated by this pressure, translating to that familiar dull ache. Most people notice this pain worsens after meals when digestion increases intestinal activity.
Fecal Impaction Emergency Signals
A large mass of dried stool becoming critically stuck in your rectum creates extreme pressure that often triggers intense lower back pain radiating down your legs. Watch for these warning signs requiring immediate medical attention:
– Swollen, tender abdomen
– Little to no urine output despite drinking fluids
– Dizziness or lightheadedness when standing
– Fever above 100.4°F (38°C)
– Inability to pass gas for 48+ hours
Why Your Back Hurts When You Strain
The act of straining during constipation overexerts your core and back muscles, creating secondary muscle tension. This explains why many people feel back pain specifically during bathroom attempts. The combination of nerve pressure from backed-up stool and muscle strain from pushing creates a double whammy of discomfort that won’t resolve until both issues are addressed.
Immediate Relief Strategies That Work in 24 Hours

Start with these targeted interventions that address both constipation and back pain simultaneously. The key is combining hydration, specific foods, and movement patterns proven to stimulate bowel activity while relieving nerve pressure.
Targeted Morning Protocol for Same-Day Relief
Within 60 minutes of waking:
– Drink 16 oz warm water with lemon (triggers gastrocolic reflex)
– Consume 3-4 dried prunes or ½ cup prune juice (sorbitol draws water into stool)
– Perform 5 minutes of knee-to-chest stretches (relieves nerve pressure)
Within 2 hours of breakfast:
– Eat fiber-rich meal (oatmeal with berries and flaxseed)
– Take 15-minute walk (stimulates intestinal contractions)
– Try child’s pose yoga stretch for 2 minutes (gently compresses abdomen)
Critical Hydration Formula
Most people don’t realize they’re dehydrated when constipated with back pain. Increase your water intake to 3-4 liters daily using this schedule:
– 16 oz upon waking
– 8 oz before each meal
– 4 oz every hour between meals
– Add electrolytes if experiencing nausea
Skip cold water—warm or room temperature fluids move through your system more efficiently when you’re constipated with back pain.
Red Flags That Demand Immediate Medical Attention
While most constipation-related back pain resolves with home treatment, certain symptoms indicate potentially dangerous conditions. These require urgent evaluation:
Danger Sign Combination Checklist
Seek ER care immediately if you have:
– Back pain with loss of bowel or bladder control
– Inability to pass gas or stool for 72+ hours
– Blood in your stool alongside severe back pain
– Fever above 101°F with abdominal swelling
Schedule doctor visit within 24 hours if:
– No bowel movement for 5+ days with worsening pain
– Back pain radiating down both legs
– Unintended weight loss exceeding 5 pounds
– Nausea preventing adequate fluid intake
These symptoms could indicate bowel obstruction, spinal cord compression, or serious underlying conditions like endometriosis or colorectal cancer.
Fiber That Actually Works for Back Pain Relief
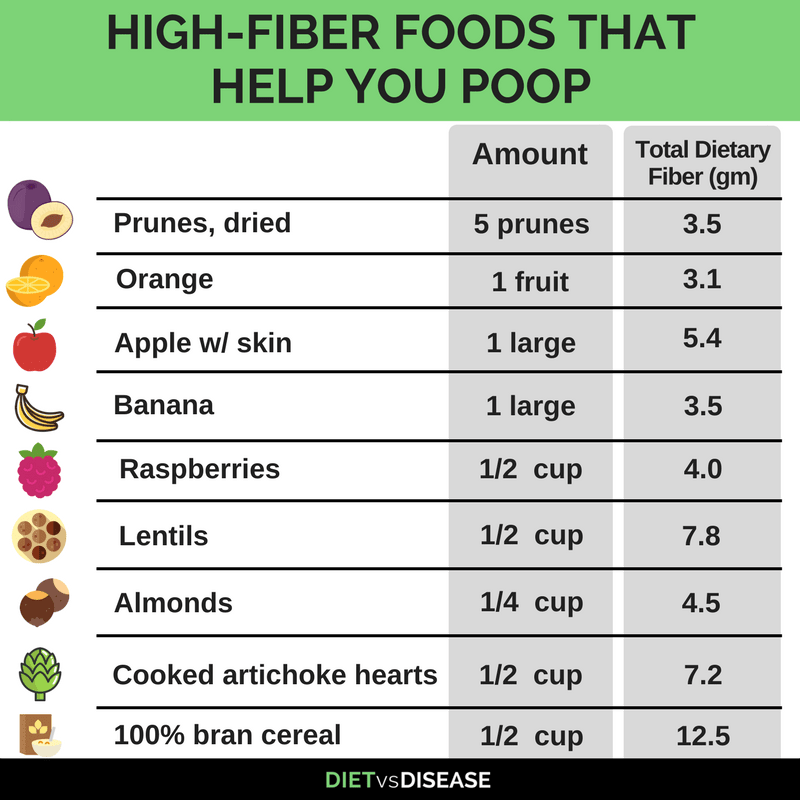
Not all fiber helps when you’re constipated with back pain. Focus on these specific sources that soften stool while reducing nerve pressure:
Most effective immediate options:
– Psyllium husk (1 tablespoon in 8 oz water)
– Ground flaxseed (2 tablespoons daily)
– Chia seeds soaked in water (forms natural gel)
– Prunes, pears, papaya (“P fruits” with natural sorbitol)
Daily fiber targets:
– Breakfast: Oatmeal with berries (8g fiber)
– Lunch: Lentil soup with whole grain bread (10g)
– Dinner: Black bean salad with avocado (12g)
– Total: 30g daily minimum
Start slowly—adding too much fiber too quickly worsens bloating and back discomfort. Increase by 5g daily until reaching target.
Movement That Unlocks Stuck Stool and Back Pain
Specific movements stimulate peristalsis (intestinal contractions) while relieving nerve compression. Try this sequence when you’re constipated with back pain:
- Pelvic tilts: Lie on back with knees bent, flatten lower back against floor 10 times
- Knee-to-chest: Hold each knee to chest for 30 seconds (releases sacral nerves)
- Walking: 10 minutes after each meal (activates digestive reflexes)
- Deep breathing: 5 minutes diaphragmatic breathing (stimulates vagus nerve)
Avoid twisting motions or heavy lifting when constipated with back pain—these can worsen impaction.
Safe Over-the-Counter Solutions Timeline
When dietary changes aren’t enough, use this medication protocol that prevents dependency while addressing both symptoms:
Days 1-2:
– Magnesium citrate (250-500mg): Draws water into colon
– Docusate sodium (stool softener): Makes stool easier to pass
– Apply heat pack to lower back for 20 minutes
Days 3-4 (if no improvement):
– Polyethylene glycol (Miralax): Osmotic laxative
– Glycerin suppository: For quick relief (15-60 minutes)
– Gentle abdominal massage in clockwise direction
Never combine: Multiple laxatives cause dehydration and electrolyte imbalance, worsening back pain.
Long-Term Prevention That Breaks the Cycle
Preventing constipation with back pain requires consistent daily habits rather than crisis management. Implement these non-negotiable routines:
Morning non-negotiables:
– 16 oz warm water upon waking
– 10-minute movement session before breakfast
– Dedicated 15-minute bathroom time after morning meal
Workday essentials:
– Hourly 2-minute movement breaks
– Visible water bottle refilled 3x daily
– Fiber-rich snacks (apples with almond butter)
Evening habits:
– 20-minute walk after dinner
– Gentle stretching before bed
– No eating 3 hours before sleep
Special Considerations for At-Risk Groups
Pregnant women: Iron supplements worsen constipation—ask about alternatives. Focus on prenatal yoga and extra hydration (10+ glasses daily).
Older adults: Age-related decreased gut motility requires proactive hydration and movement. Set phone reminders for water and walking.
Post-surgical patients: Start stool softeners before surgery. Walk as soon as medically cleared—this restarts bowel function faster than any medication.
When to Consult a Specialist
Schedule doctor visit if home treatments fail after 7 days, or sooner with any red flags. Be prepared to discuss:
- Bowel movement frequency and consistency (use Bristol Stool Chart)
- Back pain pattern (constant vs. intermittent)
- Current medications (many cause constipation)
- Dietary history and fluid intake
Your doctor may recommend blood tests, abdominal X-rays, or colonoscopy to rule out underlying conditions like endometriosis or inflammatory bowel disease.
Key Takeaway: Constipation with back pain responds dramatically to targeted interventions that address both symptoms simultaneously. Most cases improve within 3-5 days using the hydration, fiber, and movement protocols outlined here. Start with the morning relief protocol today, then build the long-term prevention habits to avoid recurrence. If symptoms persist beyond one week or include any red flags, seek medical evaluation to rule out serious underlying conditions. The connection between your gut and spine is real—treat them together for complete relief.

