That knife-like stab in your lower back when bending to pick up laundry, the relentless ache that keeps you awake at 3 a.m., or the sudden spasm that makes standing impossible—severe low back pain in women isn’t just inconvenient, it’s life-disrupting. Unlike generic back pain guides, this one targets your reality: 80% of women face this, often fueled by hormonal shifts, pregnancy changes, or conditions like endometriosis that men never experience. When standard advice fails, it’s because nobody addressed why your pain flares with your period or mimics labor contractions. Here’s how to pinpoint your exact trigger and implement targeted relief—starting today.
Why Your Period or Pregnancy Ignites Debilitating Back Pain

PMS and PMDD Back Pain Patterns That Steal Your Week
Your pre-period back pain isn’t “just cramps.” When uterine contractions intensify before bleeding starts, inflammatory prostaglandins flood your pelvis, radiating sharp pain directly to your lumbar spine. PMS-related severe low back pain typically hits 1–2 days pre-period and vanishes once bleeding begins. But PMDD (premenstrual dysphoric disorder)—the severe form affecting women with family histories of mood disorders—turns this into relentless agony that disrupts work and relationships. Spot the critical difference: PMS brings a dull ache with bloating, while PMDD causes knife-like spasms paired with severe anxiety or depression that lasts a full week.
Action step: Track pain onset in your cycle app. If it starts >5 days pre-period and includes emotional symptoms, demand a PMDD evaluation—not just painkillers.
Endometriosis Rupture: Emergency Back Pain Signs
When endometrial tissue implants near your spine or ovaries, it triggers chronic lower back pain that worsens monthly. But ruptured ovarian cysts (endometriomas) cause sudden, excruciating back pain requiring ER care. This isn’t “bad period pain”—it’s a medical emergency if you experience:
– Back pain so severe you vomit or collapse
– Pain intensifying with bowel movements during menstruation
– Zero relief from standard NSAIDs (ibuprofen, naproxen)
Critical move: If pain syncs with your cycle and radiates to your hips, insist on a pelvic ultrasound immediately. Endometriosis affects 10% of women globally, yet diagnosis takes 7–10 years on average—don’t wait.
Pregnancy Back Pain Timeline You Can’t Ignore
Forget “back pain only in third trimester”—it often starts as early as month two. Your body releases relaxin, a hormone that loosens ligaments for birth but destabilizes your spine. As your center of gravity shifts forward, muscles overcompensate, causing:
– Weeks 8–12: Sharp tailbone pain from hormonal ligament laxity
– Weeks 20–28: Radiating mid-back pain as your belly strains spinal alignment
– Active labor: Sudden lower back spasms signaling baby’s head pressing on your sacrum
Pregnancy-specific fix: Sleep on your left side with a pillow between your knees and under your upper knee. This reduces pelvic tilt that strains your lumbar spine.
Sciatica vs. Osteoporosis: Non-Gendered Triggers Women Overlook

Sciatica Nerve Pain You Can Self-Test in 60 Seconds
Sciatica doesn’t just “hurt your back”—it shoots burning pain from your buttock down one leg, often with numbness. Here’s how to confirm it: Sit straight in a chair, extend your painful leg fully, and point your toes up. If pain rockets down your leg, it’s sciatic nerve compression (often from a herniated disc). If pain stays localized to your spine, it’s likely muscular strain. Critical distinction: Sciatica requires nerve-focused treatment—muscle strain needs targeted stretching.
Immediate relief: Lie on your back, pull your knee gently toward your opposite shoulder for 30 seconds. Repeat 3x hourly.
Osteoporosis Fracture: Silent Back Pain After Menopause
Post-menopausal estrogen loss turns vertebrae brittle—so brittle that a sneeze can cause a compression fracture. This isn’t “normal aging pain” if you notice:
– Sudden severe back pain after minor activity (like lifting groceries)
– A stooped posture developing overnight
– Pain worsening when standing but easing when lying down
Prevention non-negotiable: Get a DEXA scan by age 65 (or earlier if you have risk factors like early menopause). Pair 1,200mg calcium daily with 800–1,000 IU vitamin D to rebuild bone density.
Emergency Home Relief That Works Within Hours
Heat vs. Ice Protocol for Your Specific Pain Type
First 48 hours after acute injury: Ice for 15 minutes every 2 hours to reduce inflammation. After 48 hours: Switch to heat (20 minutes every 2 hours) to relax spasms. Pregnancy exception: Skip ice—apply a warm rice sock (fill cotton sock with uncooked rice, microwave 90 seconds) to your lower back instead. Why this works: Heat improves blood flow to heal strained muscles, while ice numbs acute nerve inflammation.
Movement That Stops Pain Cycles in 10 Minutes
Bed rest backfires—movement is medicine. Try these pain-specific moves:
– For sciatica: Knee-to-chest stretch (hold 30 seconds per leg, 3x daily)
– For muscle strain: 5-minute walks hourly to prevent stiffness
– Pregnancy-safe: Cat-cow stretch on hands and knees (10 reps hourly)
Pro tip: Walk backward for 2 minutes to decompress spinal discs naturally. Studies show it reduces disc pressure by 25%.
Medical Red Flags That Demand ER Visits—Not Google
When Back Pain Means “Go Now”
Severe low back pain in women requires immediate ER care if you have:
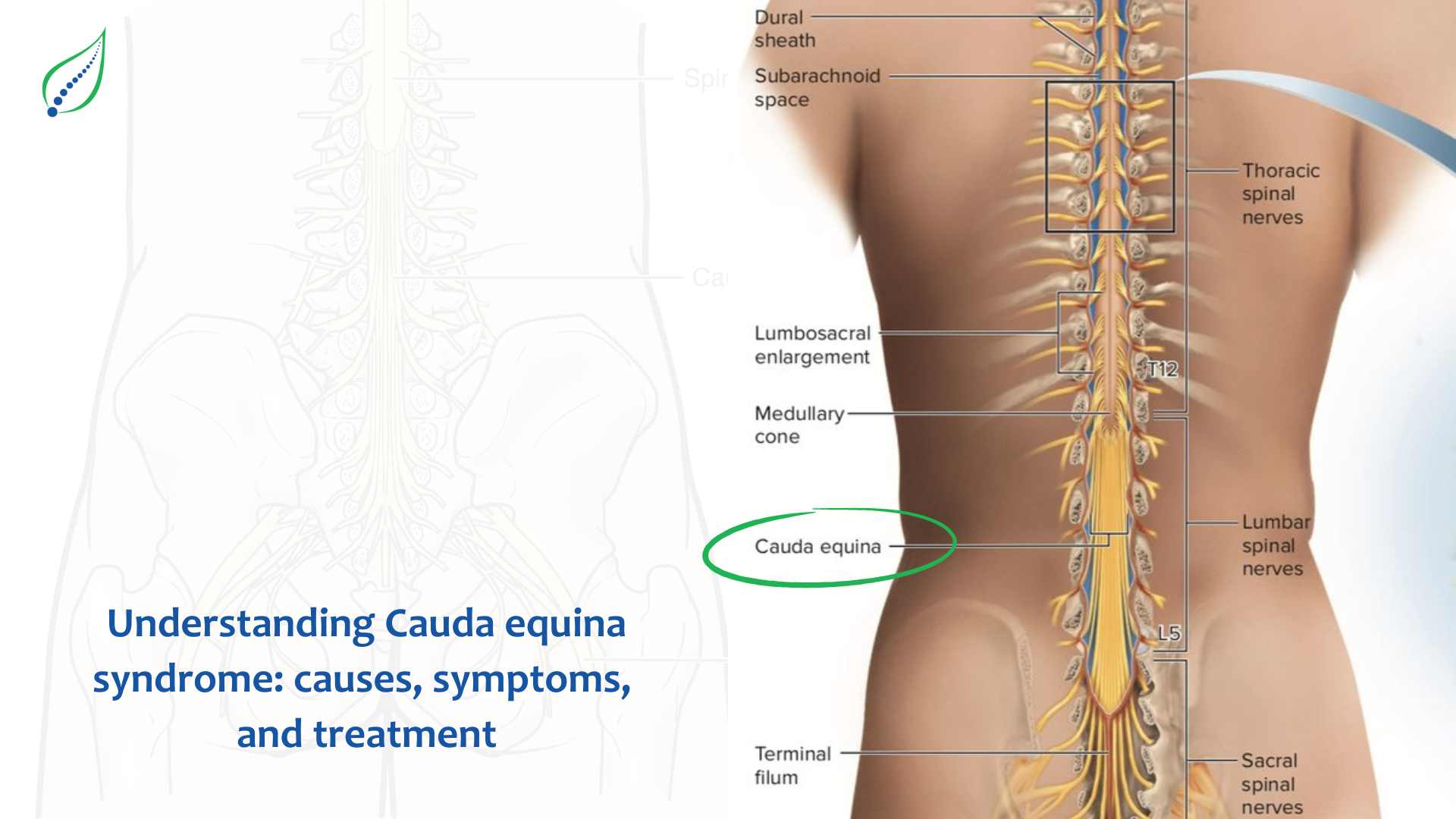
– Loss of bladder/bowel control (cauda equina syndrome—nerve damage is irreversible after 48 hours)
– Fever + back pain (possible kidney infection or PID)
– Numbness in inner thighs/groin (“saddle anesthesia” indicating spinal compression)
– Sudden pain after fall (possible osteoporosis fracture)
Do not wait: These symptoms escalate to paralysis or sepsis within hours.
Pain Medication Safety Guide for Your Condition
| Condition | Safe Immediate Relief | Pregnancy Caution |
|---|---|---|
| PMS/PMDD | Ibuprofen 400mg | Avoid NSAIDs after 20 weeks |
| Endometriosis | Naproxen + heating pad | Acetaminophen only |
| Osteoporosis Fracture | Acetaminophen + bracing | Consult OB before any medication |
Critical warning: NSAIDs (ibuprofen, naproxen) increase miscarriage risk by 80% in first-trimester pregnancy—never use without OB approval.
Prevention Strategies That Target Female Physiology
Daily Spine Protection Tactics
- Lifting hack: Hug objects to your sternum (not waist), bend knees, and exhale while standing—never twist
- Desk setup: Position monitor at eye level, use lumbar roll, and place feet flat on floor (not dangling)
- Sleep position: Side-sleep with pillow between knees and under your top arm to align shoulder/spine
Bone Density Defense After 40
Women lose 20% bone mass in first 7 post-menopausal years. Fight back with:
– Weight-bearing exercise: 30-minute walks 5x/week (dancing counts!)
– Calcium combo: 1,200mg calcium citrate + 1,000 IU vitamin D3 daily (take calcium in two 600mg doses)
– Eliminate bone robbers: Quit smoking (reduces calcium absorption by 30%), limit coffee to 2 cups
When to Demand Specialized Care
Physical Therapy Exercises That Fix 80% of Cases
A skilled PT will target your female-specific needs:
– Core stabilization: Bird-dog (extend opposite arm/leg while on hands/knees)
– Pelvic floor release: Manual therapy for endometriosis-related tension
– Posture retraining: Mirror drills to correct anterior pelvic tilt from pregnancy
Insist on this: Ask if they treat pregnancy or endometriosis patients—generic back PT often fails women.
Surgical Options for When Nothing Else Works
Only 5–10% of severe low back pain in women requires surgery. Consider if:
– Pain persists >12 weeks despite PT and medication
– You develop leg weakness or foot drop
– Endometriosis cysts rupture repeatedly
New option: The TOPS System replaces spinal fusion for some herniated discs, preserving motion with 92% patient satisfaction rates.
Bottom line: Severe low back pain in women stems from unique biological triggers—hormonal surges, pregnancy mechanics, or endometriosis—that generic advice ignores. Track your pain against your menstrual cycle, act within 24 hours of acute onset with targeted heat/movement, and never dismiss “period pain” that knocks you out for days. With 80% of women affected, you’re not alone—but relief requires treating your body, not a textbook case. Start today: Apply that rice sock, walk backward for 2 minutes, and book that ultrasound if pain syncs with your period. Your spine-friendly life starts now.

