That nagging ache where your lower back meets your hip can transform simple movements into daily challenges. Whether you’re struggling to rise from your desk chair or wincing when rolling over in bed, understanding why these two areas hurt simultaneously is crucial for effective relief. Millions experience this dual pain pattern, often confused about whether their discomfort stems from spinal issues, hip joint problems, or surrounding muscles. This guide cuts through the confusion by revealing the specific connections between your lower back and hip pain, helping you identify your exact cause and take targeted action.
The relationship between your lower back and hips operates on multiple levels—shared nerve pathways, interconnected muscle groups, and biomechanical dependencies. When pain strikes in both areas, it’s rarely coincidence but rather evidence of how these regions function as a single unit. By learning to decode your specific symptoms and their triggers, you’ll gain clarity on whether you’re dealing with muscular imbalances, joint degeneration, or nerve compression. This knowledge empowers you to move beyond temporary fixes toward lasting solutions.
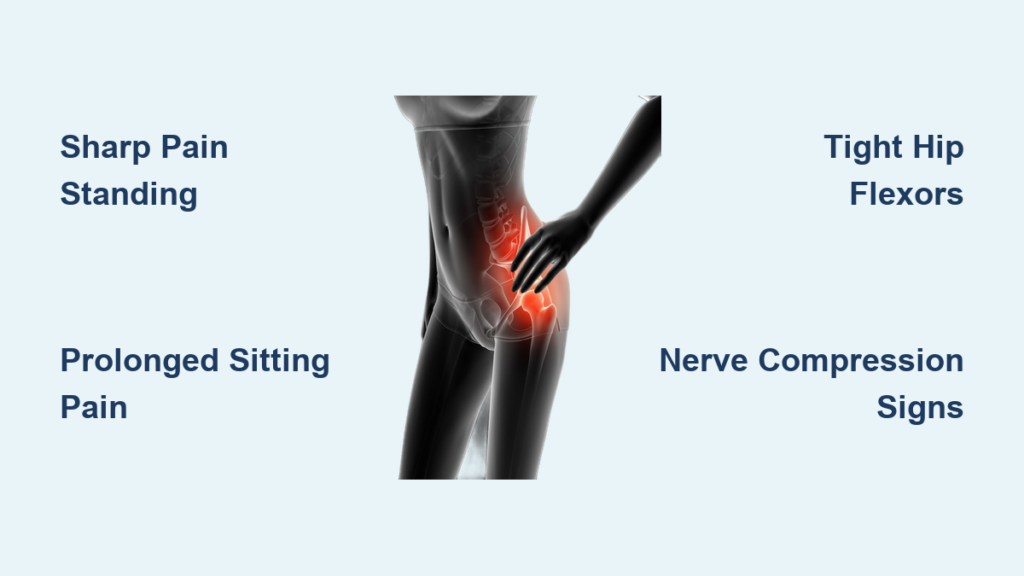
Sharp Pain When Standing Up or Twisting Your Torso
Immediate Pain During Position Changes
That stabbing sensation when transitioning from sitting to standing often signals acute muscle strain or joint impingement. You’ll typically notice this pain localizing to one side of your body and potentially radiating down your outer thigh. The sudden nature of this pain points to specific tissue irritation rather than generalized degeneration.
When you experience this type of pain, examine your movement patterns closely. Does the pain occur primarily when twisting your upper body while your hips remain fixed? This pattern frequently indicates piriformis muscle issues where the muscle compresses the sciatic nerve during rotational movements. Office workers who frequently reach for items while seated often develop this specific pain pattern.
Muscle Spasms Triggered by Sudden Movement
Muscle spasms in your lower back or hip region create intense, localized pain that feels like a “knot” or “cramp.” These involuntary contractions often follow periods of inactivity and worsen with sudden movement. The quadratus lumborum muscle, connecting your lower ribs to your pelvis, frequently spasms in response to poor lifting techniques or sudden twisting motions.
Pro tip: When you feel a spasm coming on, immediately stop the triggering movement and gently shift positions. Applying moist heat for 15-20 minutes can help relax the muscle faster than dry heat. Avoid aggressive stretching during acute spasms as this often worsens the contraction.
Persistent Aching After Sitting or Sleeping

Morning Stiffness That Improves with Movement
Dull, constant pain that feels worse after periods of rest typically indicates inflammatory conditions or muscular tightness. If your discomfort improves within 30 minutes of gentle movement, you’re likely dealing with muscular causes rather than joint degeneration. This pattern commonly affects people who sit for prolonged periods at work, causing hip flexors to tighten and pull the pelvis forward.
The psoas muscle, connecting your spine directly to your femur, often becomes chronically shortened from desk work. This creates anterior pelvic tilt—a forward rotation that increases spinal curvature while simultaneously straining hip structures. You might notice this pain radiating from your lower back around to the front of your hip.
Pain That Worsens After Prolonged Sitting
Hip and lower back pain that intensifies after sitting for more than 30 minutes frequently stems from disc-related issues or sacroiliac joint dysfunction. Unlike inflammatory conditions, this pain doesn’t improve with gentle movement but may require specific positional changes for relief. Many people find temporary relief by standing or walking briefly every half hour.
Critical distinction: If your pain improves when leaning forward (like pushing a shopping cart), spinal stenosis could be the culprit. This condition involves narrowing of the spinal canal and creates a characteristic pattern where extension (standing upright) worsens pain while flexion (bending forward) provides relief.
Weak Glutes and Tight Hip Flexors Creating Pain

How Desk Work Shortens Your Hip Flexors
Prolonged sitting ranks as the top preventable cause of combined lower back and hip pain. When you remain seated for hours, your hip flexor muscles stay in a shortened position while your glute muscles become neurologically inhibited. This creates the perfect pain recipe: tight hip flexors pulling your pelvis forward while weak glutes fail to counterbalance this movement.
The iliacus and psoas muscles (collectively called the iliopsoas) shorten significantly during prolonged sitting. These muscles attach directly to your lumbar spine, so when they tighten, they literally pull your lower vertebrae forward. This altered pelvic position forces your lower back muscles to work overtime to maintain upright posture, leading to chronic strain.
Gluteal Amnesia and Its Pain Consequences
“Gluteal amnesia” describes the neurological disconnect that occurs when your brain stops properly activating your glute muscles due to chronic sitting. When this happens, other muscles—particularly in your lower back—must compensate during basic movements like standing up or climbing stairs. This compensation pattern creates excessive strain on structures not designed for those loads.
Quick test: Lie on your stomach and try lifting one leg off the floor without bending your knee. If you feel this primarily in your lower back rather than your buttock, you likely have gluteal inhibition. This simple test reveals why many people experience back pain during activities that should primarily engage the hips.
Nerve Compression Causing Radiating Pain Patterns
:background_color(FFFFFF):format(jpeg)/images/article/the-sciatic-nerve/06pKhmOUJUczpT9Va1tNsQ_nervus_ischiadicus_large_Zs2JJYnSV675gGpeR0zZw.png)
Sciatica Versus Piriformis Syndrome Differences
Burning, tingling, or electric-like pain traveling from your lower back through your hip and down your leg indicates nerve involvement, but the specific pattern reveals the cause. True sciatica from a herniated disc typically follows a distinct path down the back of your leg to your calf or foot, while piriformis syndrome creates similar symptoms through muscle compression of the sciatic nerve.
The key diagnostic difference lies in what movements trigger your pain. Piriformis syndrome often worsens with prolonged sitting, squatting, or climbing stairs, while disc-related sciatica frequently intensifies with forward bending or coughing. Hip rotation tests can help differentiate these conditions—internal rotation often aggravates piriformis syndrome while external rotation may worsen disc issues.
Identifying Nerve Root Involvement
Specific nerve roots create predictable pain patterns when compressed. L5 nerve root compression causes pain along the outer calf and top of the foot, while S1 compression affects the back of the calf and sole of the foot. You can often identify which nerve is involved by noting exactly where you feel numbness, tingling, or weakness.
Warning sign: If you experience foot drop (trouble lifting the front of your foot) or significant weakness in leg muscles, seek medical evaluation promptly. These symptoms indicate substantial nerve compression that may require more aggressive intervention.
Work Habits That Accelerate Lower Back Hip Pain
Office Workers’ Hidden Risk Factors
Poor ergonomic setups create subtle but significant stressors that accumulate over time. When your chair lacks proper lumbar support, your pelvis rotates backward, flattening your natural spinal curve and transferring stress to your hip joints. Computer monitors positioned too low force you to slouch, further compounding the problem.
The most insidious office habit involves crossing your legs while seated. This position creates asymmetrical pelvic loading where one hip rotates internally while the other stays neutral. Over weeks and months, this seemingly harmless habit leads to significant muscle imbalances and joint stress that manifest as chronic pain.
Standing Desk Missteps to Avoid
Many people switch to standing desks to alleviate back pain but unknowingly create new problems. Standing on hard surfaces without proper footwear transfers excessive force through your hip joints. Leaning on one leg while standing creates the same asymmetrical stress patterns as leg-crossing while seated.
Pro solution: Alternate between sitting and standing every 30 minutes, using a small footrest to shift weight periodically. Wear supportive shoes with cushioning, and consider an anti-fatigue mat that encourages subtle weight shifts. Proper standing posture involves slight knee flexion and a neutral pelvis position—imagine a string gently pulling the crown of your head upward.
Immediate Relief Strategies for Acute Episodes
Targeted Stretching for Quick Pain Reduction
When lower back and hip pain strike simultaneously, specific stretches can provide rapid relief by addressing the interconnected nature of these regions. The kneeling hip flexor stretch with thoracic extension simultaneously lengthens tight hip flexors while restoring proper spinal alignment.
Step-by-step: Kneel on one knee with the other foot forward in a lunge position. Tuck your pelvis under (posterior tilt) to feel the stretch in the front of your hip. Then, gently arch your upper back while reaching the arm on your kneeling side toward the ceiling. Hold for 30 seconds, feeling the stretch travel from your hip through your side body.
Strategic Positioning for Pain-Free Rest
Your sleeping position significantly impacts morning pain levels. Side sleepers should place a pillow between their knees to maintain hip alignment and reduce strain on the lower back. Back sleepers benefit from a pillow under their knees to maintain the natural lumbar curve.
If you wake with significant stiffness, try the “hook-lying” position before getting out of bed: Lie on your back with knees bent and feet flat, then gently rock your knees side to side for 30 seconds. This gentle movement lubricates spinal joints and prepares your body for standing.
Understanding the specific cause of your lower back and hip pain transforms your approach from guessing to targeted action. By recognizing your unique pain patterns—whether they involve sharp movement-triggered pain, persistent aching after rest, or nerve-related symptoms—you gain the power to address the true source rather than just treating symptoms. Remember that lasting relief comes from addressing both the immediate discomfort and the underlying biomechanical issues that created the problem. Start by implementing one targeted strategy from this guide that matches your specific pain pattern, then build additional interventions as your understanding grows. Your path to pain-free movement begins with identifying the precise connection between your lower back and hip discomfort.