That sharp twinge hits when you’re waiting in line or walking the dog—your lower back screams as gravity pulls relentlessly on compressed discs. You’re not imagining it: 84% of adults battle this exact pain, making standing- and walking-triggered back pain the top cause of work disability worldwide. But here’s the critical truth—97% of cases stem from mechanical issues like strained muscles, bulging discs, or postural fatigue, not serious disease. You can fix this without surgery. This guide reveals why upright movement hurts, how to decode your specific pain pattern in 60 seconds, and the exact home remedies, posture tweaks, and exercises proven to restore pain-free standing and walking within weeks.
Why Standing Overloads Your Lumbar Spine
Upright posture slams 40% more compressive force onto your lumbar discs than lying down. After just two hours of standing, 50% of healthy adults develop aching backs as paraspinal muscles fatigue and spasm. Weak core muscles accelerate this—like slack tent guy-lines forcing the spine pole to wobble. Your back muscles then overcompensate until they cramp, causing that signature dull belt-line ache that vanishes when you sit.
Disc Compression That Ignites Sciatica Pain
Prolonged standing narrows disc height, letting bulging material nudge sciatic nerve roots. This creates burning leg pain that radiates from buttock to calf—a hallmark of sciatica. Relief comes instantly when you bend forward (like leaning on a shopping cart), which opens disc space and eases nerve pressure. If walking triggers electric shocks down one leg, disc compression is likely the culprit.
Postural Collapse That Fatigues Back Muscles
Hyperlordosis (excessive lower-back curve) or swayback forces vertebrae into unnatural alignment. This happens with weak abs, tight hip flexors, or pregnancy. Your erector spinae muscles fire nonstop to prevent collapse, leading to cramps by midday. You’ll notice pain worsens the longer you stand but eases immediately when seated—a telltale sign of postural muscle overload.
Match Your Pain to the Exact Cause in 60 Seconds
| Pain Description | Likely Source | Critical Clues |
|---|---|---|
| Dull, bilateral ache | Muscle strain | Worsens after 20+ minutes standing; eases with sitting |
| Sharp, one-sided leg pain | Herniated disc | Tingling in foot; better when bent forward |
| Cramping legs after 5 minutes walking | Spinal stenosis | Stops within 1 minute of sitting or leaning on cart |
| Sudden severe pain after minor fall | Compression fracture | History of osteoporosis; pain when rolling in bed |
Red-flag alert: Skip home fixes immediately if you have saddle numbness (genital/anal area), bladder leaks, or foot drop (toe dragging). These require ER care for cauda equina syndrome.
3-Minute Pain Relief Tactics for Standing Episodes

Ice vs. Heat: The 48-Hour Rule
Apply ice packs (wrapped in thin cloth) for 15 minutes within 48 hours of acute strain to reduce inflammation. Switch to heat after two days—for chronic stiffness, a 20-minute warm shower relaxes spasmed muscles by boosting blood flow. Never apply heat during initial inflammation; it worsens swelling.
Instant Spine-Offloading Positions
- Grocery line hack: Place one foot on a curb or step to reduce lumbar curve by 30%.
- Kitchen relief: Open lower cabinet doors and rest a foot on the shelf while washing dishes.
- Office reset: Every 25 minutes, walk 10 steps or sit for 90 seconds to flush lactic acid from fatigued muscles.
Smart OTC Pain Management
- NSAIDs: Ibuprofen 400mg every 6 hours (max 1,200mg/day) with food to avoid stomach irritation.
- Topical relief: Diclofenac gel rubbed twice daily on sore spots penetrates deeper than pills with fewer side effects.
- Critical caution: Never exceed 10 days of NSAID use without medical review—kidney damage risk rises sharply.
Perfect Your Standing Posture in 60 Seconds
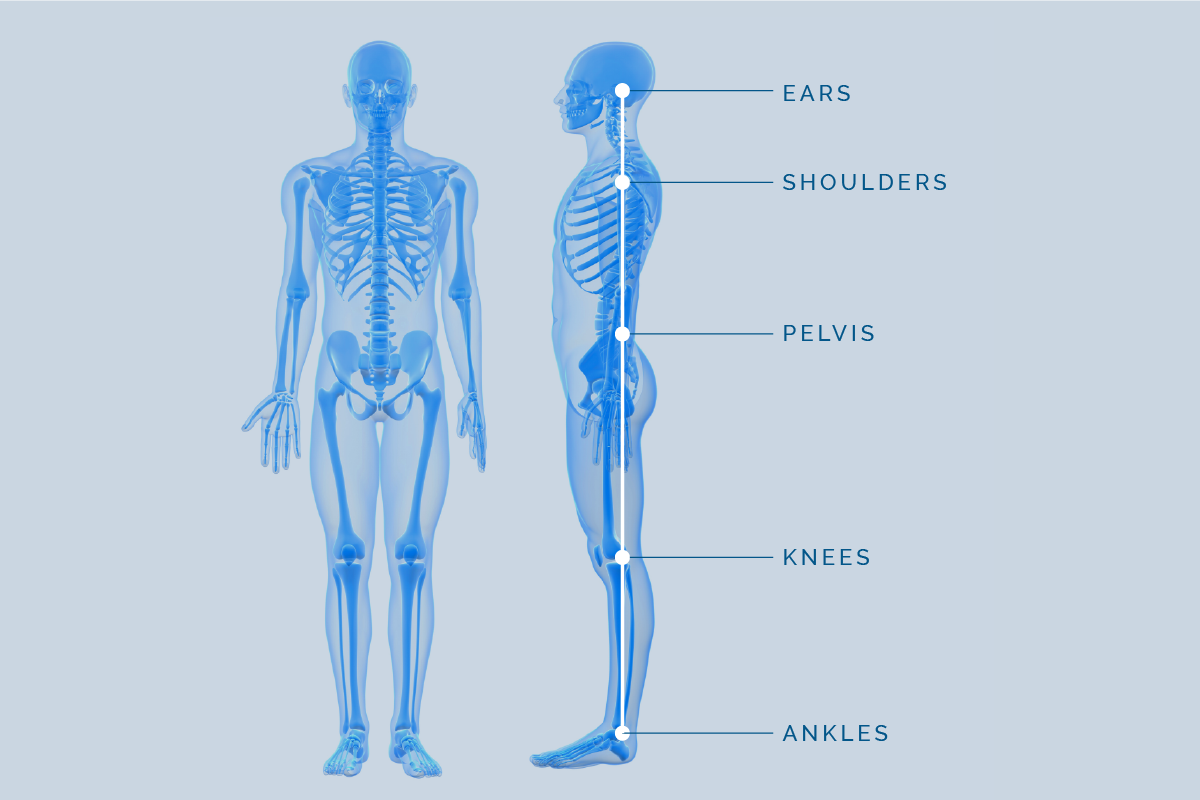
Stand feet hip-width apart with knees slightly bent (“soft”). Shift weight evenly across both feet—avoid rolling to outer edges. Tuck your tailbone under gently to neutralize excessive arch (imagine zipping a tight pair of jeans). Engage lower abs by drawing your belly button toward your spine without holding your breath. Finally, align ears over shoulders and shoulders over hips—text neck adds 10lbs of strain per inch your head juts forward. Ditch ballet flats and heels over 2cm; opt for cushioned sneakers with arch support or custom orthotics.
5 Standing-Friendly Stretches (Do Anywhere)
Hold each 25 seconds, twice daily. Stop if pain radiates below the knee.
1. Standing hamstring stretch: Prop heel on step, hinge at hips (not waist) until gentle thigh pull.
2. Hip flexor lunge: Half-kneel, tuck pelvis under to feel front-hip stretch on back leg.
3. Sink decompression: Hands on counter, walk hips back while bending knees slightly.
4. Knee-to-chest: Lie down, pull both knees to chest to relieve disc pressure.
5. Child’s pose: Kneel, sit back toward heels with arms extended for spinal flexion.
Core Strengthening That Ends Standing Pain
Start with activation moves before progressing. Do daily:
– Phase 1 (Days 1-7): Pelvic tilts lying down—flatten lower back into floor, hold 3 seconds (2×15 reps).
– Phase 2 (Week 2): Front plank on elbows—maintain straight line head-to-heels (3×20 seconds).
– Phase 3 (Week 3): Bird-dog—extend opposite arm/leg without wobbling (3×8/side).
Stop any exercise causing leg pain—this signals nerve irritation needing professional evaluation.
When to Seek Professional Help (Don’t Wait 6 Weeks)
See a physical therapist if pain persists beyond 10 days despite home care. They’ll prescribe targeted core stabilization and manual therapy—80% of patients improve within 8 sessions. For radiating leg pain, an epidural steroid injection can reduce inflammation around pinched nerves for weeks. Reserve surgery like microdiscectomy only for progressive foot drop or bowel/bladder issues.
Red-Flag Symptoms Requiring Same-Day Doctor Visit
- Pain lasting >6 weeks despite consistent stretching/posture work
- Numbness spreading to both feet or groin area
- Night pain waking you despite rest and painkillers
- Unexplained weight loss or fever accompanying back pain
Call 911 immediately for saddle numbness, urinary retention, or bilateral leg weakness—these indicate cauda equina syndrome.
Prevent Standing Pain From Returning
- Move every 25 minutes: Set phone alarms to reset muscle fatigue.
- Lift properly: Bend at hips (not waist), keep objects close to your body.
- Sleep smart: Medium-firm mattress with pillow under knees (back sleepers) or between knees (side sleepers).
- Lose 5kg: Every 4-5kg reduction cuts lumbar disc load by 15%.
- Vitamin D boost: Adults over 50 need 1,000IU daily for bone density—critical if osteoporosis runs in your family.
Take action today: Pick one stretch (try the sink decompression), one posture tweak (soft knees while standing), and one core move (pelvic tilts). Do them consistently for 7 days. Track how long you can stand pain-free—most people gain 15+ minutes by Day 4. Within three weeks, you’ll transform grocery lines from agony to routine, proving that standing and walking without back pain isn’t a luxury—it’s your birthright.

