That deep, aching pressure in your lower back might not be from lifting something heavy or sleeping awkwardly—it could be trapped gas pressing against your spine. Many people waste weeks trying back pain remedies that fail because they’re treating the wrong problem. The truth? Gas-related lower back pain responds dramatically to specific techniques that target your digestive system, not your muscles. When gas gets trapped in your intestines, it creates pressure on surrounding nerves and muscles that refer pain directly to your lower back.
This frustrating condition affects millions who mistakenly believe they’ve pulled a muscle. You might notice the pain intensifies after meals or when lying down, then suddenly vanishes after passing gas. The good news is that with the right approach, you can relieve gas pain in lower back within minutes and prevent future episodes with simple lifestyle tweaks. In this guide, you’ll discover how to accurately identify gas-related back pain, implement immediate relief techniques, and develop long-term strategies to keep your digestive system running smoothly.
Spot the Difference: Gas Pain Versus Muscle Injury
Telltale Signs Gas Is Your Culprit
Gas-related lower back pain has distinct characteristics that set it apart from muscle strain. The pain typically feels like a dull, moving pressure rather than a sharp, localized ache. You’ll notice it intensifies after eating certain foods or when sitting/lying down for extended periods, then dramatically improves after passing gas or having a bowel movement. Listen for accompanying symptoms: audible gurgling from your abdomen, a “tight” or “pulling” sensation across your lower back that shifts position as gas moves through your intestines.
Unlike muscle injuries that worsen with movement, gas pain often improves with gentle walking or positional changes. The cyclic nature of your discomfort—predictable patterns tied to meals and digestion—is your biggest clue that trapped gas, not a pulled muscle, is causing your lower back pain.
Critical Warning Signs Needing Immediate Care
While gas pain is usually harmless, certain symptoms require urgent medical attention. Contact your healthcare provider immediately if you experience severe pain lasting more than 24 hours, fever above 100.4°F, vomiting, or blood in your stool. Sudden, sharp pain that could indicate appendicitis or gallstones, and chest pain that might signal cardiac issues, also warrant emergency evaluation. Don’t assume all lower back pain is gas-related when these red flags appear.
Immediate Relief Techniques That Work in Minutes
Knee-to-Chest Gas Release Position
Lie flat on your back on a comfortable surface and gently pull both knees toward your chest, hugging them with your arms. Hold this position for 30-60 seconds while taking slow, deep breaths. This posture compresses your intestines in just the right way to help trapped gas move through your digestive system while simultaneously stretching tight lower back muscles. Most people experience noticeable relief within two minutes of holding this position, especially when combined with deep breathing to relax abdominal muscles.
Targeted Heat Application for Dual Relief
Apply a heating pad set to medium heat directly to your lower back for 15-20 minutes. The warmth serves two crucial purposes: relaxing intestinal muscles to allow trapped gas to move freely while simultaneously easing muscle tension in your back. For maximum effectiveness, alternate the heating pad between your lower back and lower abdomen every five minutes. This dual-application technique addresses both the digestive source and muscular manifestation of your pain, providing comprehensive relief within 10-15 minutes for most sufferers.
Walking and Gentle Spinal Twists
Start with a 5-10 minute walk at a comfortable pace immediately after noticing gas-related back pain. Light movement stimulates digestive motility and helps gas move through your system more efficiently. Follow your walk with gentle spinal twists: while sitting upright in a chair, slowly rotate your torso left and right, holding each position for 10-15 seconds. These movements create space in your digestive tract while loosening tight back muscles that may be trapping gas. Avoid vigorous twisting which can worsen discomfort—gentle, controlled movements yield the best results.
Dietary Fixes to Prevent Future Episodes
Eliminate These Gas-Triggering Foods Immediately
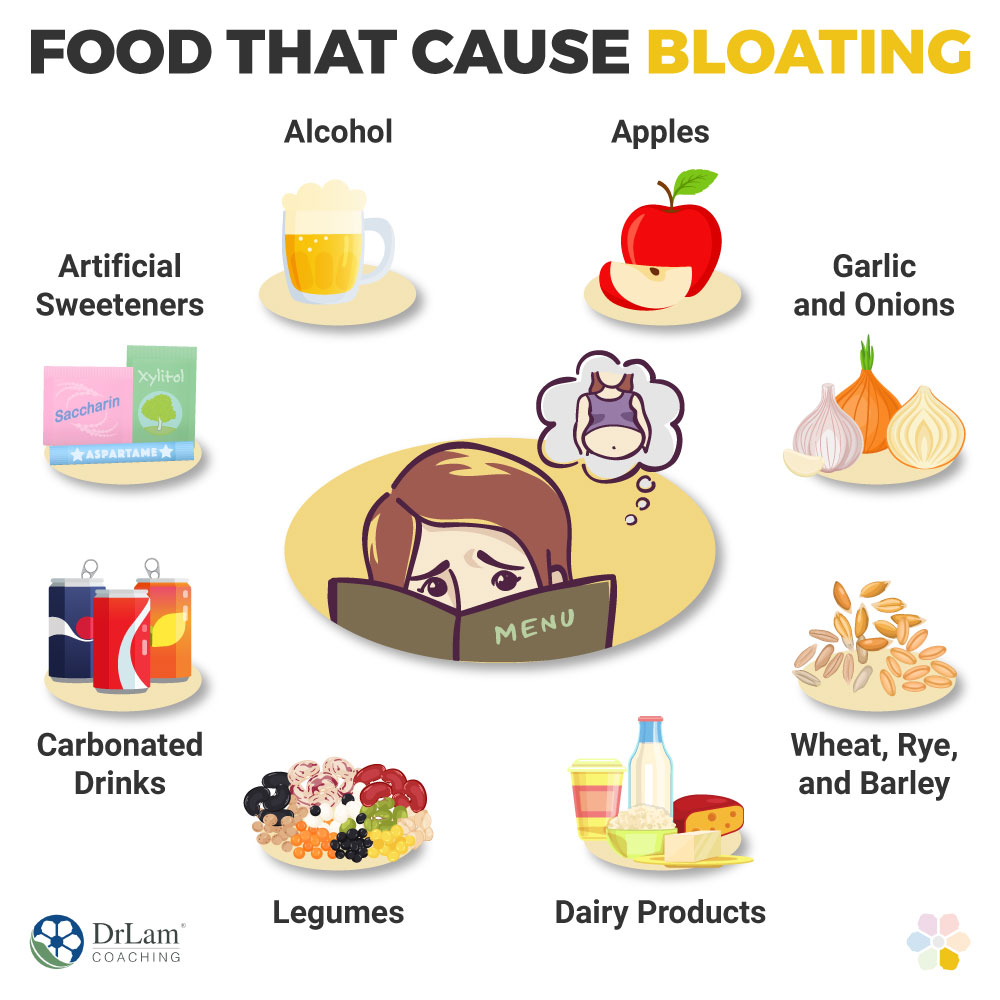
Certain foods consistently trigger gas production and subsequent back pain. Reduce or temporarily eliminate these common offenders:
- Beans, lentils, and other legumes
- Cruciferous vegetables (broccoli, cabbage, Brussels sprouts)
- Carbonated beverages including soda and sparkling water
- Artificial sweeteners like sorbitol and xylitol found in sugar-free products
- Dairy products if you suspect lactose intolerance
Many people overlook hidden gas producers like whole grains introduced too quickly into the diet. While healthy, these can overwhelm your digestive system and cause significant gas pressure that refers to your lower back.
Incorporate These Gas-Reducing Foods Daily
Add these digestive-friendly options to your meals to minimize gas formation:
- Peppermint: Sip peppermint tea after meals or chew fresh leaves—its natural antispasmodic properties relax digestive muscles
- Ginger: Try fresh ginger tea or add grated ginger to meals for its anti-inflammatory digestion benefits
- Fennel seeds: Chew ½ teaspoon after meals or steep for tea—centuries of traditional use for gas relief
- Papaya: Eat fresh as a between-meal snack; contains papain enzyme that breaks down proteins
These natural remedies work synergistically to reduce gas production at its source, preventing the abdominal pressure that causes lower back pain.
Smart Eating Habits to Stop Gas Before It Starts

Transform Your Meal Patterns Immediately
Switch to smaller, more frequent meals rather than three large ones—this reduces digestive burden and minimizes gas formation. Allow 3-4 hours between your last meal and bedtime to prevent nighttime gas accumulation that leads to morning back pain. Most importantly, slow your eating pace significantly: aim for 20-30 minutes per meal to reduce air swallowing, a major contributor to trapped gas.
Perfect Your Eating Technique
Avoid talking while chewing to minimize air intake during meals. Chew each bite 20-30 times until nearly liquid—this thorough chewing aids initial digestion and reduces intestinal workload. Sit upright during and after meals; slouching compresses your abdomen and traps gas that later refers to your lower back. These simple technique changes can reduce gas production by up to 40% within just a few days.
Over-the-Counter Solutions for Persistent Gas Pain

Strategic Use of Enzyme Supplements
Take alpha-galactosidase (Beano) just before meals containing gas-producing foods—these enzymes break down complex sugars before they ferment in your gut. For dairy-related issues, take lactase supplements with the first bite of dairy products. Timing is critical: these work best when taken immediately before problematic foods, not after symptoms appear.
Fast-Acting Gas Medications
Keep simethicone (Gas-X) on hand for immediate relief when gas pressure builds. This medication breaks up gas bubbles in your digestive tract, making them easier to pass and relieving the pressure causing your back pain. Take it at the first sign of gas discomfort—not after pain becomes severe—for maximum effectiveness. Activated charcoal may help absorb excess gas, but take it 2 hours away from other medications to prevent absorption interference.
Long-Term Prevention Strategies for Gas-Free Living
Daily Movement Patterns That Prevent Gas Trapping
Incorporate 30 minutes of moderate daily exercise like walking or swimming to maintain healthy digestive motility. Focus particularly on gentle torso-twisting movements, as these help prevent gas from becoming trapped in specific intestinal segments. Many people find that just 10 minutes of morning stretching reduces gas-related back pain by 50% within two weeks.
Stress Reduction Techniques That Aid Digestion
Implement daily stress-reduction practices because anxiety directly impacts digestion and increases gas production. Try just 5 minutes of deep breathing exercises morning and evening—this simple habit can dramatically reduce both gas formation and the muscle tension that amplifies back pain. Keep a symptom journal to identify personal stress-gas-back pain patterns; most people discover their back pain worsens during high-stress periods even with identical diets.
When to Consult a Healthcare Professional
Recognize These Professional Care Indicators
Schedule an appointment if gas-related back pain persists despite two weeks of dietary changes and home remedies. Consult a gastroenterologist if you have family history of digestive disorders, suspect specific food intolerances, or need prescription-strength solutions. A physical therapist can help if muscle tension contributes to your pain pattern, especially when combined with digestive issues.
Prepare These Questions for Your Doctor
Bring specific questions to maximize your appointment: “Could an underlying condition like IBS cause my symptoms?” “What tests should rule out serious conditions?” “How long should dietary changes continue before trying other interventions?” “Are prescription medications appropriate for my situation?” Being prepared helps you get the most accurate diagnosis and effective treatment plan.
Gas-related lower back pain responds remarkably well to targeted interventions that address both digestive and muscular components. Most people experience significant improvement within 1-2 weeks of implementing these specific strategies. Remember that everyone’s digestive system is unique—what works quickly for one person may take longer for another. Track your responses to different techniques, adjust your approach based on results, and don’t hesitate to seek professional guidance if symptoms persist beyond two weeks of consistent effort. With the right combination of immediate relief techniques and long-term prevention strategies, you can finally break free from the cycle of gas pain in lower back.