You’ve faithfully attended every physical therapy session, mastered your prescribed bridges and planks, and diligently performed cat-cow stretches for weeks. Yet your back pain persists—or worse, it intensifies. This frustrating reality affects millions: Up to 80% of Americans experience back pain, with 10% developing chronic conditions. When physical therapy not helping back pain becomes your reality, you’re caught in a demoralizing cycle of generic exercises that miss the true source of your discomfort. The truth? Standard PT fails 85% of chronic low-back pain cases because they’re mislabeled as “non-specific,” leaving you with symptom-focused treatments that ignore underlying tissue damage. This guide reveals why exercise therapy often backfires and delivers evidence-based solutions when physical therapy not helping back pain is your daily struggle.
Why Standard PT Fails Most Back Pain Cases
Core Pathologies Exercise Can’t Fix
Traditional physical therapy operates on the flawed assumption that strengthening muscles will stabilize your spine. When ligamentous spinal instability creates “wandering vertebrae,” your muscles lack firm anchor points—making even perfect planks counterproductive. Your body compensates with dysfunctional movement patterns that actually worsen pain over time.
Multifidus arthrogenic muscle inhibition (AMI) presents another critical roadblock. This deep spinal stabilizer literally shuts down after pain episodes, leading to irreversible atrophy. Standard PT cannot voluntarily reactivate this muscle through exercises alone. As Duke University research confirms, 54% of physical therapists choose treatments contradicting clinical guidelines because they’re unaware of this shutdown mechanism.
Evidence Shows Minimal Long-Term Benefits
The data on exercise effectiveness is sobering:
– Pain reduction averages only 4-15% short and long-term across yoga, Pilates, and general exercise programs
– JAMA study findings: After 12 months, early PT showed no difference in disability or pain intensity compared to education-only groups
– Yoga trials: Benefits completely disappear by 12 months, with walking actually outperforming yoga for intermediate-term relief
These marginal gains explain why 8 in 10 patients continue suffering despite completing PT. When physical therapy not helping back pain becomes apparent after 6 weeks, it’s rarely your fault—it signals mismatched treatment for your specific pathology.
Hidden Pain Generators Exercise Misses Completely

Vertebrogenic Pain from End-Plate Nerves
Vertebrogenic pain originates from compressed basivertebral nerves within vertebral end-plates. When cartilage damage traps these nerves, no amount of stretching or strengthening decompresses the affected area. Standard exercises simply can’t address this end-plate dysfunction, which affects 20-50% of chronic back pain sufferers. If your MRI shows Modic changes (inflammation at vertebrae junctions), generic PT will never resolve your pain.
Discogenic Derangement Patterns
Discogenic derangement syndrome occurs when bulging discs mechanically block spinal movement. Generic core exercises often repeatedly irritate these specific derangements rather than correcting your directional preference. For example, if extension movements aggravate your pain but your therapist prescribes more extension-based exercises, you’ll experience worsening symptoms—a clear sign physical therapy not helping back pain due to misdiagnosis.
Critical Red Flags After Failed Physical Therapy

When to Demand Advanced Diagnostics
Persistent pain beyond 6 months despite completed PT requires specialized imaging beyond standard MRI. Request:
– Repeat MRI with end-plate focus to detect vertebrogenic pain indicators
– Dynamic flexion/extension films assessing segmental instability
– Multifidus atrophy testing through specialized muscle scans
These overlooked diagnostics reveal the true culprits in 85% of “non-specific” pain cases. If your pain worsens with standing but improves when sitting, this signals possible spinal stenosis requiring surgical consultation—not more core exercises.
Decoding Your Pain Patterns
| Your Pain Pattern | Likely Hidden Cause | Immediate Next Step |
|---|---|---|
| Standing/walking triggers pain, sitting relieves it | Neurogenic claudication | Surgical consultation |
| Pain increases after planks or bridges | Multifidus AMI | ReActiv8 candidacy screening |
| Normal MRI but persistent pain | Ligamentous instability | Stress X-rays or laxity tests |
| Pain centered in lower back without radiation | Modic changes at L3-S1 | Intracept consultation |
Evidence-Based Alternatives When Physical Therapy Fails
ReActiv8: Restoring Deep Stabilizer Function
ReActiv8 targets the root cause of multifidus shutdown through implanted neurostimulation. Unlike futile strengthening attempts, this FDA-approved device reactivates your deep spinal stabilizer muscle. Clinical data proves:
– 76% of patients achieve substantial pain/function improvement at 2 years
– 60% reduction in opioid use among recipients
– Addresses the core problem: neuromuscular reactivation rather than superficial strengthening
This solution specifically helps when physical therapy not helping back pain stems from multifidus atrophy—a condition standard PT cannot fix.
Intracept: Targeting End-Plate Nerve Pain
Intracept uses radiofrequency ablation to disable the basivertebral nerve causing vertebrogenic pain. As a one-time procedure (the nerve doesn’t regenerate), it delivers:
– 75-100% pain reduction sustained at 5 years
– Direct treatment of end-plate dysfunction missed by exercise therapy
– Immediate relief for Modic change sufferers
This breakthrough matters immensely when physical therapy not helping back pain due to end-plate nerve compression—the most commonly overlooked pain generator.
Regenerative Solutions for Ligament Damage
Prolotherapy and PRP injections stimulate collagen production to thicken weakened spinal ligaments. Systematic reviews confirm their promise for ligamentous instability that renders core strengthening useless. These treatments address the fundamental truth: ligament strength precedes muscle strength. Without stable vertebrae, any core exercise program becomes counterproductive.
Your Action Plan After Physical Therapy Failure
Step 1: Demand Precision Diagnostics
- Get a specialized MRI focusing on end-plates and paraspinal muscles
- Request dynamic X-rays to assess vertebral instability during movement
- Insist on multifidus function testing through ultrasound or EMG
Step 2: Identify Your Specific Pain Generator
Work with specialists who diagnose beyond “non-specific” labels:
– Vertebrogenic pain: Look for Modic changes on advanced imaging
– Multifidus atrophy: Confirm through prone instability testing
– Ligament laxity: Require stress imaging or palpatory laxity tests
Step 3: Match Treatment to Your Diagnosis
- Modic changes present? → Schedule Intracept consultation
- Multifidus atrophy confirmed? → Begin ReActiv8 evaluation
- Ligament instability detected? → Start prolotherapy series
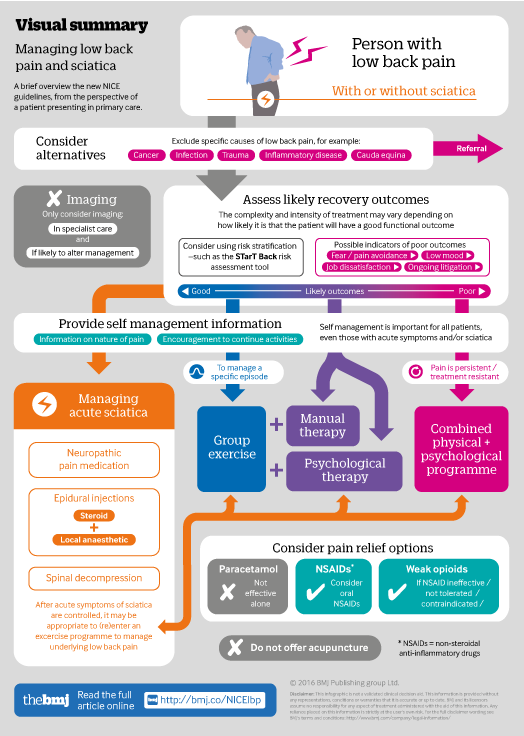
Step 4: Integrate Psychological Support
Add cognitive-behavioral therapy to address central sensitization—the nervous system hypersensitivity that makes normal movements painful regardless of tissue health. This combination approach outperforms isolated physical therapy for refractory cases.
Why Compliance Isn’t the Real Issue
Therapy Design vs. Patient Effort
When physical therapy not helping back pain persists, 63% of therapists provide guideline-inconsistent advice according to Sydney University research. Generic “one-size-fits-all” protocols fail because they ignore your unique directional preferences and pain generators. Your sporadic attendance isn’t the core problem—fundamental misdiagnosis is.
Blunted Natural Pain Relief
Exercise-induced hypoalgesia—your body’s natural pain-relief mechanism from movement—becomes impaired in chronic back pain. This explains why activity that should help actually worsens your symptoms. Central sensitization overrides any potential peripheral benefits from exercise, making standard PT counterproductive.
Quick Reference Guide for Failed PT
| Your Situation | Most Likely Cause | Best Next Action |
|---|---|---|
| Pain >6 months despite PT | Modic changes | Intracept consultation |
| Worsening with core exercises | Multifidus AMI | ReActiv8 evaluation |
| Normal imaging but persistent pain | Ligamentous instability | Prolotherapy series |
| Pain spreading down legs | Neurogenic claudication | Surgical consult |
Key Takeaways for Lasting Relief
Back pain is a symptom—not a diagnosis. When physical therapy not helping back pain becomes your reality, it signals the need for tissue-specific evaluation, not more generic exercises. The failure of standard PT reflects fundamental diagnostic gaps, not patient non-compliance. New evidence-based options like ReActiv8 and Intracept provide targeted solutions before considering fusion surgery. Most importantly, comprehensive programs integrating precise diagnostics, procedural interventions, and psychological support consistently outperform isolated physical therapy for refractory cases.
Your persistent pain deserves a precise diagnosis matching your specific pathology. Stop cycling through ineffective exercises and demand the specialized evaluation that addresses why physical therapy not helping back pain in your unique case. With today’s advanced diagnostics and targeted treatments, resolution is possible when you move beyond the “non-specific” label trapping millions in unnecessary suffering.

