That sudden wave of nausea hitting as your upper back seizes—it’s a distressing combo many women endure but rarely discuss. If you’re clutching your shoulder blades while feeling queasy after a meal or during your period, you’re not imagining it. Upper back pain and nausea female symptoms often signal underlying issues tied to your unique biology, from hormonal shifts to anatomical vulnerabilities. This isn’t just “bad digestion” or “poor posture.” For women, this pairing frequently points to conditions like gallbladder attacks, kidney infections, or even cardiac events that present differently than in men. By the end of this guide, you’ll know exactly when to seek emergency care, how to decode your symptom patterns, and which female-specific relief strategies actually work.
Gallbladder Attacks: Why Women Face Triple the Risk
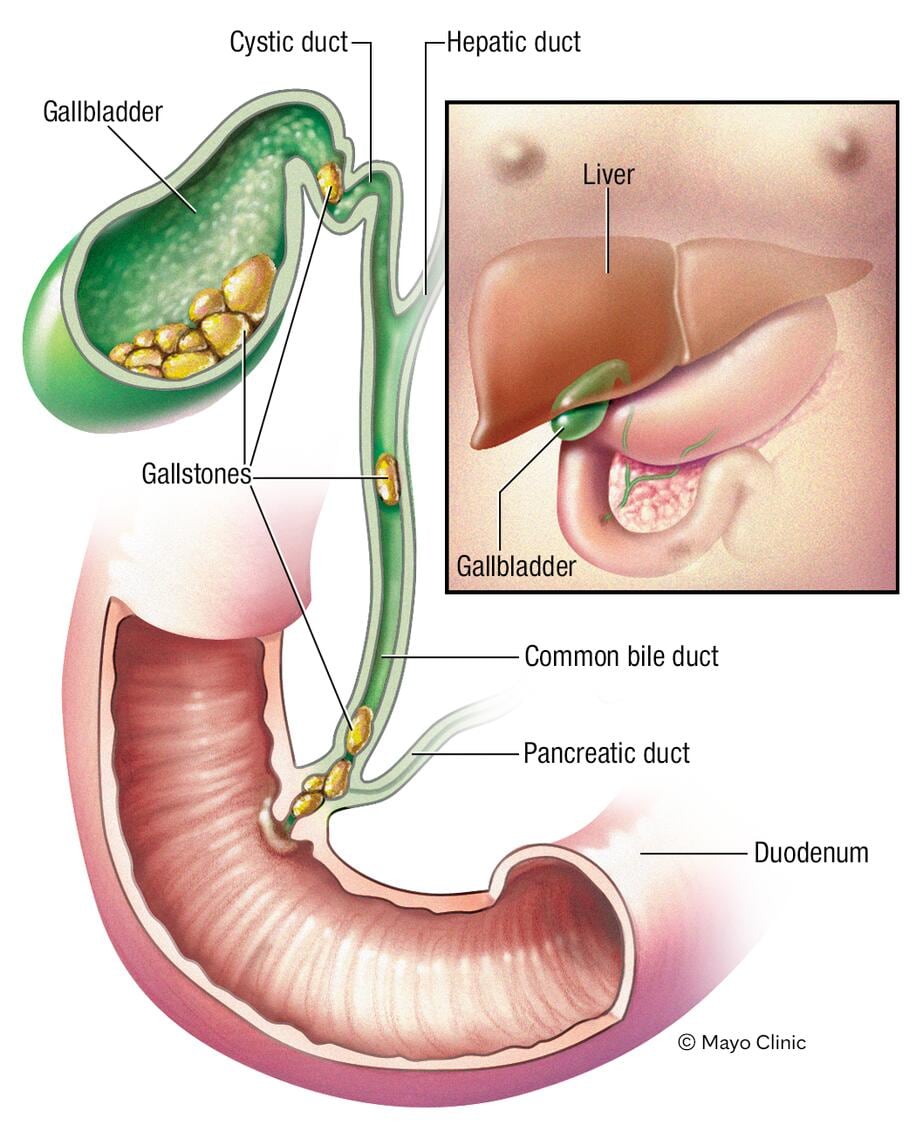
Estrogen’s role in bile production makes women three times more likely to develop gallstones, directly triggering that classic right upper back pain and nausea combo. When stones block ducts, pain radiates from under your right ribs to your shoulder blades—often worsening 30–60 minutes after fatty meals like pizza or fried foods. Nausea typically hits simultaneously, sometimes leading to vomiting that offers only temporary relief.
Spotting Gallbladder Warning Signs
Watch for these specific indicators:
– Pain that wraps around your torso like a tight band under your right ribcage
– Shoulder blade discomfort intensifying with deep breaths
– Nausea triggered exclusively after rich meals (not on an empty stomach)
– Temporary symptom relief after vomiting
Avoid the critical mistake of dismissing this as “indigestion.” Left untreated, gallstone complications can escalate rapidly. If you’re pregnant, on hormonal birth control, or in perimenopause, your risk multiplies due to estrogen fluctuations.
Pregnancy and Hormonal Shifts: Unexpected Triggers
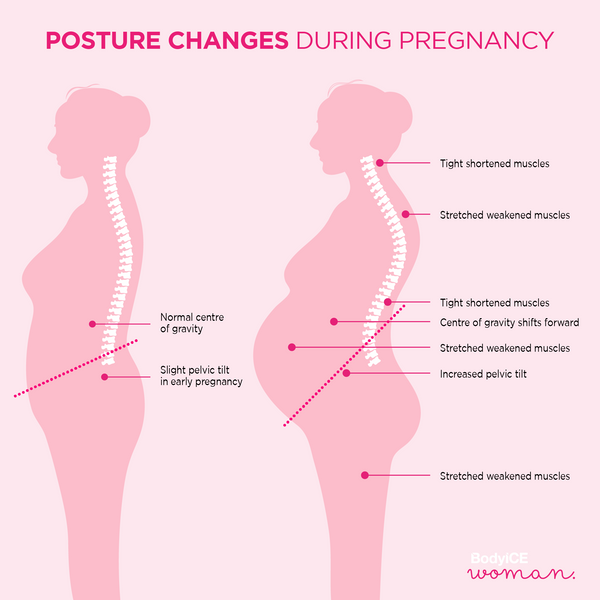
Progesterone surges during your luteal phase or early pregnancy slow digestion, causing bloating that presses against your diaphragm and strains upper back muscles. This same hormone relaxes spinal ligaments, forcing your back to compensate for shifting posture. Meanwhile, 70% of pregnant women experience morning sickness—a nausea wave that often coincides with new back discomfort as your center of gravity moves forward.
Menstrual Cycle Connections
Track these timing patterns:
– Days before your period: Prostaglandin surges cause uterine contractions that refer pain to your upper back while triggering nausea
– First-trimester pregnancy: Morning sickness peaks alongside new postural strain from ligament laxity
– Perimenopause: Declining estrogen lowers pain thresholds, making chronic back issues more nauseating
Never ignore new upper back pain with nausea during pregnancy. Cholestasis of pregnancy—a second/third-trimester condition—causes intense itching alongside right-sided back pain and nausea and requires immediate intervention to protect your baby.
Kidney Infections: Exploiting Female Anatomy
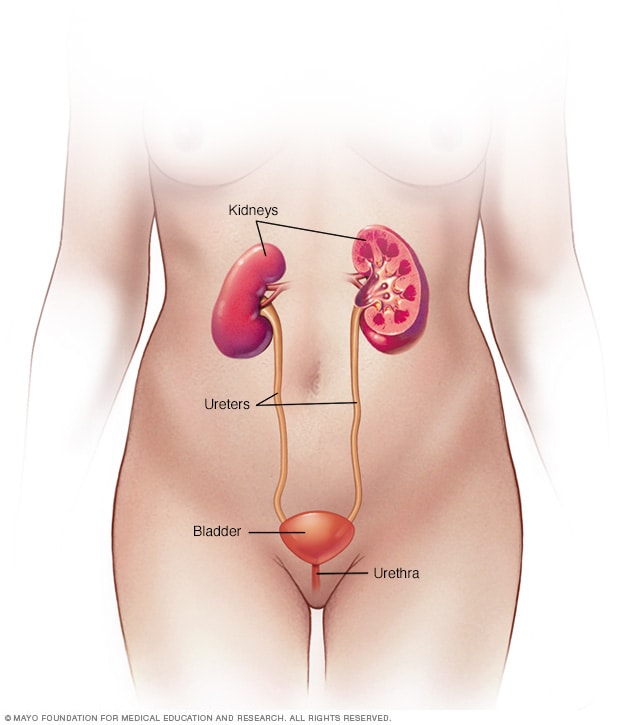
Your shorter urethra puts you at higher risk for bacteria traveling to your kidneys, causing infections that manifest as flank pain radiating to your upper back. The resulting toxins trigger nausea, creating a dangerous cycle where dehydration from vomiting worsens the infection. Symptoms often escalate quickly, especially during pregnancy when immune changes increase vulnerability.
Self-Check for Kidney Involvement
Perform these safe assessments before calling your doctor:
1. Press gently under your right ribs: Sharp pain during inhalation suggests gallbladder issues; flank tenderness (mid-back, just below ribs) points to kidneys
2. Check your urine: Cloudy, foul-smelling, or bloody urine confirms kidney involvement
3. Monitor fever: Temperatures above 101°F indicate infection needing antibiotics within 24 hours
Skip the common error of self-treating with cranberry juice alone—kidney infections require prescription antibiotics. Women on oral contraceptives face 30% higher risks due to altered vaginal pH.
Cardiac Red Flags Women Often Miss
Heart attacks in women rarely feature crushing chest pain. Instead, you might experience upper back pressure between shoulder blades, nausea with unexplained fatigue, or jaw pain—especially if you’re postmenopausal. This “atypical” presentation delays treatment by 2+ hours on average. If you feel clammy, sweaty, or a sense of “impending doom” with these symptoms, call 911 immediately.
When to Treat Nausea + Back Pain as an Emergency
Seek care within 2 hours if you have:
– Pain intensity reaching 8/10 or higher on a scale where 10 is unbearable
– Nausea preventing fluid retention for over 6 hours (risking dehydration)
– Fever spiking above 102°F with shaking chills
– Neurological symptoms like leg weakness or blurred vision
Go straight to the ER for pregnancy-related right upper quadrant pain, postpartum breathing difficulty with back pain, or vomiting blood/black stools. These signal life-threatening conditions like HELLP syndrome or internal bleeding.
Immediate Relief Strategies That Respect Female Biology
Positioning and Temperature Tactics
- Sit upright with lumbar support: Place a rolled towel behind your lower back to reduce diaphragm pressure. This eases both nausea and muscle strain within 15 minutes.
- Apply targeted temperature: Use cold compresses for gallbladder-related inflammation (wrap ice pack in cloth over right shoulder blade). Choose heat therapy for hormonal or muscular back pain (20-minute intervals).
- Hydrate strategically: Sip room-temperature ginger tea in teaspoon increments. Large gulps trigger vomiting, while dehydration worsens muscle spasms.
Pregnancy-Safe Medication Guide
| Symptom | Safe Option | Timing Tip |
|---|---|---|
| Back pain | Acetaminophen | Take before pain peaks; avoid ibuprofen after 28 weeks |
| Nausea | Ondansetron (Zofran) | Use only if ginger fails; safe throughout pregnancy |
| Bloating | Ginger chews (250mg) | Take 30 mins before meals to prevent nausea |
Never take NSAIDs for period-related back pain on an empty stomach—they increase ulcer risk when combined with nausea. Start ibuprofen 1–2 days before your period begins for best results.
Prevention Tactics Targeting Female Vulnerabilities
Daily Habits That Reduce Risk
- Correct posture at work: Raise computer monitors to eye level to prevent forward head posture. Set phone alarms every 30 minutes to reset your shoulders.
- Optimize bra fit: Get professionally measured every 6 months. Tight straps compress nerves running from neck to upper back, triggering nausea.
- Limit purse weight: Carry crossbody bags under 10 pounds to avoid asymmetric muscle strain that refers pain upward.
Gallbladder-Protective Nutrition
- Eat healthy fats daily: Avocados and olive oil prevent bile stagnation (zero-fat diets increase stone risk).
- Prioritize small, frequent meals: Prevents gallbladder overloading—eat every 3–4 hours, even when nausea-free.
- Add anti-inflammatory foods: Include turmeric in morning smoothies and fatty fish twice weekly to reduce systemic inflammation.
Your Action Plan: From Symptom Tracking to Treatment
Start documenting symptoms today using this simple framework:
1. Note pain location (right/left/both sides) and intensity (1–10 scale)
2. Record timing relative to meals, periods, or pregnancy stage
3. Log triggers like fatty foods or stress spikes
Most cases resolve with posture correction and dietary changes within 72 hours. But persistent symptoms demand medical evaluation—especially if fever develops or pain exceeds 6/10 for over 12 hours. Bring your symptom log to appointments; it helps doctors distinguish between gallbladder issues, kidney infections, or cardiac concerns faster.
Remember: Your body’s signals deserve validation. If a provider dismisses your “upper back pain and nausea female” symptoms as “stress,” seek a second opinion. Conditions like endometriosis or cholestasis require specialists familiar with women’s unique presentations. Schedule preventive screenings based on your risk factors—like annual liver tests if you’ve had gallstones—and establish care with providers who understand how female biology shapes pain pathways. Trust your instincts; timely action prevents minor issues from becoming emergencies.