That persistent ache just above your hips isn’t “normal” – it’s your body signaling specific issues tied to being female. The reason for lower back pain for ladies often lies in biological factors men never experience, from cyclical hormone surges to pelvic anatomy and reproductive health shifts. When 80% of women report monthly back discomfort yet receive generic “stretch more” advice, understanding these female-specific triggers becomes critical. This article reveals the 7 hidden causes behind your pain – from endometriosis lesions to post-menopausal bone loss – so you can finally target relief instead of masking symptoms.
Hormonal Pain Triggers Only Women Experience
Why Your Period Turns Your Back Into a Pain Zone
Your uterus isn’t working alone during menstruation. When prostaglandins trigger uterine contractions, this pain radiates through shared nerve pathways to your lower back via the sacral plexus. This referred pain typically starts 1–3 days before bleeding, peaks during heavy flow days, and fades within 72 hours. Unlike mechanical back pain, this aching wraps around your hips and thighs and improves significantly with heat or NSAIDs.
Confirm it’s cycle-related if you notice:
– Pain timing perfectly matches your menstrual cycle
– Abdominal cramps precede back discomfort
– Sitting on a heating pad provides noticeable relief
– Symptoms vanish once your period ends
PMDD: When Back Pain Becomes Debilitating
While 80% of women experience PMS back pain, Premenstrual Dysphoric Disorder (PMDD) transforms this into disabling agony. With PMDD, your lower back may spasm so severely you struggle to stand upright for 3–7 days pre-menses. Warning signs include:
– Back pain interfering with work or daily tasks
– Pain accompanied by extreme mood shifts or anxiety
– Symptoms persisting beyond the first day of bleeding
– Previous diagnosis of depression or anxiety disorders
Endometriosis: The Silent Back Pain Culprit
Endometrial tissue growing outside your uterus creates a distinct pain pattern. Lesions on pelvic ligaments and the sacral area cause chronic lower back pain that worsens during periods but often persists all cycle long. This deep, knife-like pain frequently radiates down legs and intensifies during bowel movements or sex. If your “period back pain” lasts longer than 3 days or disrupts your life monthly, endometriosis could be the reason for lower back pain for ladies.
Pregnancy’s Unique Back Stressors

Second Trimester Back Pain Explained
Between months 5–7, 50–80% of pregnant women develop significant lower back pain as your center of gravity shifts forward. This creates an exaggerated arch (lordosis) in your lower spine, compressing facet joints and overstretching supporting muscles. Unlike typical back strain, pregnancy-related pain concentrates below your waistline across the sacrum, often worsening when standing still but improving when lying on your side.
Relaxin’s Double-Edged Sword
The relaxin hormone peaks in your first and third trimesters, loosening pelvic joints for delivery but destabilizing your entire lower back. This joint laxity makes simple movements risky – you might feel sharp sacroiliac pain when transitioning from sitting to standing. Critical mistake to avoid: Ignoring pelvic tilts. Performing 10 pelvic tilts hourly counteracts lordosis by realigning your spine.
Immediate Relief Tactics That Work
- Prenatal support belts: Reduce gravitational strain within 15 minutes
- Side-sleeping with pillow: Place between knees to maintain alignment
- Warm (not hot) baths: Limit to 100°F for safe muscle relaxation
- Avoid prolonged standing: Shift weight every 5 minutes to prevent muscle fatigue
Post-Menopausal Bone Loss Dangers

Osteoporosis Fractures: The Silent Threat
After menopause, declining estrogen accelerates vertebral bone loss. You might lose 1–2 inches in height gradually, then experience sudden severe back pain from a compression fracture during routine activities like coughing. Unlike muscle strain, this sharp, localized pain:
– Worsens significantly when standing or walking
– Improves immediately when lying flat
– Persists for weeks without improvement
– May cause visible spinal curvature (kyphosis)
Bone Defense Protocol
Daily requirements to protect your spine:
– Calcium: 1,200 mg (combine dairy, leafy greens, and supplements)
– Vitamin D: 800–1,000 IU for optimal calcium absorption
– Weight-bearing exercise: 30 minutes of brisk walking daily
– Alcohol limit: No more than one drink per day (accelerates bone loss)
Female Anatomy’s Pain Amplifiers
Wider Pelvis = More Back Stress
Your naturally wider pelvis increases the Q-angle (hip-to-knee angle), creating 3–4 times more torque on your lower spine with every step compared to men. This explains why women develop sacroiliac joint dysfunction far more often – you’ll feel deep buttock pain worsening with stair climbing or prolonged standing. Pro tip: When walking, engage your glutes to reduce pelvic sway and spinal stress.
High Heel Damage You Can’t Ignore
Heels over 2 inches tilt your pelvis forward 15–30 degrees, forcing your lower back into excessive arching. After just 2 hours in heels:
– Paraspinal muscles fatigue, causing deep aching
– Facet joints experience abnormal pressure
– Pain persists even after removing shoes
– Years of use contribute to chronic degeneration
Hidden Gynecological Causes
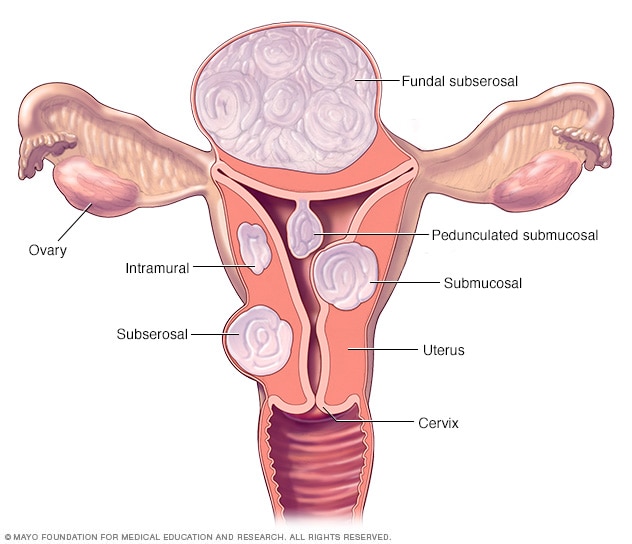
Fibroid Pressure Pain
Enlarged uterine fibroids increase pelvic weight, creating constant downward pressure on your sacrum. This manifests as a persistent dull ache worsening before periods. Multiple fibroids can expand your uterus to 4–5 months’ size, making standing unbearable. Key indicator: Back pain accompanied by heavy periods or urinary frequency.
PID’s Inflammatory Back Pain
Pelvic inflammatory disease causes deep, aching lower back pain through inflamed tissue irritating sacral nerves. Unlike mechanical pain, PID pain:
– Persists regardless of position changes
– Includes fever or abnormal discharge
– Worsens during intercourse
– Requires immediate antibiotics to prevent infertility
Lifestyle Contributors You Can Fix
Sitting Disease’s Back Impact
Prolonged sitting tightens hip flexors and weakens glutes, creating anterior pelvic tilt. Your lower back compensates with hyperlordosis, leading to paraspinal muscle overuse. Women desk workers often develop this by age 30, experiencing worse pain at day’s end. Fix this today: Set a timer to stand and extend your spine every 20 minutes.
Core Weakness You Didn’t Know You Had
Pregnancy, diastasis recti, and inactivity weaken deep abdominal muscles, forcing your back muscles to overwork. Test your core:
– Can’t maintain a plank for 30 seconds?
– Back arches when lifting legs lying down?
– Struggle to roll out of bed without using arms?
These indicate core deficiency requiring targeted rehab.
Red Flag Symptoms Requiring ER Care
Emergency Pain Indicators
Seek immediate help if experiencing:
– Saddle numbness: Loss of sensation in groin/inner thighs
– Bladder changes: Inability to urinate or sudden incontinence
– Progressive leg weakness: Worsening over hours
– Night pain: Wakes you from sleep and doesn’t improve with position
– Unexplained weight loss: With new-onset back pain
Cauda Equina: The 48-Hour Window
This rare but critical condition involves spinal nerve root compression. Beyond back pain, you’ll experience bilateral sciatica and possible bowel/bladder dysfunction. Act now: Emergency MRI and surgical decompression within 24–48 hours prevent permanent damage.
Proven Prevention Strategies
Daily Back-Saving Habits
- Heel limits: Reserve 3+ inch heels for events under 2 hours
- Lifting mechanics: Squat (don’t bend), keep loads close, engage core
- Sleep positioning: Side-sleep with knee pillow to maintain alignment
- 20-20-20 rule: Every 20 minutes sitting, stand and extend for 20 seconds
5-Minute Daily Core Routine
Perform this sequence daily to stabilize your spine:
1. Pelvic tilts: 10 reps (flatten back against floor while breathing deeply)
2. Bridges: Hold 5 seconds, 15 reps (lift hips while squeezing glutes)
3. Bird-dogs: Hold 5 seconds each side, 10 reps (opposite arm/leg extension)
4. Clamshells: 20 reps per side (side-lying hip rotation with knees bent)
Nutritional Back Support
Beyond bone health basics:
– Magnesium: 320 mg daily reduces muscle tension (spinach, almonds, supplements)
– Omega-3s: 1,000 mg daily fights inflammatory pain (salmon, walnuts, fish oil)
– Hydration: 8 glasses water daily maintains disc hydration
Your lower back pain isn’t “normal aging” or stress – it’s your body highlighting specific female health issues. Whether it’s cyclical endometriosis pain, pregnancy-related instability, or osteoporosis fractures, targeted solutions exist. Start tracking your pain patterns against your menstrual cycle, note what triggers relief, and bring these details to your doctor. Understanding the reason for lower back pain for ladies transforms guesswork into effective treatment – because lasting relief begins with identifying your unique cause.

