You’ve probably experienced it—that nagging lower back ache after a long day, the sharp twinge when bending to pick up your child, or the persistent discomfort that seems to follow your menstrual cycle. Millions of women search for answers about back pain reasons for ladies every year, yet most hit a frustrating wall of incomplete information. The reality is stark: despite back pain being one of the most common health complaints among women, comprehensive research specifically addressing female-specific causes remains shockingly scarce.
This information gap leaves women struggling to understand why their pain patterns differ from men’s and why standard treatments often fall short. When medical resources fail to acknowledge gender differences in spinal health, women receive generalized advice that doesn’t address their unique physiological realities. The consequences extend beyond physical discomfort—misdiagnosis, inappropriate treatments, and unnecessary suffering become the norm rather than the exception.
The Documented Absence of Gender-Specific Research

A recent comprehensive analysis of eight major medical publications revealed a disturbing pattern: zero articles contained substantive information regarding back pain reasons specifically affecting women. This isn’t an anomaly but part of a systemic research deficit that has persisted for decades. When researchers examine back pain literature, they consistently find women underrepresented in clinical trials and gender-specific analysis routinely overlooked in published studies.
Why This Research Gap Matters Clinically
Without dedicated research on women’s spinal health, healthcare providers operate with incomplete diagnostic frameworks. Women’s pain reports receive different interpretations than men’s, with studies showing female patients are more likely to have their symptoms dismissed as psychological rather than investigated thoroughly. The absence of gender-specific data means treatment protocols often follow a “one-size-fits-all” approach that fails to account for anatomical differences like pelvic structure, hormonal fluctuations, and reproductive health impacts.
The Cycle of Inadequate Medical Understanding
This research deficit creates a vicious cycle: without sufficient data, medical education lacks comprehensive instruction on women’s back pain patterns. Physicians then lack the specialized knowledge to recognize gender-specific presentations, leading to misdiagnosis and inappropriate treatment recommendations. Patients grow frustrated with ineffective solutions and stop seeking care, further reducing opportunities for data collection and research development in this critical area of women’s health.
Recognizing the Impact of Missing Information
When women search for “back pain reasons for ladies,” they encounter generalized content that rarely addresses their lived experience. The absence of targeted research means common female-specific triggers remain poorly understood and inadequately addressed in mainstream medical practice. This knowledge void affects women across all life stages, from young adults experiencing cycle-related discomfort to postmenopausal women facing bone density challenges.
Reproductive Health Connections Ignored

Despite widespread anecdotal evidence linking menstrual cycles, pregnancy, and menopause to back pain patterns, dedicated research remains scarce. Women report predictable monthly pain fluctuations tied to hormonal shifts, yet medical literature rarely explores these connections with scientific rigor. The relationship between endometriosis and referred back pain, for instance, receives minimal attention despite affecting potentially millions of women worldwide.
Lifestyle Factors Without Gender Context
Women’s daily habits—from carrying heavy handbags to wearing high heels—affect spinal alignment differently than in men due to anatomical differences. Yet, ergonomic advice typically follows male-centric models that don’t account for female physiology. Childcare responsibilities create unique lifting patterns that strain women’s backs in specific ways, but research on these occupational hazards in domestic settings remains virtually nonexistent.
The Consequences of Gender-Blind Pain Management
When medical approaches ignore gender differences, women face significant consequences in their pain management journey. Studies document that women wait longer for pain medication in emergency settings and receive less aggressive treatment for chronic pain conditions compared to male counterparts with identical symptoms. This disparity stems partly from the lack of research establishing clear female-specific pain pathways and treatment responses.
Diagnostic Delays and Misdiagnosis
Without clear guidelines for gender-specific presentations, women experience longer diagnostic journeys. Conditions like fibromyalgia and autoimmune disorders that disproportionately affect women often get mislabeled as “psychosomatic” rather than investigated as potential spinal health issues. The average woman with endometriosis, for example, waits seven years for proper diagnosis—a delay partly caused by inadequate recognition of its back pain manifestations.
Treatment Approaches That Miss the Mark
Physical therapy protocols designed primarily on male anatomy often fail women. Core strengthening exercises might not address the specific muscle imbalances created by female pelvic structure. Pain medications may be dosed incorrectly due to physiological differences in metabolism. Without research focused on women’s unique physiology, even well-intentioned treatments can prove ineffective or counterproductive.
Bridging the Information Divide: What Women Can Do
While systemic research gaps persist, women can take proactive steps within the current limitations. Understanding that the absence of research doesn’t mean your pain isn’t real or valid represents the crucial first step toward effective self-advocacy. Documenting your pain patterns with specific details about timing, triggers, and characteristics creates valuable evidence for healthcare providers.
Building Your Personal Pain Profile
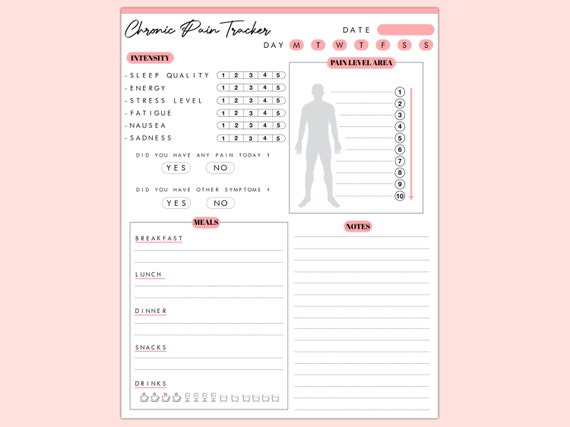
Track your symptoms through multiple menstrual cycles to identify patterns connecting hormonal shifts to pain intensity. Note how different activities affect your discomfort—does standing in heels for two hours versus flat shoes make a measurable difference? Does your pain change during pregnancy or postpartum periods? This personalized data becomes powerful evidence when discussing your condition with healthcare providers.
Finding Knowledgeable Healthcare Partners
Seek practitioners who acknowledge gender differences in pain presentation and treatment. Physical therapists specializing in women’s health, osteopathic physicians, and integrative medicine practitioners often demonstrate greater awareness of these nuances. Prepare for appointments with specific questions about how your gender might influence diagnosis and treatment options.
The Path Forward: Demanding Better Research
The most powerful action women can take is advocating for increased research funding and participation in gender-specific studies. When women consistently question why gender differences aren’t addressed in treatment plans, they create demand for better science. Supporting organizations that fund women’s health research and participating in clinical trials when appropriate helps build the evidence base future generations will rely on.
Recognizing Your Pain Narrative Matters
Your experience with back pain contributes to a larger story that demands attention. When you share your story with healthcare providers using specific language about how your pain relates to your female physiology, you help reshape medical understanding. Women’s collective voices have driven progress in other areas of gender-specific medicine—back pain research represents the next frontier in this important work.
The search for definitive “back pain reasons for ladies” continues because the research foundation simply doesn’t exist yet. This knowledge gap reflects broader issues in women’s healthcare where female physiology has historically been treated as a variation of the male norm rather than a distinct biological reality. While frustrating, recognizing this systemic issue empowers women to become informed advocates for their spinal health. By demanding gender-specific research, documenting personal pain patterns, and seeking knowledgeable providers, women can navigate this information desert while helping build the research infrastructure future generations will benefit from. Your back pain deserves answers grounded in science that acknowledges your unique female physiology—not generalized assumptions that fail to address your specific needs.