Waking up with nagging lower back pain after hip replacement surgery can feel like trading one problem for another. While most patients expect hip pain relief, that persistent ache in your lumbar spine might come as an unwelcome surprise. Here’s the good news: clinical research shows total hip replacement effectively reduces lower back pain in 94% of patients, and when it doesn’t resolve naturally, targeted treatments deliver relief.
This guide walks you through proven strategies to eliminate lower back pain following hip surgery, from immediate post-operative care to long-term solutions based on extensive clinical data. You’ll discover why lower back pain occurs after hip replacement and exactly what you can do to accelerate your recovery.
Immediate Post-Surgery Relief Strategies
First 48 Hours: Positioning and Ice Therapy
Sleep positioning makes or breaks your recovery. Place a pillow between your knees when lying on your non-surgical side, or use a wedge pillow under your knees when lying on your back. This reduces lumbar spine stress while your hip heals. The optimal position maintains spinal alignment without putting pressure on your new hip joint.
Apply ice packs to your lower back for 15-minute intervals, 3-4 times daily. Research shows this reduces inflammation that often radiates from surgical trauma. Never place ice directly on skin—wrap in a thin towel first. This simple technique helps manage the 4.13 average pre-op lower back pain score that drops to 1.90 within weeks after surgery.
Pain Medication Timing Protocol
Take medications before pain escalates. Prescribed anti-inflammatories work best when taken consistently, not just when pain spikes. Set phone reminders for medication intervals during the first week post-surgery. This prevents pain cycles that trigger muscle spasms in your lower back.
Avoid over-the-counter NSAIDs beyond what’s prescribed—excessive inflammation reduction can slow bone healing around your new hip joint. Your surgeon carefully balanced this equation to maximize healing while minimizing discomfort.
Movement Patterns That Reduce Lumbar Stress
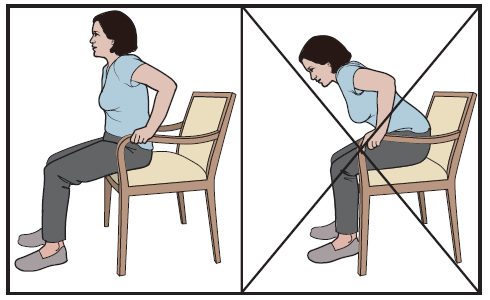
Safe Transitions from Sitting
Master the 90-90 rule. When rising from chairs, ensure both feet and knees form 90-degree angles. This prevents lumbar twisting that aggravates post-surgical back pain. Many patients unknowingly strain their lower back during these transitions, undoing hours of careful recovery work.
Step-by-step transition technique:
1. Slide forward to chair edge
2. Place surgical leg slightly forward
3. Push up using armrests, keeping back straight
4. Pause briefly before taking first step
Walking Progression Guidelines
Start with 5-minute walks, 3-4 times daily. Increase by 2 minutes each day until reaching 30 minutes continuously. Use a walker or cane as directed—limping increases lower back strain dramatically. Clinical data shows consistent walking patterns significantly improve both hip function (from 45.33 to 86.44 on Harris Hip Score) and lower back pain.
Red flags to stop walking immediately:
– Sharp lower back pain above 4/10
– Numbness or tingling down legs
– Sudden weakness in surgical leg
Physical Therapy Exercises That Work
Week 1-2: Gentle Lumbar Mobility
Ankle pumps prevent stiffness. While lying down, flex and point your feet 20 times each hour. This pumps blood through your lower back muscles without stressing your hip. These micro-movements maintain circulation critical for healing.
Pelvic tilts restore alignment. Lie on your back with knees bent. Gently flatten your lower back into the bed, hold 3 seconds, release. Repeat 10 times, 3 sets daily. This simple movement reestablishes proper pelvic positioning that supports both your new hip and lumbar spine.
Week 3-4: Strengthening Foundation
Bridge progression builds support:
– Basic bridge: Lift hips while keeping shoulders down
– Single-leg bridge: Extend one leg while bridging
– Hold each position 5 seconds, 10 repetitions
Clamshells protect lumbar spine:
Lie on non-surgical side with knees bent. Keeping feet together, lift top knee like opening a clamshell. This strengthens glutes that support both hip and spine. Strong glutes prevent compensatory movements that strain your lower back.
When Pain Persists: Diagnostic Pathways
Identifying Red Flag Symptoms
Seek immediate evaluation if you experience:
– Progressive weakness in legs
– Loss of bowel or bladder control
– Severe pain unresponsive to medication
– Fever with increasing back pain
These symptoms could indicate serious complications requiring prompt attention. While 94% of patients see significant improvement, approximately 5.9% (9 out of 153 in clinical studies) experience persistent or worsening lower back pain after hip replacement.
Imaging That Reveals Hidden Issues
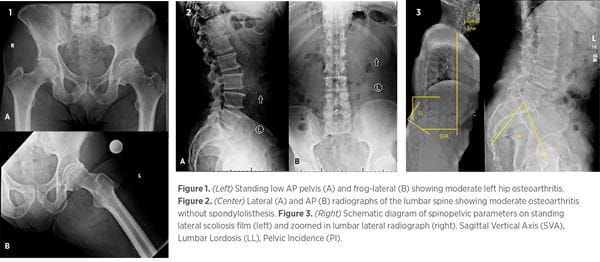
Persistent pain beyond 6 weeks requires investigation. MRI scans identify residual disc herniations or spinal stenosis missed during initial hip evaluation. Research shows 6% of patients need targeted spinal treatment after hip replacement. Diagnostic imaging helps determine if your lower back pain stems from the hip surgery or pre-existing spinal conditions.
X-ray findings to discuss with your surgeon:
– Implant positioning affecting spinal alignment
– Leg length discrepancies causing lumbar compensation
– Bone healing patterns around prosthetic components
Non-Surgical Treatment Options
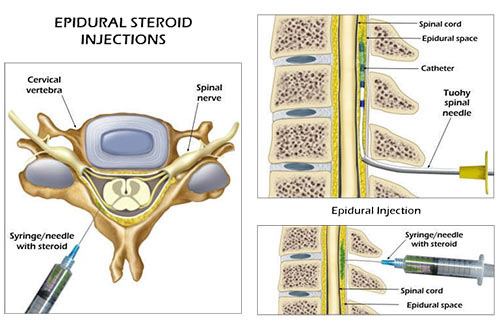
Targeted Injection Therapy
Epidural steroid injections provide relief for patients with confirmed nerve root compression. Success rates reach 83% in recent studies, often eliminating need for additional surgery. These injections target specific pain generators in your lumbar spine that may have become irritated during recovery.
Facet joint injections address arthritis pain at specific spinal levels. These diagnostic injections confirm pain sources before considering permanent treatments. For the small percentage of patients who don’t achieve complete relief from hip replacement alone, these targeted approaches offer significant improvement.
Professional Therapy Modalities
Manual therapy techniques from certified therapists restore normal spinal mechanics. Focus areas include:
– Sacroiliac joint mobilization
– Lumbar segmental stabilization
– Soft tissue release for compensating muscles
Dry needling releases trigger points in lower back muscles that compensate for hip surgery. Most patients require 4-6 sessions for lasting relief. These specialized techniques address the muscle imbalances that develop when your body adapts to hip surgery.
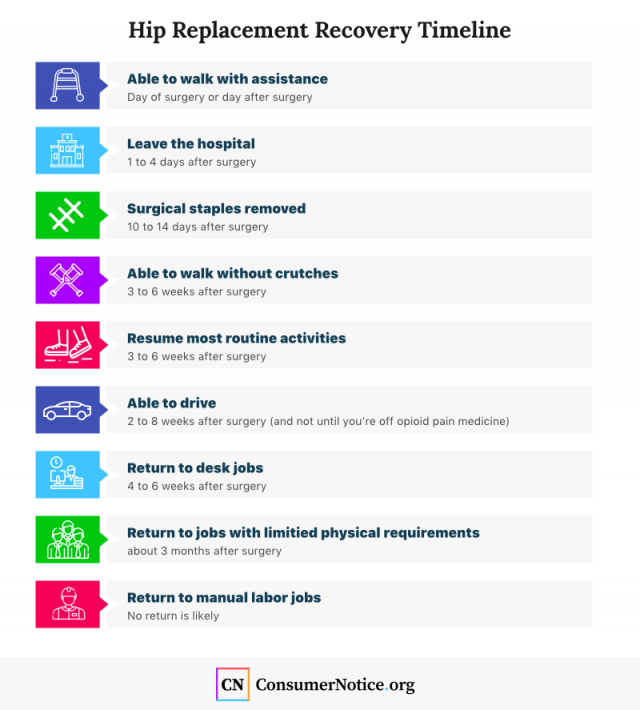
Recovery Timeline Expectations
Realistic Milestone Mapping
Week 1-2: Expect significant pain reduction as surgical inflammation subsides. Lower back pain often decreases dramatically as hip mechanics improve. This aligns with clinical data showing VAS scores dropping from 4.13 to nearly half that within weeks.
Month 1-3: Gradual improvement continues. Most patients report 50-70% back pain reduction by 6 weeks. Continue exercises consistently—even when pain improves. The Harris Hip Score typically jumps from 45 to 86 during this period, reflecting dramatic functional improvement.
Month 3-6: Final healing phase. By 6 months, 94% of patients experience minimal or no lower back pain. Persistent cases merit specialist evaluation. Long-term follow-up shows average recovery at 44.3 months with zero complications in the study group.
Activity Return Schedule
Driving: Resume when you can brake without hesitation—typically 2-4 weeks post-surgery. Start with short trips.
Work: Sedentary jobs return at 2-4 weeks with standing breaks every 30 minutes. Physical jobs require 6-12 weeks clearance.
Exercise: Low-impact activities like swimming and cycling resume at 6-8 weeks. High-impact sports require 3-6 months healing.
Key Success Factors Summary
Your lower back pain after hip replacement isn’t permanent—94% of patients achieve lasting relief through natural healing, targeted exercises, and occasional medical intervention. Focus on consistent physical therapy, proper movement patterns, and patience with your body’s healing timeline.
Remember these critical points:
– Most back pain resolves within 6 months naturally
– Persistent pain beyond 6 weeks warrants specialist evaluation
– Targeted treatments succeed in 83% of persistent cases
– Daily exercises prevent recurrence long-term
Follow this roadmap, and you’ll likely join the majority of patients who eliminate lower back pain while enjoying their new hip’s benefits. For the small percentage who need additional care, subsequent lumbar surgery delivers pain relief in 83% of cases, ensuring comprehensive recovery regardless of your specific situation. Your path to pain-free movement starts with understanding these evidence-based strategies and implementing them consistently throughout your recovery journey.

