That sharp twinge between your shoulder blades after dinner isn’t just bad luck—it’s your body signaling something deeper. Back pain after eating affects millions daily, yet most people dismiss it as poor posture or overeating. When your meal transforms into mid-back agony or lower spine discomfort, your digestive system is sending urgent signals that demand attention.
Understanding why this happens transforms random suffering into manageable, treatable symptoms. This guide reveals the hidden connections between your digestive system and back pain after eating, plus proven strategies to stop the cycle before your next meal.
GERD’s Hidden Back Pain Connection
How Acid Reflux Targets Your Spine
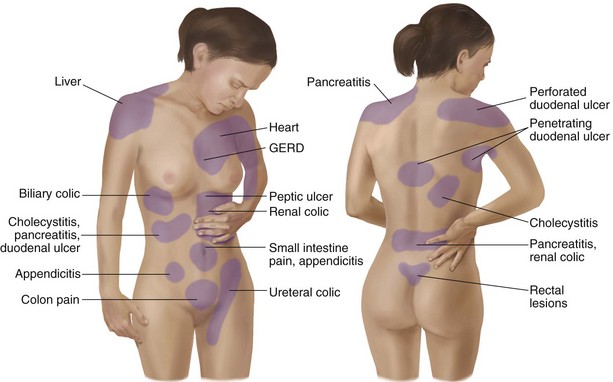
When stomach acid flows backward into your esophagus after eating, the burning sensation doesn’t stay confined to your chest—it radiates directly to your upper back. Your lower esophageal sphincter acts like a faulty door, letting acid splash upward when you consume trigger foods or lie down too soon after meals.
Spot GERD-related back pain with these telltale signs:
– Burning sensation starts in chest then spreads between shoulder blades
– Pain worsens when bending over or lying flat within 30 minutes of eating
– Relief comes quickly when sitting upright
– Sour taste in mouth typically accompanies the back discomfort
Quick Acid Reflux Relief That Works Tonight
Immediate actions when pain strikes:
– Sit upright for at least 30 minutes—no slouching allowed
– Take a gentle 10-minute walk to stimulate digestion
– Apply a heating pad set to medium on painful areas for 20 minutes
– Mix 1 teaspoon of baking soda in 8 ounces of water for natural relief
Critical mistake to avoid: Never take ibuprofen or other NSAIDs when experiencing back pain after eating—they worsen stomach lining irritation and could trigger ulcers.
Gallbladder Attacks: Why Fatty Foods Trigger Back Pain

Recognizing Your Gallbladder’s Warning Signs
That pizza you enjoyed last night might be the culprit behind your sudden right shoulder blade pain. Your gallbladder contracts to release bile after fatty meals, but when gallstones block this process, the resulting pressure creates sharp pain under your right ribs that radiates directly to your back.
Classic gallbladder attack pattern:
– Severe upper right abdominal pain peaks 30-60 minutes after eating
– Pain shoots through to right shoulder blade or mid-back
– Nausea often follows the meal
– Symptoms typically last 1-5 hours before gradually subsiding
Emergency Gallbladder Pain Protocol
If you suspect gallbladder issues:
1. Stop eating immediately and avoid lying down
2. Apply cold compress to upper right abdomen (not back)
3. Sip small amounts of ginger tea to calm nausea
4. Note the exact time pain started for medical evaluation
Red flag symptoms requiring ER visit: Fever over 101°F, yellowing of skin/eyes, or pain lasting more than 6 hours without relief.
Ulcer-Induced Back Pain: When Stomach Sores Radiate
Identifying Your Ulcer Pain Pattern
Open sores in your stomach lining become aggravated by food, creating referred pain that shoots through to your back. Duodenal ulcers typically cause mid-back pain, while gastric ulcers create upper back discomfort between the shoulder blades—often 2-3 hours after your meal.
Ulcer warning indicators that need medical attention:
– Burning stomach pain that wakes you at night
– Temporary relief after taking antacids
– Unexplained weight loss despite normal eating
– Dark, tarry stools indicating internal bleeding
Ulcer-Friendly Eating Strategy
Transform your meal timing to prevent pain:
– Switch to 5-6 small meals instead of 3 large ones
– Stop eating 3 hours before bed to allow stomach rest
– Chew each bite 20-30 times to reduce digestive burden
– Eat slowly—your meal should take at least 20 minutes
Sample ulcer-safe dinner: Baked salmon with steamed carrots and quinoa, followed by banana instead of acidic dessert.
Posture Problems That Turn Meals Into Back Pain

How Your Eating Position Triggers Discomfort
Slouching over your plate compresses your spine for 20-30 minutes straight, irritating existing conditions. This mechanical pressure creates lower back pain or tension between your shoulder blades, particularly during long meals or when eating at low tables.
Quick posture fixes during meals:
– Sit with feet flat on floor (use stool if needed)
– Keep shoulders relaxed but upright—imagine a string pulling your head toward ceiling
– Bring food to mouth, not head to plate
– Use chairs with proper lumbar support or add a small cushion
When Back Pain After Eating Signals Emergency
Life-Threatening Conditions Requiring Immediate Care
Some back pain after eating indicates serious medical emergencies. Learn to distinguish routine discomfort from conditions needing ER attention within hours.
Seek emergency care immediately for:
– Severe pain with fever over 101°F
– Black or bloody stools
– Chest pain that may indicate heart issues
– Jaundice (yellow skin or eyes)
– Inability to keep food down for 24+ hours
Smart Symptom Tracking for Doctor Visits
Keep a simple 7-day log:
– Time pain starts after eating (immediate, 30 min, 2 hours)
– Specific foods consumed (be precise: “2 slices pepperoni pizza”)
– Pain location and intensity (1-10 scale)
– Associated symptoms like nausea or heartburn
– What provides relief (position changes, medications)
Bring this log to your doctor—it’s worth more than vague descriptions and gets you proper diagnosis faster.
Immediate Relief Strategies That Work Within Minutes
Position and Movement Fixes
Do this now when pain hits:
– Sit upright for 30 minutes minimum
– Gentle 10-minute walk promotes digestion
– Apply heat to painful areas for 20 minutes
– Elevate upper body 45 degrees if resting
Never do this: Lie flat within 3 hours of eating, bend over to pick things up, wear tight clothing around waist, or take NSAIDs like ibuprofen.
Fast-Acting Medication Guide
Safe over-the-counter options:
– Antacids (Tums, Rolaids) for immediate acid relief
– H2 blockers (Pepcid) for longer-lasting effects
– Simethicone for gas-related discomfort
– Acetaminophen for pain (avoid NSAIDs)
Pro tip: Keep a small emergency kit in your car with antacids, ginger chews, and a heating pad for unexpected pain after restaurant meals.
Dietary Changes That Eliminate Back Pain After Eating
Top 5 Trigger Foods to Cut Immediately
Eliminate these first for quick relief:
– Fried foods and high-fat meats (pizza, burgers)
– Citrus fruits and tomato-based sauces
– Coffee and caffeinated beverages
– Carbonated drinks causing bloating
– Chocolate and peppermint (relax esophageal sphincter)
Sample Day Without Trigger Foods
Breakfast: Oatmeal with banana and almond milk (no dairy)
Snack: Apple with small handful of almonds
Lunch: Grilled chicken with steamed vegetables (no tomatoes)
Snack: Low-fat yogurt (if dairy tolerated)
Dinner: Baked fish with sweet potato and green beans
Special note for pregnant women: Smaller, more frequent meals prevent both heartburn and back strain as your baby grows—add an extra snack mid-afternoon.
Long-Term Prevention Strategies That Last
Daily Habits That Prevent Flare-Ups
Morning routine:
– Start with warm water and lemon (not citrus juice)
– Light stretching before breakfast
– Eat largest meal midday when digestion is strongest
Evening wind-down:
– Gentle walk after dinner
– Elevate head of bed 6-8 inches
– Avoid screens during meals to eat mindfully
Building Your Trigger-Free Kitchen
Pantry staples for pain-free meals:
– Ginger tea for inflammation
– Oatmeal for gentle fiber
– Low-fat proteins (chicken, fish)
– Non-citrus fruits
– Whole grain options
Emergency backup plan: Keep antacids in car and at work, identify “safe” restaurants near home/work, prepare grab-and-go snacks for busy days.
Final Takeaway
Back pain after eating rarely resolves on its own, but targeted changes bring dramatic relief within weeks. Start with the immediate relief steps, then systematically eliminate trigger foods while building supportive habits. Most people see 50-70% improvement within 30 days using these strategies.
Your next meal doesn’t have to end in back pain. By understanding your specific triggers and implementing these proven techniques, you can enjoy food without the aftermath. Remember: persistent or worsening pain requires professional evaluation to rule out serious conditions. Your back—and your digestive system—will thank you for taking action today.

