That sharp leg pain shooting down your calf isn’t just “bad back trouble”—it’s likely your herniated disc pressing on a nerve root. If you’re between 20-50 and suddenly can’t sit through a meeting without radiating discomfort, you’re not alone. Eighty percent of people battle low back pain, and herniated discs rank as a top culprit in this age group. The critical news? Only 10% ever need surgery. With the right back exercises for herniated disc pain, most find significant relief in 6-8 weeks and full recovery within 3-4 months. This guide delivers precise, evidence-based moves that reduce nerve pressure, strengthen your spinal armor, and get you moving without risking further damage.
Why Your Herniated Disc Causes Leg Pain (Not Just Back Pain)
Your spinal discs function like jelly-filled donuts—tough outer rings (annulus fibrosus) containing a soft center (nucleus pulposus). When the outer layer tears, the inner gel bulges outward and compresses nearby nerves. This triggers radiating leg pain below the knee, tingling, or weakness—often worse than your original backache. Sitting, forward bending, coughing, or twisting intensifies symptoms by squeezing the disc further onto nerves. Crucially, imaging alone doesn’t diagnose pain; your symptoms must match the herniation location. If you feel pain shooting into your foot when bending to tie shoes, that’s your nerve signaling disc trouble.
Critical Safety Rules Before Doing Herniated Disc Exercises
Stop immediately if pain shoots below the knee—this “peripheralization” means you’re worsening nerve compression. Success looks like centralization: leg pain retreating toward your spine. Follow these non-negotiable rules:
- Warm up first: 5-minute walk or heat pack on lower back
- Never hold your breath: Inhale during prep, exhale during exertion
- Avoid “no pain, no gain”: Stay within pain-free range
- Frequency beats duration: Do exercises 1-2x daily, not marathon sessions
- Emergency stop signs: Numbness, leg weakness, or bowel/bladder changes require immediate medical care
Skipping these steps risks turning a manageable herniation into chronic nerve damage. If you feel electric shocks during an exercise, revert to the previous progression.
30-Second Spinal Decompression Moves for Instant Relief
These techniques create space between vertebrae, reducing disc pressure on nerves within minutes.
Doorway Hanging Traction
Stand under a sturdy doorframe pull-up bar. Grip with palms facing forward, arms straight. Let your body hang while keeping shoulders relaxed. Lightly touch toes to the floor if needed to control intensity. Hold 30 seconds, rest 30 seconds, repeat 3 times. Pro tip: Release by bending knees—never drop suddenly—to prevent muscle spasms.
Supine Towel Decompression (No Equipment Needed)
Lie flat on your back near a doorway. Loop a bath towel under both feet. Gently pull the towel ends toward your chest until you feel a mild stretch along your spine—not pain. Hold 60 seconds while breathing deeply into your ribs. Repeat twice. Warning: Stop if leg pain increases; this isn’t stretching your hamstrings.
McKenzie Extensions That Centralize Leg Pain

These evidence-backed moves encourage the herniated gel to retreat inward, reducing nerve pressure.
Prone Resting on Belly (First Step for Acute Pain)
Lie face-down with a pillow under your hips if needed. Rest forehead on stacked hands. Relax completely for 2 minutes—do not lift your chest. This position naturally shifts disc material away from nerves. Stop immediately if leg pain intensifies; try towel decompression instead.
Sphinx Position for Moderate Herniations
From prone position, slide elbows under shoulders. Press through forearms to lift your chest 2-4 inches while keeping pelvis glued to the floor. Hold 10-30 seconds, lower slowly. Repeat 10 times hourly when pain flares. Key: Keep lower ribs heavy—arching here worsens symptoms.
Standing Back Extensions for Desk Workers
Stand tall with hands on your lower back. Gently push hips forward while tilting your gaze toward the ceiling. Hold 3 seconds, return to neutral. Complete 10 reps every hour you sit. Why it works: Counters spinal compression from prolonged sitting better than lying extensions.
Core Stability Exercises That Shield Your Herniated Disc

Weak core muscles force discs to bear excess load. These moves build a natural “corset” around your spine.
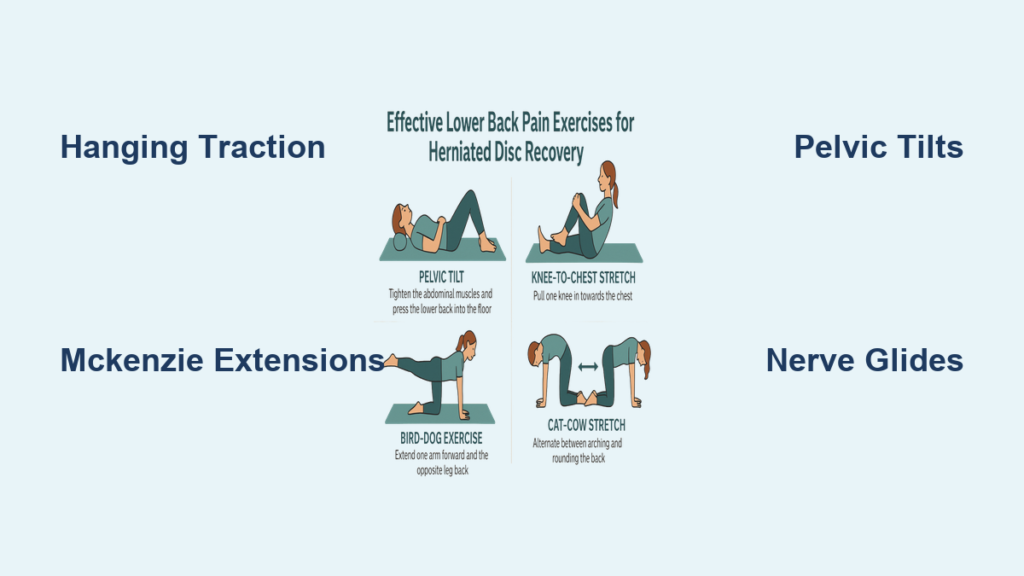
Pelvic Tilts for Immediate Spinal Relief
Lie on your back with knees bent. Tighten lower abs to flatten your lower back into the floor. Hold 5 seconds, relax. Perform 15 reps 3x daily. Visual cue: Imagine zipping a tight pair of jeans—you should feel deep lower abdominal engagement, not hip flexor strain.
Glute Bridges to Reduce Nerve Pressure
Lie on your back, feet flat hip-width apart. Squeeze glutes to lift hips until shoulders, hips, and knees form a straight line. Hold 2 seconds, lower slowly. Do 12 reps × 2 sets. Mistake to avoid: Arching your lower back at the top—this shifts pressure to the herniated disc.
Forearm Plank for 24/7 Spinal Protection
Prop on forearms and toes, body straight from head to heels. Engage abs and glutes. Hold 20 seconds. Rest 30 seconds. Repeat 3 times. Progression: Lift one foot 1 inch off the floor for 5 seconds per side once pain-free.
Nerve-Safe Hamstring and Piriformis Stretches
Tight hamstrings pull your pelvis out of alignment, increasing disc stress. These modifications prevent nerve aggravation.
Seated Chair Hamstring Stretch (No Floor Needed)
Sit tall in a chair. Place one heel on a low stool, knee straight. Hinge forward at hips (not waist) until you feel a gentle pull behind the thigh. Hold 8 seconds. Repeat 3x per leg. Critical: Keep your chest lifted—slumping forward compresses discs.
Supine Piriformis Stretch for Buttock Pain
Lie on your back. Cross the ankle of your painful leg over the opposite knee. Grasp the uncrossed thigh and pull it toward your chest until you feel a stretch in the buttock—not the knee. Hold 12 seconds × 5 reps. Stop if: Pain radiates down the leg.
Sciatic Nerve Glides to Reduce Tingling
Stiff nerves worsen herniation symptoms. This technique mobilizes nerves without stretching.
Supine Nerve Flossing Technique
Lie on your back. Flex one hip to 90 degrees. Grasp behind the thigh (not knee). Slowly straighten the knee until you feel tension—not pain—in your leg. Hold 2 seconds, then bend the knee. Repeat 15 times for 2 minutes. Sign of success: Tingling decreases during the movement.
Movement Patterns That Worsen Herniated Discs (Stop Doing These)
Loaded spinal flexion is the #1 exercise mistake. Avoid these until cleared by a physical therapist:
- Sit-ups and crunches: Increase disc pressure by 200% when performed lying down
- Deadlifts and deep squats: Compress discs under heavy load
- Prolonged sitting: >30 minutes without extension breaks
- Aggressive toe touches: Forces nucleus material posteriorly
- Running on hard surfaces: High-impact jarring worsens nerve irritation
Safer alternatives: Swimming instead of running, wall sits instead of deep squats, seated marching instead of crunches.
Daily Micro-Habits to Prevent Flare-Ups
Integrate these into your routine without extra time:
- Every 30 minutes of sitting: Stand and perform 2 standing back extensions
- Driving: Place a lumbar roll behind your lower back to maintain spinal curves
- Sleeping: Back sleepers—use pillow under knees; side sleepers—place pillow between knees
- Lifting: Hinge at hips (not waist), keep objects against your body, exhale while lifting
- Pain spikes: Apply heat for 15 minutes before moving, ice for 10 minutes after
Pro tip: Set phone reminders for hourly extension breaks during desk work—this prevents cumulative disc compression.
When to Call a Physical Therapist Immediately
Seek professional help if you experience:
- Foot drop: Tripping when walking due to weak dorsiflexion
- Saddle numbness: Loss of sensation in inner thighs/buttocks
- Bowel/bladder dysfunction: Incontinence or retention
- Progressive weakness: Leg giving way when climbing stairs
- No improvement: After 6 weeks of correct exercise
A physical therapist will customize your program using directional preference testing—finding the exact movement that centralizes your pain. They may add manual traction or neuromobilization techniques beyond home exercises.
Consistency with these back exercises for herniated disc pain delivers faster results than intensity. Start today with 2 minutes of prone resting and 10 standing extensions hourly. Track your symptoms: each millimeter that pain retreats toward your spine signals healing. Within 4 weeks, most replace sharp leg pain with manageable stiffness. By week 8, 85% resume normal activities without restrictions. Never push through nerve pain—your disc heals best with precise, pain-free movement. Stick to these evidence-based exercises, and you’ll transform “I can’t sit through dinner” to “I forgot I had a herniation” within months.