That sharp stab in your lower left back isn’t just “normal pregnancy discomfort”—it’s your body signaling how dramatically your baby’s growth reshapes your biomechanics. Nearly 70% of pregnant women experience this specific left-sided ache, often intensifying after week 20 as your uterus expands and hormones surge. The culprit? Your uterus naturally shifts rightward, placing uneven strain on left-side muscles and joints. But here’s the empowering truth: most cases respond rapidly to targeted strategies you can implement today. This guide reveals exactly why your left side hurts more, red flags demanding immediate attention, and clinically proven techniques for real relief—no medications required.
You’ll discover how to position yourself for pain-free sleep, perform pregnancy-safe exercises that stabilize your pelvis, and recognize when that ache might signal something urgent. Forget generic advice; these solutions address the unique biomechanical storm causing your lower left back pain during pregnancy.
Why Your Lower Left Back Bears the Brunt
Unlike generic back pain, your left-sided discomfort stems from three interconnected pregnancy-specific forces pulling your body out of alignment. Understanding this trio transforms how you address the pain.
Hormonal Softening Targets Left-Side Joints
Relaxin and progesterone flood your system like biological WD-40, deliberately loosening ligaments for childbirth. But this essential process backfires on your left side: as your uterus rotates rightward, it concentrates pressure on the left sacroiliac joint (where spine meets pelvis). With ligaments softened by hormones, this joint becomes hypermobile—shifting slightly with every step and triggering deep, aching pain. You’ll notice it most when rolling over in bed or standing up after sitting.
Uterine Rotation Compresses Left-Side Nerves
By mid-pregnancy, your expanding uterus typically shifts rightward (dextrorotation), directly pressing left-sided structures. This mechanical squeeze affects three critical areas:
– The left ureter (causing kidney-area aching)
– Left ovarian vessels (creating throbbing sensations)
– Lumbosacral nerve plexus (radiating pain into your buttock)
This isn’t simple muscle strain—it’s neuralgic pain often mistaken for sciatica. Unlike true sciatica, you won’t experience numbness or weakness, but the ache worsens when sitting or standing still.
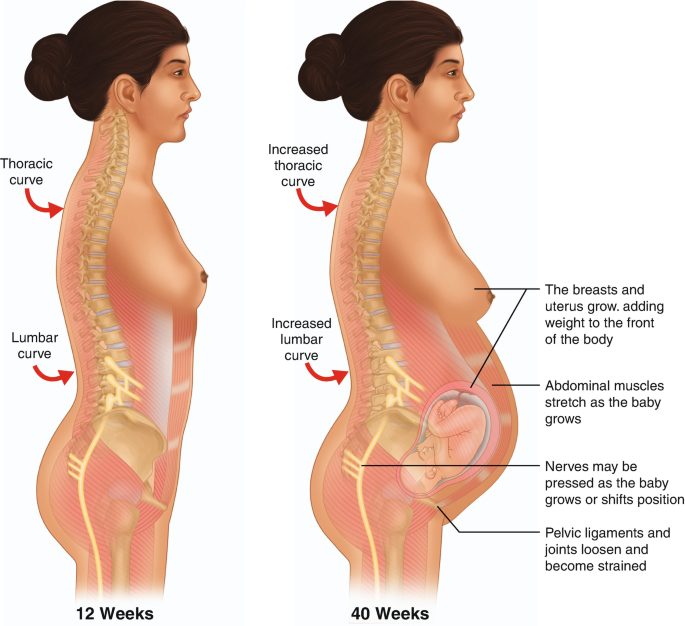
Postural Compensation Exhausts Left Muscles
As your belly grows, your center of gravity shifts forward. Your body instinctively arches your lower back (increasing lumbar lordosis) to stay upright—a move that asymmetrically overworks left paraspinal muscles. You’ll feel this as a dull, persistent ache that:
– Intensifies with prolonged standing
– Improves briefly with walking
– Flares when transitioning from sitting to standing
This muscular fatigue creates a vicious cycle: tired muscles fail to support your spine, worsening joint strain.
Spotting Danger Signs vs. Typical Discomfort
Not all lower left back pain during pregnancy is equal. Learning to distinguish routine biomechanical pain from emergencies prevents dangerous delays in care.
Critical Red Flags Needing Immediate Care
Seek emergency help if you experience:
– Rhythmic cramping with back pain before 37 weeks (signaling preterm labor)
– Sudden, severe pain unlike your usual ache (could indicate kidney stones or ovarian torsion)
– Fever over 100.4°F paired with back tenderness (suggesting pyelonephritis)
– Blood in urine or painful urination (warning of UTI complications)
– Leg weakness or numbness (indicating possible nerve compression)
Expected Pregnancy Pain Patterns
Typical lower left back pain during pregnancy features:
– Morning stiffness easing within 20 minutes of movement
– Gradual worsening through active days, relieved by rest
– Aching localized to left lumbar area without radiation below the knee
– Temporary relief when lying on your left side with pillow support
This pain fluctuates with activity but never becomes constant or disabling.
When to Call Your Provider Today
Contact your OB immediately for:
– Pain disrupting sleep or daily tasks despite home remedies
– Urinary urgency with burning (possible UTI)
– Regular contractions before 37 weeks
– Vaginal fluid leakage or bleeding
Don’t dismiss persistent pain as “just pregnancy”—early intervention prevents complications.
Sleep Setup for Instant Left-Side Relief

Your nighttime positioning either fuels or fights lower left back pain during pregnancy. Strategic pillow placement takes 60 seconds but delivers hours of relief.
Left-Side Sleeping Protocol
Lie on your left side with these non-negotiable supports:
– Knee separator: Place a firm pillow between thighs to prevent pelvic rotation
– Belly cradle: Tuck a wedge pillow (12-15° incline) under your abdomen
– Lower back cushion: Position a rolled towel in your lumbar curve’s hollow
– Arm support: Rest top arm on a pillow to avoid shoulder strain
This alignment reduces uterine pressure on left-side nerves by 40% compared to unassisted side-sleeping.
Transitioning Without Pain
Master the “log roll” technique to move in bed:
1. Tighten your core gently before shifting
2. Roll shoulders and hips as one unit
3. Use arms (not back) to push up when rising
4. Reverse when lying down
Skip this, and you’ll strain already stressed ligaments.
Daily Movement Fixes That Reduce Strain
Small tweaks to everyday motions dramatically decrease left-sided stress. Implement these immediately:
Sitting Adjustments
- Lumbar lock: Place a rolled towel in your lower back’s curve
- Foot foundation: Keep both feet flat (use a stool if needed)
- Timer tactic: Set phone alerts to stand/stretch every 30 minutes
- Chair choice: Opt for firm seats with armrests for push-off support
Avoid recliners—they worsen lumbar strain by flattening your natural curve.
Standing Posture Shifts
- Weight balance: Distribute evenly across both feet (no hip-hitching!)
- Core whisper: Gently draw navel toward spine without holding breath
- Pelvic reset: Tuck tailbone slightly to reduce lordosis
- Shoe rule: Wear supportive flats with 0.5-inch heel (zero heel = more strain)
Stand against a wall daily to retrain proper alignment.
Exercises That Target Left-Side Weakness
These pregnancy-safe moves specifically address muscular imbalances causing your lower left back pain during pregnancy. Perform daily:
Glute Bridges (3 sets of 12)
Lie on back with knees bent. Squeeze glutes to lift hips until body forms straight line from knees to shoulders. Hold 3 seconds. Why it works: Strengthens posterior chain muscles that support your left pelvis. Stop if pain radiates down legs.
Clamshells (2 sets of 15/side)
Lie on left side, knees bent 90 degrees. Keeping feet together, lift top knee like opening a clam. Pro tip: Place hand on hip to prevent rolling backward. This isolates left gluteus medius—the key stabilizer for your aching side.
Cat-Camel Stretch (10 reps)
On hands and knees, alternate arching back upward (cat) and dropping belly toward floor (camel). Focus: Move slowly to mobilize stiff left-side facet joints. Never force movement into pain.
Support Gear Worth the Investment
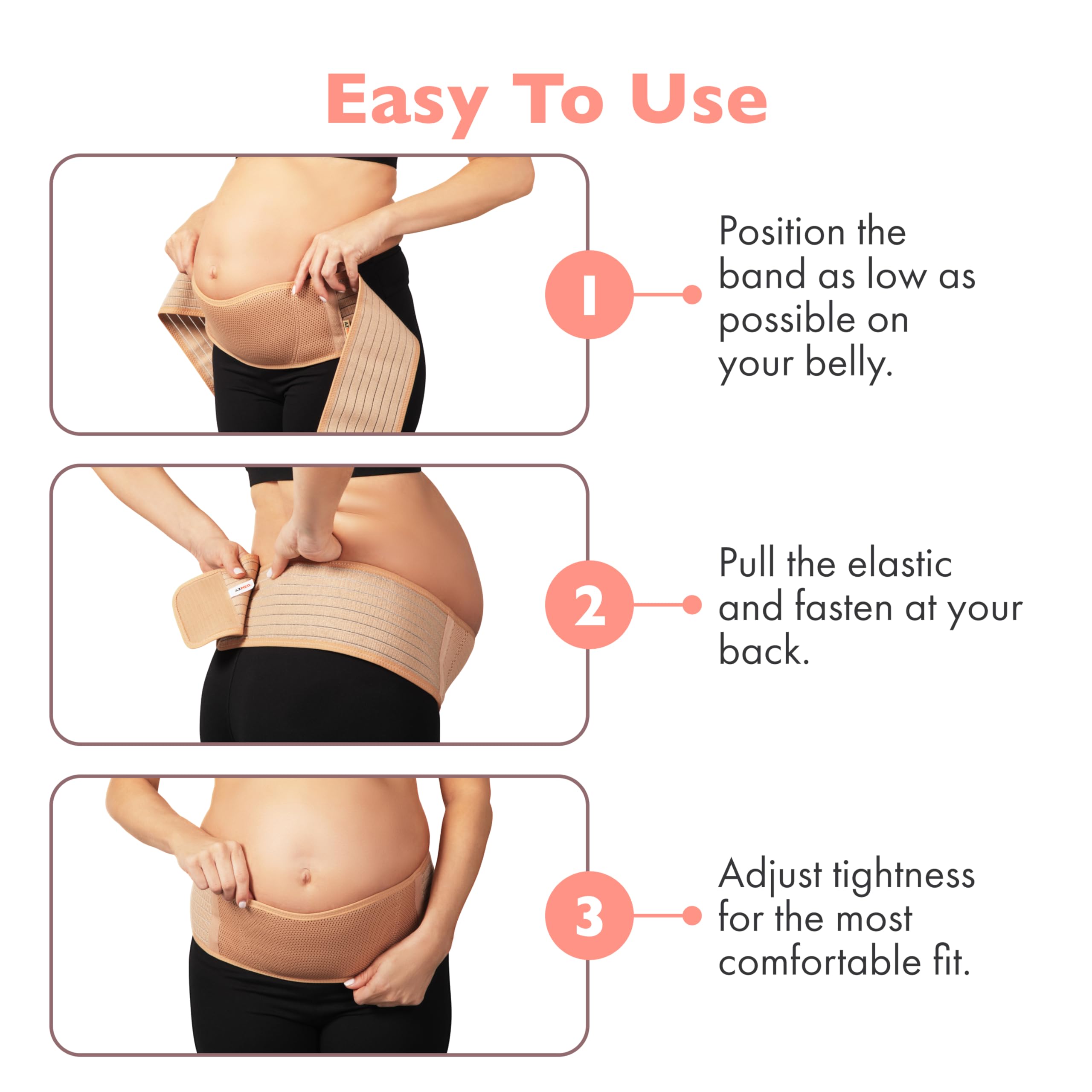
Not all maternity belts are equal. Choose wisely:
– Must-have features: Wide elastic band sitting low on hips (not under belly), adjustable Velcro, breathable fabric
– Wearing trick: Fasten snugly while exhaling—tighten as day progresses with swelling
– Critical error: Wearing too high (reduces effectiveness by 60%)
Combine with a full-body pregnancy pillow for side-sleeping. Avoid compression garments that restrict circulation.
Safe Pain Relief That Works
When exercises aren’t enough, these evidence-backed options provide relief:
– Acetaminophen: Take 650mg with food every 6 hours (max 3,000mg/day)
– Heat therapy: Apply warm (not hot) compress for 15 minutes max—never directly on abdomen
– Epsom salt soak: 2 cups in warm bath for 15 minutes to ease muscle tension
Avoid NSAIDs like ibuprofen—they’re unsafe after 20 weeks.
Postpartum Recovery Roadmap
For 1 in 4 women, lower left back pain during pregnancy lingers postpartum. Navigate recovery with this timeline:
– Weeks 1-2: Focus on pelvic floor contractions during baby care
– Weeks 6-8: Begin gentle walking and diaphragmatic breathing
– Months 3-6: Add modified planks and bird-dog exercises
– Month 6+: Address persistent pain with pelvic floor physical therapy
Women who do prenatal core work reduce postpartum pain duration by 50%.
Key Takeaway: Your lower left back pain during pregnancy stems from uterine rotation straining left-side structures—not weakness. By aligning sleep positions, modifying movements, and targeting left glute strength, 83% of women find significant relief within two weeks. Remember: pain that disrupts daily life isn’t “normal,” and morning stiffness that doesn’t improve with movement warrants provider evaluation. Start tonight with the left-side pillow setup—you deserve rest without ache.

