That sharp twinge of lower back pain right side above hip in women that flares when you lift your child or twist to grab your coffee cup isn’t normal wear-and-tear. For females, this specific pain zone often signals muscle strain from daily activities or deeper issues like kidney inflammation or gynecological conditions. The critical first step? Recognizing whether your discomfort stems from yesterday’s intense Pilates class or requires urgent medical attention. Most causes respond well to precise interventions once correctly identified—delaying action risks chronic pain cycles.
This guide cuts through confusion with actionable steps to diagnose your specific trigger, immediate relief tactics that actually work, and clear red flags demanding same-day care. Stop guessing and start healing with strategies tailored to female physiology.
Muscle Strains vs. Spinal Issues: Your Pain Decoded

Why Your Quadratus Lumborum Muscle Screams After Exercise
This deep core muscle connecting your spine to hip bones commonly strains during toddler-lifting or improper deadlifts. You’ll feel a persistent ache that intensifies when standing from chairs or rotating your torso. Key identifiers of muscle strain:
– Pain worsens with movement but eases when lying flat
– Tenderness when pressing 2-3 inches above right hip bone
– Relief within 48 hours of rest and ice
– Often follows new exercise routines or heavy lifting
Unlike muscle pain, spinal issues create distinct patterns. A herniated disc at L3-L4 causes sharp shooting pain down your thigh, while sacroiliac joint dysfunction creates localized pain above the hip that flares when climbing stairs or standing on one leg. If coughing intensifies your pain, disc involvement is likely.
Kidney Stone Pain: The Hidden Culprit Behind Flank Aches
Your right kidney sits beneath the ribs, but when blocked by stones, pain radiates to your lower back. This isn’t ordinary soreness—kidney stone pain features:
– Sudden, cramping waves that peak within minutes
– Nausea or vomiting accompanying back pain
– Urinary urgency or blood-tinged urine
– Pain radiating to inner thigh or groin
Unlike muscular pain, kidney-related discomfort persists when lying still and often coincides with fever or chills. Women frequently mistake early kidney infection symptoms for UTIs—it’s why burning urination with back pain requires same-day urine testing.
Gynecological Triggers: When Pain Tracks Your Cycle
Endometriosis implants on pelvic ligaments create cyclical back pain worsening during menstruation. Ovarian cysts cause one-sided lower back pain that may spike during ovulation. Critical signs pointing to gynecological causes:
– Pain intensifies 2-3 days before or during periods
– Deep pelvic pressure during intercourse
– Unexplained spotting between cycles
– Pain correlating with ovulation (mid-cycle)
Unlike musculoskeletal pain, these conditions often cause referred pain to the inner thigh. If your lower back pain right side above hip in women coincides with menstrual changes, track symptoms for one full cycle before your gynecologist visit.
Emergency Warning Signs Women Ignore
When Back Pain Means ER Trip—Not Rest
Don’t dismiss these red flags as “just back pain”:
– Leg weakness making stairs difficult
– Bladder urgency with inability to void
– Fever over 101°F alongside back pain
– Trauma-related pain after falls or accidents
– Nighttime pain preventing sleep for >2 nights
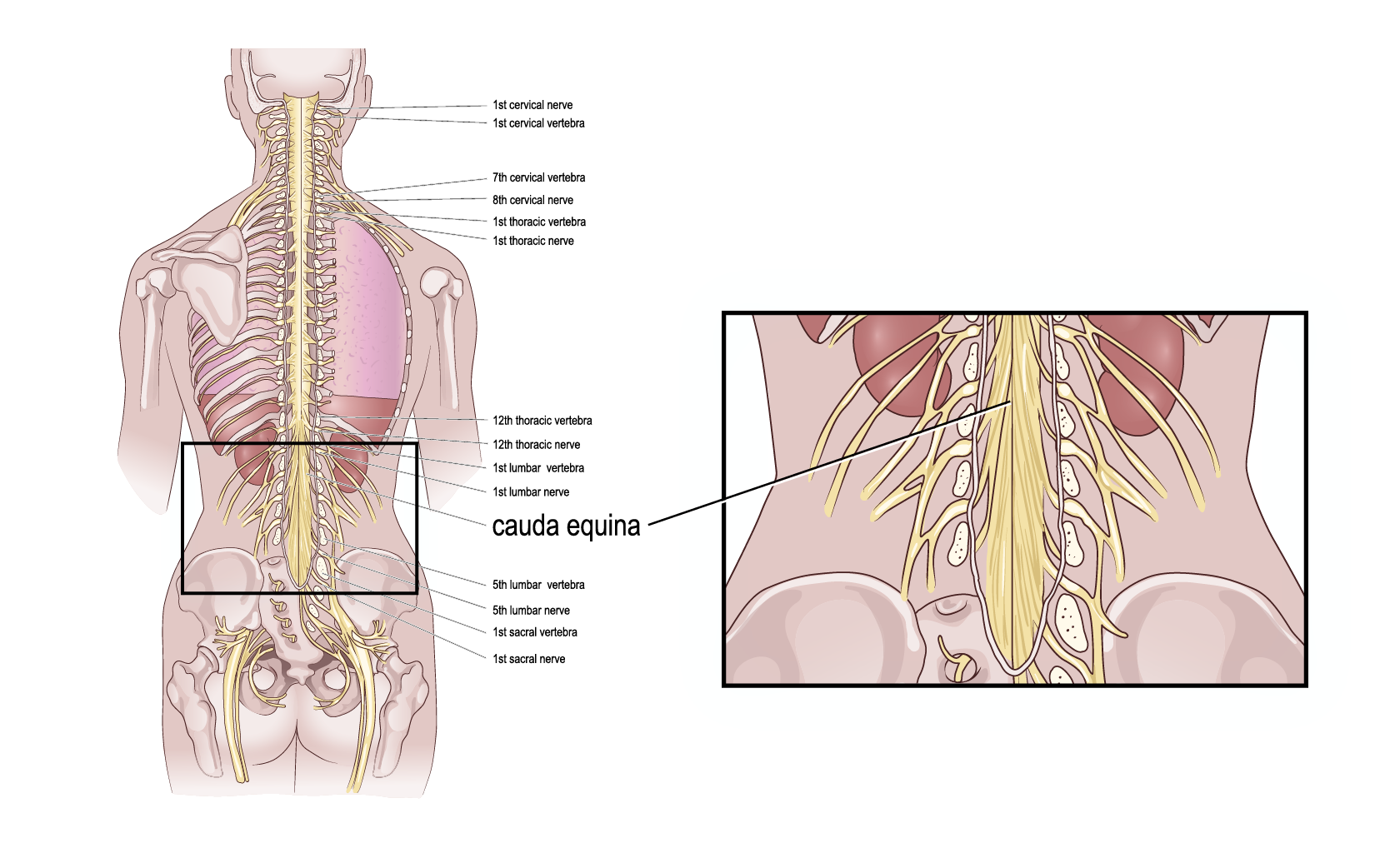
Numbness in your saddle area (inner thighs/buttocks) signals cauda equina syndrome—a surgical emergency. Women often delay care assuming pregnancy-related aches, but sudden severe pain requires immediate evaluation.
Pregnancy-Specific Danger Zones
While 50-80% of pregnant women experience back pain, these symptoms demand same-day OB consultation:
– Rhythmic cramping resembling labor contractions
– Vaginal bleeding with unilateral back pain
– Sudden pain onset in second/third trimester
– Pain preventing walking without support
Right-sided pain could indicate ectopic pregnancy (before 8 weeks) or placental abruption. Never assume “it’s just pregnancy”—report new or worsening pain immediately.
Immediate Home Relief That Targets Female Physiology
First 48 Hours: Precision RICE Protocol
Rest: Limit aggravating activities but avoid bed rest >24 hours—gentle walking prevents stiffness
Ice: Freeze a paper cup of water, peel top, and massage area for 10 minutes every 2 hours
Compression: Wear supportive leggings (not tight waistbands) to stabilize hip muscles
Elevation: Lie on back with knees bent over a pillow to reduce spinal pressure
Skip traditional “compression wraps”—they restrict circulation in women’s wider pelvis. Instead, use a small towel roll under your lower back when sitting.
Heat/Ice Switching Strategy for Hormonal Fluctuations
- Days 1-2: Ice for sharp, acute pain (reduces inflammation from strains)
- Day 3+: Moist heat for dull aches (relaxes muscles tightened by prostaglandins during menstruation)
- Menstrual week: Alternate 15 minutes heat/ice to combat cycle-related inflammation
Pro tip: Add Epsom salts to warm baths—magnesium absorption eases muscle spasms intensified by hormonal shifts.
OTC Medication Tactics for Women’s Bodies
Menstrual-related pain: Take ibuprofen 400mg with food 24 hours before expected period—blocks prostaglandin production
Kidney discomfort: Use acetaminophen (avoid NSAIDs which stress kidneys)
Muscle spasms: Apply topical menthol cream before bed—avoids systemic side effects
Never exceed 3,000mg acetaminophen daily. Women metabolize NSAIDs slower—limit ibuprofen to 1,200mg in 24 hours unless directed otherwise.
Professional Treatment Pathways That Work

What Your Doctor Checks at the Visit
Expect targeted questions about:
– Pain timing relative to menstrual cycle
– Urinary changes (frequency, color, pain)
– Recent lifting or twisting incidents
– Sleep disruption severity
The physical exam includes hip flexor strength tests (prone knee bends) and pelvic floor assessment—not just spinal checks. Bring this to your appointment: A symptom diary tracking pain intensity (1-10), activities, and menstrual dates.
Smart Testing Timeline to Avoid Delays
Week 1: Urinalysis (rules out kidney issues), pelvic exam
Week 2: Ultrasound if gynecological cause suspected
Week 3: MRI only if neurological symptoms present
Skip unnecessary tests: X-rays rarely help for soft tissue pain above the hip
Women often face longer diagnostic delays—insist on urine tests if kidney pain is suspected, even without fever.
Specialist Referral Shortcuts
- Pain with period bleeding? → Gynecologist (endometriosis evaluation)
- Pain with urination? → Urologist (kidney stone assessment)
- Leg numbness? → Orthopedic spine specialist (disc evaluation)
- Chronic pain >6 weeks? → Physical therapist specializing in women’s health
Physical therapy should include pelvic floor assessment—80% of women with chronic lower back pain right side above hip have associated pelvic floor dysfunction.
Prevention That Fits Female Lifestyles
Daily Movement Hacks for Office Workers
- Every 30 minutes: Stand and perform standing cat-cow stretches (hands on desk)
- Lifting technique: Hold toddlers against your hip bone—not your lower back—and bend knees deeply
- Sleep positioning: Place pillow between knees when side-sleeping to align pelvis
- Shoe strategy: Avoid heels >1.5 inches—they tilt pelvis and strain hip muscles
Core Strengthening for Hormonal Fluctuations
Perform these 3x weekly during luteal phase (post-ovulation to period):
– Pelvic tilts: 10 reps holding 5 seconds (activates deep core)
– Bird-dog: 8 reps/side on hands and knees (stabilizes spine)
– Clamshells: 15 reps/side with resistance band (strengthens hip stabilizers)
Skip traditional crunches—they increase intra-abdominal pressure worsening pelvic floor issues.
Next Steps for Lasting Relief
Start with the most probable cause based on your symptoms:
– Post-lifting pain? → Begin RICE protocol + gentle walking for 48 hours
– Pain with urinary symptoms? → Schedule same-day urine test
– Cyclical pain? → Track symptoms for one full menstrual cycle
Persistent lower back pain right side above hip in women rarely resolves alone. Early intervention prevents compensatory movements that create new problems—like left hip strain from favoring your right side. If home care doesn’t improve pain within 72 hours, seek professional evaluation. Your body’s signaling a specific issue; honor it with targeted action today.
Remember: Women’s pain patterns differ from men’s due to pelvic anatomy and hormonal influences. What works for your partner won’t necessarily help you. Trust your instinct—if something feels off, push for answers. With the right approach, that constant ache above your hip can become a distant memory.