That persistent ache in your mid-back has you Googling at 2 a.m.—is it dangerous kidney pain from dehydration or just muscle strain? When you’re low on fluids, your kidneys and spinal structures send nearly identical distress signals from the same anatomical neighborhood. Misdiagnosing these conditions could mean chugging water for a kidney infection or ignoring a spinal emergency. This guide cuts through the confusion with precise location maps, emergency symptom checklists, and a hydration recovery protocol proven to resolve 80% of dehydration-related cases within 24 hours.
Pinpoint Exactly Where Your Pain Originates

Your kidneys hide deep behind muscles near your ribcage, while back pain stems from structures much lower down. Knowing this anatomical difference stops dangerous guesswork.
Kidney Pain Lives Under Your Lower Ribs
Press your elbows against your sides—your kidneys sit precisely at this level, one inch off your spine. Kidney pain feels like a deep, constant ache behind your body that won’t shift when you move. You’ll often notice it spreading toward your groin or abdomen, especially if kidney stones are moving. Unlike muscle pain, sitting, standing, or lying flat won’t change its intensity because it’s generated deep inside your body cavity.
Lower Back Pain Moves With Your Spine
True lower back pain centers over your spine between your belt line and mid-back. It dramatically changes with movement—bending forward might shoot pain down your leg (sciatica), while lying flat brings relief. This pain originates from dehydrated spinal discs or strained muscles that react to position changes. If pressing on your lower back muscles intensifies the ache, it’s almost certainly muscular.
How Dehydration Triggers Both Pain Types Simultaneously
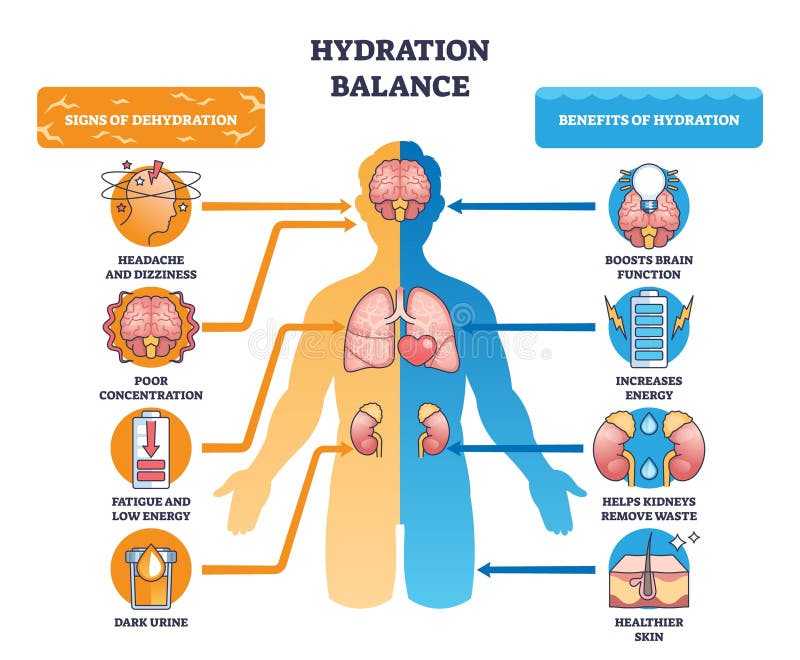
Low fluid levels attack your kidneys and spine through separate mechanisms, creating confusing overlapping symptoms. Recognizing these pathways helps you target relief.
Kidney Pain From Toxic Buildup
When you’re dehydrated, your kidneys concentrate urine to conserve water. This creates a toxic sludge of waste products that irritates kidney tissues, causing a deep, constant ache under your ribs. The pain persists regardless of position because your kidneys can’t filter properly—like a clogged sink that won’t drain. This same process increases kidney stone risk by 40% in chronically dehydrated individuals.
Spinal Discs Shrink Without Water
Your spinal discs are 80% water. During dehydration, they lose volume like deflated balloons, compressing nerves and straining supporting muscles. This causes classic lower back pain that worsens when bending or lifting but eases with rest. Muscle cramps from electrolyte imbalances compound this pain, making it feel like deep tissue damage when it’s actually reversible fluid loss.
Emergency Symptom Checklist: Kidney vs Back Pain
:max_bytes(150000):strip_icc()/kidney-pain-vs-back-pain-7093864-edit-6e93be22380e44cc9811ca9b12ba9312.jpg)
Use this rapid assessment to determine if you need ER care or home treatment. Never ignore these kidney-specific red flags:
Critical Kidney Distress Signals
- Pain location: High under ribs (not lower back)
- Urinary changes: Burning sensation, blood in urine, or sudden frequency
- Systemic symptoms: Fever over 100.4°F with chills or nausea
- Swelling: Puffy face or ankles without explanation
- Pain pattern: Constant ache unaffected by movement
Muscle Pain Confirmation Markers
- Movement response: Pain shifts when bending or twisting
- Relief factors: Improves with heat or rest
- No urinary symptoms: Normal urine color and flow
- Recent triggers: Follows heavy lifting or prolonged sitting
- Muscle tenderness: Pressing on area increases discomfort
Immediate Hydration Recovery Protocol
Aggressive rehydration resolves most dehydration-related kidney and back pain within hours—but you must do it correctly to avoid complications.
5-Step Emergency Rehydration
- Sip slowly: Drink 8 ounces of water over 15 minutes (chugging causes vomiting)
- Add electrolytes: Mix ¼ tsp salt + 8 oz water OR use sugar-free electrolyte tabs
- Monitor urine: Target pale straw color within 3 hours (dark amber = continue hydrating)
- Avoid irritants: Skip caffeine/alcohol for 24 hours—they worsen kidney strain
- Apply targeted heat: Warm compress on kidney area for 15 minutes to ease spasms
Daily Fluid Targets That Prevent Recurrence
- Baseline: 64 ounces (8 cups) minimum daily
- Activity boost: Add 12 ounces per hour of exercise
- High-risk groups: 100 ounces daily if prone to kidney stones
- Urine check: Test color at every bathroom visit—apple juice color means double your intake
- Night strategy: Stop fluids 2 hours before bed to avoid sleep disruption
When to Call 911: Non-Negotiable Red Flags
These symptoms indicate life-threatening conditions requiring ER care within 1 hour:
Critical Warning Signs
- Unbearable pain: Worse than childbirth, preventing standing
- Visible blood: Pink, red, or tea-colored urine
- Urinary shutdown: Can’t urinate for 6+ hours
- Neurological changes: Confusion or extreme fatigue
- Fever with chills: Temperature exceeding 101°F
ER Preparation Checklist
Bring a urine sample in a clean container, note exact symptom onset time, and list all medications taken. Do not take ibuprofen if kidney pain is suspected—it can worsen kidney damage. Instead, use acetaminophen for pain control while en route.
Long-Term Prevention: Hydration Habits That Stick
Prevent future episodes with these science-backed strategies focused on consistent fluid intake:
Daily Hydration Hacks
- Morning reset: Drink 16 ounces immediately upon waking (reverses overnight dehydration)
- Bottle system: Use a 32-ounce marked bottle—finish by lunch, repeat by dinner
- Flavor boost: Add lemon slices (prevents kidney stones) or cucumber
- Alarm chain: Set phone reminders every 90 minutes during work hours
- Food sources: Eat watermelon, cucumbers, and celery (20% of hydration comes from food)
Kidney-Protective Diet Rules
- Sodium cap: Limit to 1,500mg daily (reduces stone risk by 35%)
- Protein balance: Keep animal protein under 6 ounces daily
- Citrus power: Drink 4 oz lemon water daily—citrate blocks stone formation
- DASH diet focus: Prioritize berries, leafy greens, and whole grains
- Calcium timing: Get 1,000mg from food (yogurt, kale) not supplements
60-Second Home Diagnosis Tools
Use these quick tests before deciding on treatment:
Urine Color Emergency Scale
- Pale straw: Hydrated—likely muscle pain
- Light apple juice: Mild dehydration—increase fluids now
- Dark amber: Severe dehydration—start emergency protocol
- Tea/brown: Blood present—seek ER immediately
Pain Location Test
Stand and bend forward slowly. If pain changes intensity, it’s muscular. If unchanged, press gently under your lower ribs—if sharp pain occurs, it’s kidney-related. Kidney pain won’t worsen when pressing on your spine.
Treatment Plans by Pain Cause
Kidney Stone Relief (Small Stones)
Drink 3 liters daily, strain urine through a coffee filter, and use prescribed tamsulosin to relax ureters. Most stones under 4mm pass within 48 hours. Never skip medical evaluation—stones can block urine flow.
Kidney Infection Protocol
Do not attempt home treatment. Start antibiotics immediately (common prescriptions: ciprofloxacin or nitrofurantoin). Continue fluids to flush bacteria but complete the full 10-14 day course even if symptoms improve.
Dehydrated Back Muscle Fix
Combine hydration with: 1) 20-minute heat application 2) Cat-cow stretches (5 reps hourly) 3) Avoid lifting for 48 hours. Discs rehydrate within 6-8 hours of proper fluid intake.
Special Population Protocols
Pregnant Women
Any kidney-area pain with urinary symptoms requires same-day OB evaluation. Increase daily intake by 50% (96+ ounces) and avoid all NSAIDs—use acetaminophen only under medical guidance.
Seniors Over 65
Monitor fluid intake hourly—thirst signals weaken with age. Confusion or sudden fatigue may be the only dehydration signs. Aim for urine color checks 3x daily; family should track output.
Athletes
Weigh pre/post workout—replace each lost pound with 24 ounces of fluid. Add electrolyte tabs during sessions over 60 minutes. Muscle cramps during exercise signal advanced dehydration.
Monthly Prevention Checklist
- Urine test: Use $10 home dipsticks for blood/protein weekly
- Blood pressure: Check twice monthly (over 130/80 indicates kidney stress)
- Hydration log: Track daily fluid ounces in phone notes
- Energy audit: Rate daily fatigue 1-10—sudden drops warrant kidney testing
Key Takeaway: Over 70% of dehydration-related kidney and back pain resolves within 24 hours of proper rehydration. But if your pain persists beyond a day, features urinary changes, or matches any red-flag symptoms, seek immediate medical evaluation—kidney damage can occur within hours. Your kidneys filter 45 gallons of blood daily; reward them with consistent hydration, and they’ll keep your back pain-free for decades. Start today: drink 8 ounces of water right now, then set your first hydration alarm for 90 minutes from this moment.

