That sharp ache in your lower back spreading down into your hip can stop you in your tracks. Whether you’re struggling to stand up from your desk or wincing with every step, this radiating pain affects everything from your morning commute to your evening workout routine. Understanding why lower back pain moves to the hip—and more importantly, what you can do about it—becomes essential for reclaiming your daily activities. Without accurate information, however, self-diagnosis can lead to worsening symptoms or delayed treatment.
This guide addresses the critical need for reliable information about lower back pain that travels to the hip, while acknowledging the significant gap in verified medical resources on this specific symptom pattern. You’ll learn why proper diagnosis matters, what questions to ask your healthcare provider, and how to navigate treatment options safely when your back pain begins radiating toward your hip.
Why Verified Information Matters for Radiating Pain

The Danger of Self-Diagnosis Without Medical Guidance
Lower back pain moving to hip represents a symptom that could stem from multiple underlying causes, each requiring different treatment approaches. Without access to verified medical information, attempting to self-diagnose can lead to inappropriate exercises or treatments that worsen your condition. A pinched nerve requires different management than hip joint arthritis, yet both can cause similar radiating pain patterns. Misidentifying your specific issue might transform a temporary discomfort into a chronic problem.
How Medical Professionals Determine the True Source
Healthcare providers use specific assessment techniques to distinguish between pain originating in the spine versus the hip joint. They evaluate your pain pattern, perform physical tests that isolate different structures, and determine whether your symptoms indicate nerve involvement. This precise diagnosis is crucial because treating hip pain when the problem actually originates in your lower back—or vice versa—wastes valuable recovery time and potentially aggravates your condition.
Recognizing When Symptoms Require Professional Evaluation
Certain pain characteristics should prompt immediate medical consultation rather than home treatment attempts. Pain that moves from your lower back to your hip accompanied by numbness, tingling, or weakness requires professional assessment to rule out nerve compression. Similarly, pain that worsens at night or doesn’t respond to position changes may indicate issues needing specific medical intervention. Ignoring these warning signs while searching for internet-based solutions could delay necessary treatment.
Essential Questions to Ask Your Healthcare Provider
Clarifying Your Specific Pain Pattern
When discussing lower back pain moving to hip with your doctor, be prepared to describe exactly where your pain travels. Does it follow a specific pathway down your leg? Does it feel deep in the hip joint or more superficial? Does certain movements trigger or relieve your symptoms? These details help professionals differentiate between conditions like sciatica, sacroiliac joint dysfunction, or actual hip pathology—all of which cause similar radiating pain but require different treatments.
Understanding Diagnostic Testing Options
Ask your healthcare provider which diagnostic tests might clarify your specific situation. While X-rays show bone structure, they won’t reveal soft tissue or nerve issues. MRI provides more comprehensive information about discs, nerves, and soft tissues but isn’t always necessary initially. Understanding why certain tests are recommended—and which might be unnecessary for your specific presentation—helps you make informed decisions about your care without undergoing excessive procedures.
Establishing Realistic Treatment Expectations
Inquire about the typical recovery timeline for your diagnosed condition and what milestones indicate progress. Lower back pain moving to hip might resolve in weeks for some conditions but require months of management for others. Knowing what to expect prevents frustration when improvement doesn’t follow an unrealistic timeline. Also, ask about warning signs that indicate your condition is worsening rather than improving, so you know when to seek additional help.
Safe Initial Steps While Waiting for Professional Consultation

Positioning Strategies That Reduce Nerve Pressure
While waiting for your medical appointment, certain positions may provide temporary relief without risking further injury. Lying on your back with knees bent and supported by pillows reduces pressure on lumbar nerve roots. If this position increases discomfort, try lying on your side with a pillow between your knees to maintain spinal alignment. Avoid positions that intensify your pain, as these likely aggravate the underlying issue causing your lower back pain to move toward your hip.
Movement Modifications for Daily Activities
Adjust how you perform basic movements to minimize strain during acute phases. When rising from sitting, pivot your entire body rather than twisting at the waist. When lifting objects, bend at the knees while keeping your back straight—not the reverse. For sleeping, experiment with positions that don’t radiate pain toward your hip, typically avoiding stomach sleeping which increases spinal stress. These modifications prevent additional strain while you await professional guidance.
What NOT to Do with Radiating Pain
Avoid aggressive stretching or massage in the painful area without professional guidance, as this might worsen nerve irritation. Don’t ignore persistent pain hoping it will resolve on its own, especially when it moves from your lower back to your hip—a sign of potential nerve involvement. Resist following generic exercise routines found online, as movements appropriate for one condition might aggravate another. Patience during proper diagnosis prevents creating additional problems while treating the wrong issue.
Building a Collaborative Treatment Plan
Why Treatment Must Address the Source, Not Just Symptoms
Effective management of lower back pain moving to hip requires identifying and treating the underlying cause, not just masking discomfort. If nerve compression causes your radiating pain, strengthening exercises alone won’t resolve the issue. If hip joint problems refer pain to your back, spinal manipulation might provide temporary relief but won’t fix the hip dysfunction. A comprehensive treatment plan addresses both symptom management and the root cause to prevent recurrence.
Integrating Professional Guidance with Home Care
Work with your healthcare provider to develop a home care routine that complements professional treatments. This might include specific stretches to perform multiple times daily, activity modifications for your work environment, and gradual reintroduction of movement as symptoms improve. The most successful outcomes occur when patients consistently follow professionally designed protocols rather than mixing advice from multiple unverified sources.
Tracking Progress to Inform Ongoing Treatment
Keep a simple symptom journal noting pain intensity, locations, and activities that affect your lower back pain moving to hip. Rate your pain daily on a 1-10 scale and record what makes it better or worse. This information provides valuable data for your healthcare provider to adjust treatment as needed. Objective tracking prevents misjudging improvement based on temporary good days or overestimating severity during flare-ups.
Recognizing When to Seek Specialized Care
Identifying Red Flags Requiring Immediate Attention
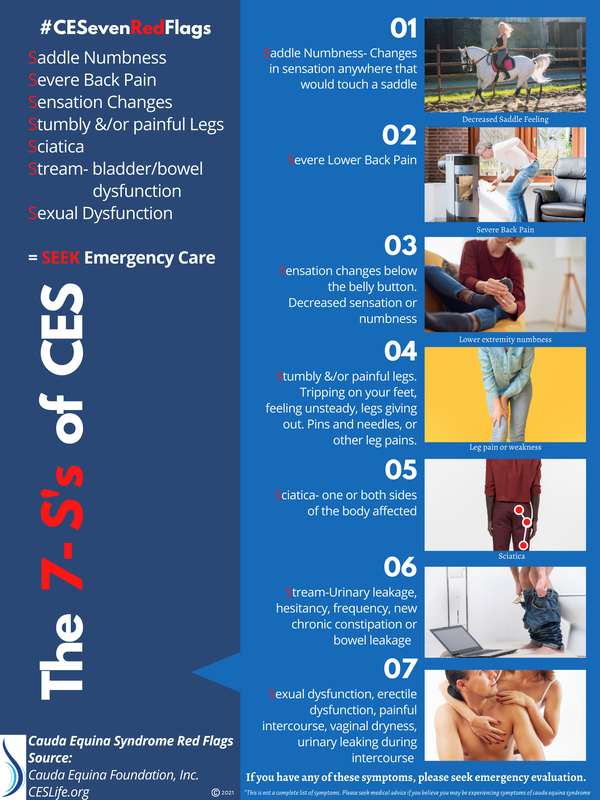
Contact your healthcare provider immediately if you experience loss of bowel or bladder control, progressive leg weakness, or numbness in the saddle area (groin and inner thighs) along with your lower back pain moving to hip. These symptoms indicate potential cauda equina syndrome, a rare but serious condition requiring urgent intervention. Similarly, fever accompanying back pain or unexplained weight loss with radiating pain warrants prompt medical evaluation.
Knowing When to Request Specialist Referral
If your symptoms don’t improve after 2-4 weeks of appropriate conservative treatment, ask about referral to a spine specialist or physical therapist with expertise in lower back and hip conditions. Persistent radiating pain beyond this timeframe often requires more specialized assessment and treatment. A second opinion can provide valuable perspective when standard approaches haven’t resolved your lower back pain moving to hip.
Understanding Advanced Treatment Options
When conservative approaches don’t resolve your symptoms, discuss advanced options with your provider. These might include targeted injections to both diagnose and treat specific pain generators, specialized physical therapy techniques for nerve mobilization, or in rare cases, surgical consultation. Understanding these options helps you participate actively in treatment decisions rather than feeling overwhelmed by unfamiliar terminology during critical discussions.
Key Takeaway: Lower back pain moving to hip requires professional evaluation to determine the true source and appropriate treatment path. While temporary relief strategies can help during the initial phase, long-term resolution depends on accurate diagnosis and targeted treatment addressing the underlying cause. The most successful outcomes occur when patients partner with healthcare providers, follow evidence-based protocols, and avoid self-treatment based on incomplete or unverified information. Always prioritize professional medical guidance over online suggestions when dealing with radiating pain patterns that could indicate nerve involvement or serious underlying conditions.

