That sharp jab when lifting your suitcase or the persistent ache after raking leaves—back muscle strain pain affects over 51 million Americans dealing with chronic pain, with low-back issues topping the list. Most recover fully within weeks, but missteps in early care can turn a minor strain into months of frustration. Skip the endless googling and conflicting advice. This guide delivers the exact science-backed steps to stop acute pain, restore movement, and prevent future episodes—based on clinical protocols used by physical therapists and pain specialists.
Pinpoint Your Back Muscle Strain Symptoms Immediately
Sharp Pain Triggers vs. Dull Ache Patterns
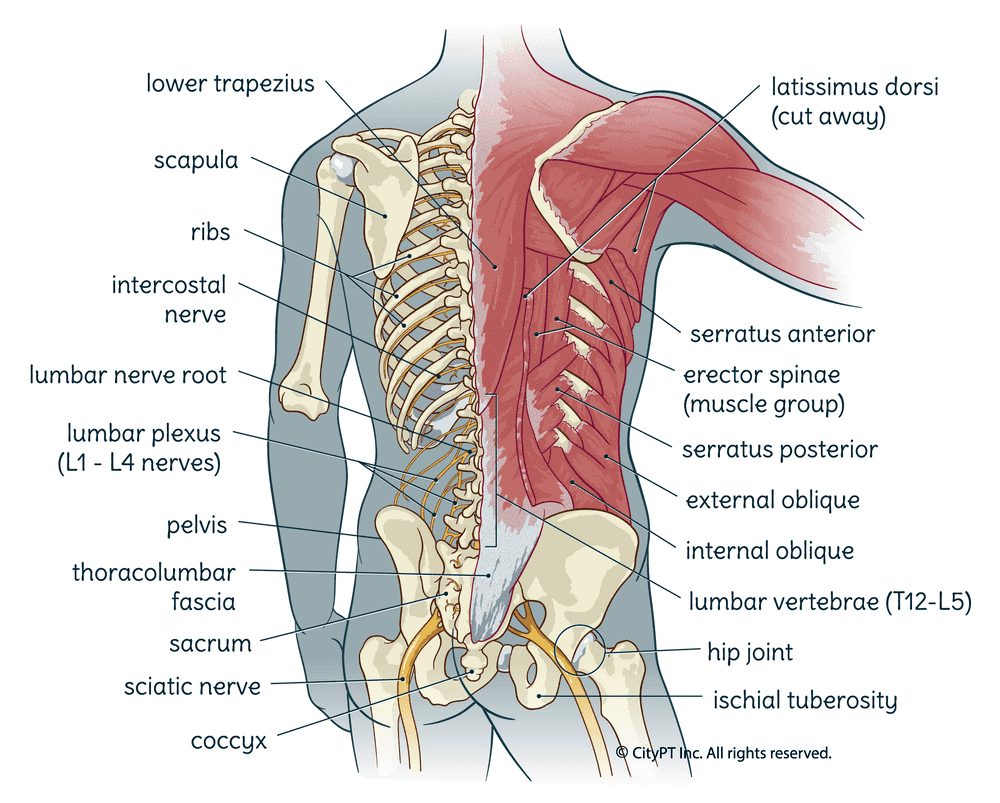
Back muscle strain pain announces itself through distinct patterns. A sudden stabbing sensation hits during specific movements like twisting or heavy lifting, while a persistent dull ache worsens steadily throughout your workday. Crucially, this pain stays confined to your lower back—between ribcage and buttocks—and rarely travels below the knees. You’ll notice it flares when bending forward to tie shoes or lifting grocery bags, yet eases when lying flat on your back. If pain shoots down your leg past the knee, seek evaluation for possible nerve involvement.
Muscle Spasm Danger Signals
Watch for involuntary muscle spasms that feel like hard knots under your skin. These protective contractions create visible bulges along your spine and often follow an audible “pop” during injury. Spasms severely limit your ability to stand upright or twist your torso, making simple tasks like getting out of bed feel impossible. These aren’t just discomfort—they’re your body’s alarm system signaling torn muscle fibers triggering inflammation. Ignoring them prolongs healing by forcing abnormal movement patterns.
Movement Limitations That Demand Action
Strain pain manifests through functional red flags: inability to transition smoothly from sitting to standing, a hunched posture when walking, or avoiding movement altogether. When basic tasks like putting on socks cause wincing, your muscles are in protective guarding mode. This isn’t laziness—it’s your nervous system restricting motion to prevent further damage. Document these limitations; they guide your recovery timeline and signal when to escalate care.
Target Your Personal Risk Triggers

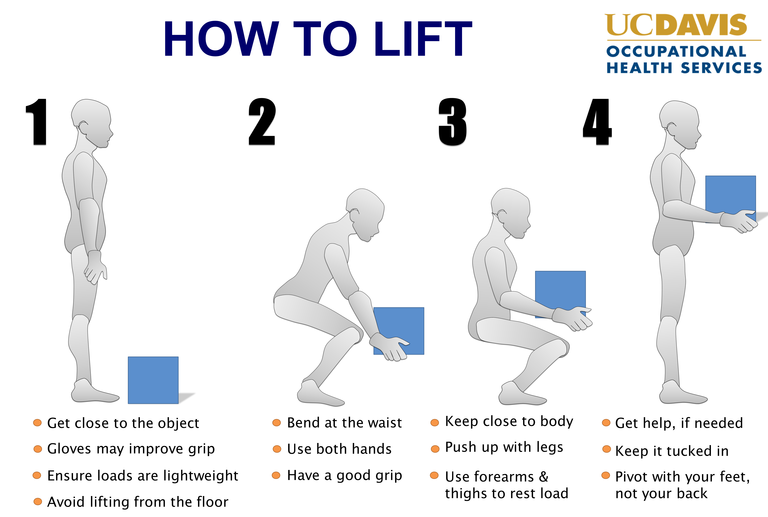
Activity-Specific Injury Culprits
Your weekend warrior habits might be setting you up for strain. Sudden lifting without bending knees, forceful twisting during sports like tennis or golf, or repetitive bending during yard work overload spinal muscles. Weightlifters often strain during deadlifts with improper form, while basketball players suffer from explosive pivots. The common thread? Rapid force application exceeding your muscles’ current capacity. Track your injury moment—it reveals your weak links for future prevention.
Occupational Threats You Can Control
Desk jobs create silent strain through prolonged sitting that compresses spinal discs, while truck drivers face vibration-induced microtrauma. Nurses lifting patients and construction workers handling heavy materials face triple threats: awkward postures, repetitive motions, and insufficient recovery time. Even “safe” jobs become risky with poor ergonomics—like typing with slumped shoulders or staring down at a phone. Your workstation isn’t neutral; it’s either healing or harming your back daily.
Hidden Vulnerability Amplifiers
Weak core muscles fail to stabilize your spine during simple tasks, turning a sneeze into an injury trigger. Poor hip flexibility forces your lower back to compensate during walking, while excess weight multiplies spinal load—every extra pound adds 4 pounds of pressure when upright. Previous injuries increase recurrence risk by up to 69%. Most overlooked? Stress and negative mindset—they literally amplify pain perception through neural pathways. Address these, and you tackle strain at its roots.
Stop Acute Back Muscle Strain Pain in 72 Hours
Ice Application Protocol That Works
Apply ice packs wrapped in thin cloth for 15 minutes every 2 hours during the first 48 hours. This isn’t just numbing—it constricts blood vessels to reduce inflammatory fluid buildup around torn fibers. Skip gel packs straight from the freezer; they cause frostbite. Instead, use a bag of frozen peas that molds perfectly to your spine. Stop icing once the area feels deeply cold (never numb), and never sleep with ice on your back.
Smart Medication Strategy
Start NSAIDs within 1 hour of injury: Ibuprofen 400mg every 8 hours or Naproxen 220mg every 12 hours. These block inflammation at the source—unlike acetaminophen, which only masks pain. If stomach issues prevent NSAID use, acetaminophen 650mg every 8 hours is a weaker alternative. Avoid muscle relaxants like cyclobenzaprine unless spasms prevent sleep—they cause drowsiness without healing benefits. Never use opioids; they delay recovery by promoting inactivity.
Critical Rest Period Limits
Confined rest beyond 48 hours backfires by weakening supporting muscles. Instead, move within pain tolerance: walk to the bathroom every 30 minutes, perform seated ankle pumps, or do gentle shoulder rolls. Your goal isn’t complete stillness—it’s avoiding movements that spike pain above 3/10. Set hourly phone alarms to reset your posture. This “relative rest” maintains blood flow to damaged tissues without re-injury.
Restore Movement Without Re-Injury (Days 3-14)
Heat Therapy Timing Mistakes to Avoid
Switch to heat only after inflammation peaks (typically day 3). Applying heat too early increases swelling like pouring gasoline on fire. Use a microwavable rice pack for 20 minutes while performing cat-cow stretches. Morning showers are ideal—let hot water hit your lower back while slowly bending knees. Never use heating pads while sleeping; burns occur before you feel them.
Safe Activation Walks That Heal
Begin walking within 72 hours: Start with 3-minute walks every 2 hours, focusing on tall posture (imagine a string pulling your head upward). Increase duration by 1 minute daily only if pain doesn’t spike. Walk on flat surfaces—avoid hills initially. If walking hurts, regress to seated marches: lift knees alternately while sitting tall. This gentle loading stimulates collagen alignment in healing muscles.
Manual Therapy That Actually Helps
Schedule massage only after acute pain subsides (day 4+). Request “myofascial release” techniques—not deep tissue—that follow pain referral patterns. Research shows massage combined with movement re-education outperforms either alone for subacute pain. Avoid aggressive spinal manipulation in the first week; it risks worsening micro-tears. Chiropractic adjustments become appropriate only when movement restrictions persist beyond 10 days.
Prevent Recurrence With Proven Daily Habits
Core Exercises That Protect Your Spine
Start pelvic tilts day 3: Lie on back with knees bent, gently flatten lower back into floor while exhaling (hold 5 seconds). Progress to bird-dog by day 7: On hands and knees, extend right arm/left leg while keeping hips level. Perform 2 sets of 10 daily. These activate deep stabilizers without straining healing tissues. Skip crunches—they compress injured discs.
Sleep Position Fixes for Pain Relief
Side sleepers: Place a pillow between knees to prevent pelvic rotation that strains your back. Back sleepers: Roll a towel under knees to maintain natural lumbar curve. Never sleep on your stomach—it forces spinal rotation all night. Test positions by waking at 3 AM; if you’ve shifted positions, that’s your body seeking relief from strain.
Lifting Technique Overhauls That Stick
Relearn lifting: Stand close to objects, bend knees deeply (not waist), keep load against your torso, and pivot feet—not spine—when turning. For grocery bags, use a backpack instead of carrying unevenly in one hand. At work, request a sit-stand desk; standing while working reduces disc pressure by 40% versus sitting. Set phone reminders every hour to reset your posture.
Emergency Red Flags That Demand ER Visits
Immediate Danger Signs You Can’t Ignore
Call 911 if you experience leg paralysis, loss of bladder/bowel control, or saddle numbness (genital area). These indicate cauda equina syndrome—a surgical emergency. Also seek ER care after major trauma like car accidents if back pain prevents standing. Don’t “wait and see” with these; permanent damage occurs within 48 hours.
Urgent Warning Signs Needing Same-Day Care
Contact your doctor immediately for new leg weakness (tripping when walking), fever with back pain, or unexplained weight loss. These could signal spinal infection or cancer—conditions mimicking strain but requiring urgent intervention. First-time severe pain after age 50 also warrants same-day evaluation to rule out fractures.
Final Note: Back muscle strain pain typically resolves within 2-4 weeks when you activate early, move intelligently, and target your personal risk factors. The 35-69% recurrence rate isn’t fate—it’s preventable through consistent core strengthening and ergonomic adjustments. Start pelvic tilts today, optimize your workstation tonight, and walk for 5 minutes hourly. Your spine’s resilience surprises most people; honor it with daily care, and you’ll transform strain from a recurring nightmare into a one-time lesson.