That sharp twinge in your lower back after just minutes of standing at the kitchen counter or checkout line isn’t normal—and it’s incredibly common. Four out of five adults will experience lower back pain during their lifetime, with standing often intensifying discomfort. If your job requires prolonged upright posture or household chores leave you wincing, you’re part of a global statistic: 619 million people currently battle this issue. This guide reveals exactly why standing triggers pain, how to pinpoint your specific cause, and science-backed strategies to find relief within days—without expensive treatments or surgery.
Why Standing Triggers Back Pain
Gravity relentlessly compresses lumbar discs and fatigues paraspinal muscles within two hours of static standing. This mechanical stress causes muscles to tighten and spasm, creating that familiar ache. Without movement to pump nutrients into spinal discs, temporary pain develops in 50% of healthy adults after just 120 minutes upright.
Core Weakness & Postural Drift
Weak abdominal and multifidus muscles fail to stabilize vertebrae, allowing spinal segments to drift out of alignment. Tight hamstrings or hip flexors tilt your pelvis forward, exaggerating lumbar curvature and multiplying disc pressure. This combination creates a perfect storm for standing-induced pain—especially if you’ve skipped core conditioning.
Workplace & Lifestyle Traps
Hard flooring without antifatigue mats transmits shock directly through your spine. High heels or collapsed arches in worn shoes alter your center of gravity, forcing compensatory spinal curves. Forward head posture while checking your phone strains cervical muscles, triggering chain reactions down your back. Most critically, skipping micro-breaks longer than 30 minutes starves fatigued muscles of recovery time.
Identify Your Pain Type Fast
| Pain Feel | Likely Cause | Key Clue |
|---|---|---|
| Dull ache on both sides | Muscle strain | Eases when sitting |
| Sharp shooting down leg | Disc herniation or stenosis | Worse with spinal extension |
| Sudden after minor twist | Facet joint irritation | One-sided, localized spot |
| Deep, non-mechanical | Referred organ pain | Unchanged by movement |
Red flags demand immediate care: saddle numbness, bladder/bowel changes, unexplained fever, or leg weakness. These indicate potential cauda equina syndrome or serious systemic illness requiring ER attention.
Quick Visual Inspection Steps
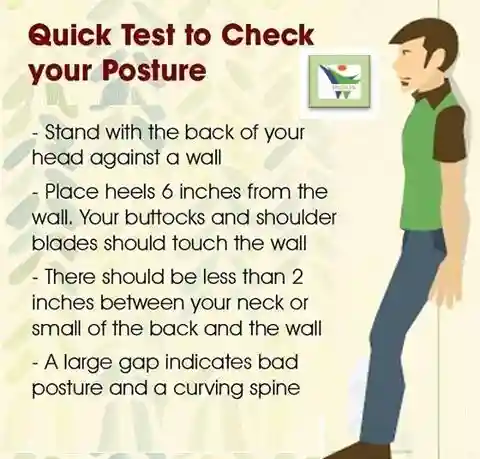
- Posture Check: Stand against a wall—ears, shoulders, hips, and ankles should align vertically
- Pelvic Tilt Test: Flatten your lower back against the wall; inability indicates tight hip flexors
- Single-Leg Stand: Hip drop or wobble reveals glute weakness
- Shoe Scan: Uneven wear patterns or collapsed arches compromise spinal alignment
Immediate Pain Relief Techniques
30-Second Micro-Break Routine
Shift weight side-to-side 10 times while pumping your calves. Step into a mini-backward lunge on each leg. Squeeze shoulder blades together for 5 seconds. Repeat hourly—these micro-movements instantly reduce disc compression.
Ice vs Heat Rules
Apply ice packs for 15 minutes every 2-3 hours during the first 48 hours of acute pain to reduce inflammation. After 48 hours, switch to heat pads for 20 minutes twice daily to relax spasmed muscles. Never sleep with either—risk of burns or frostbite increases dramatically.
OTC Meds That Work
Take ibuprofen 200-400 mg every 6-8 hours (max 3 days) for inflammation. Apply topical diclofenac gel 1% twice daily for localized relief. Use acetaminophen 500-650 mg if NSAIDs upset your stomach. Pro tip: Combine 200 mg ibuprofen + 325 mg acetaminophen for synergistic pain control—safe for short-term use.
Stretching Protocol for Standing Jobs
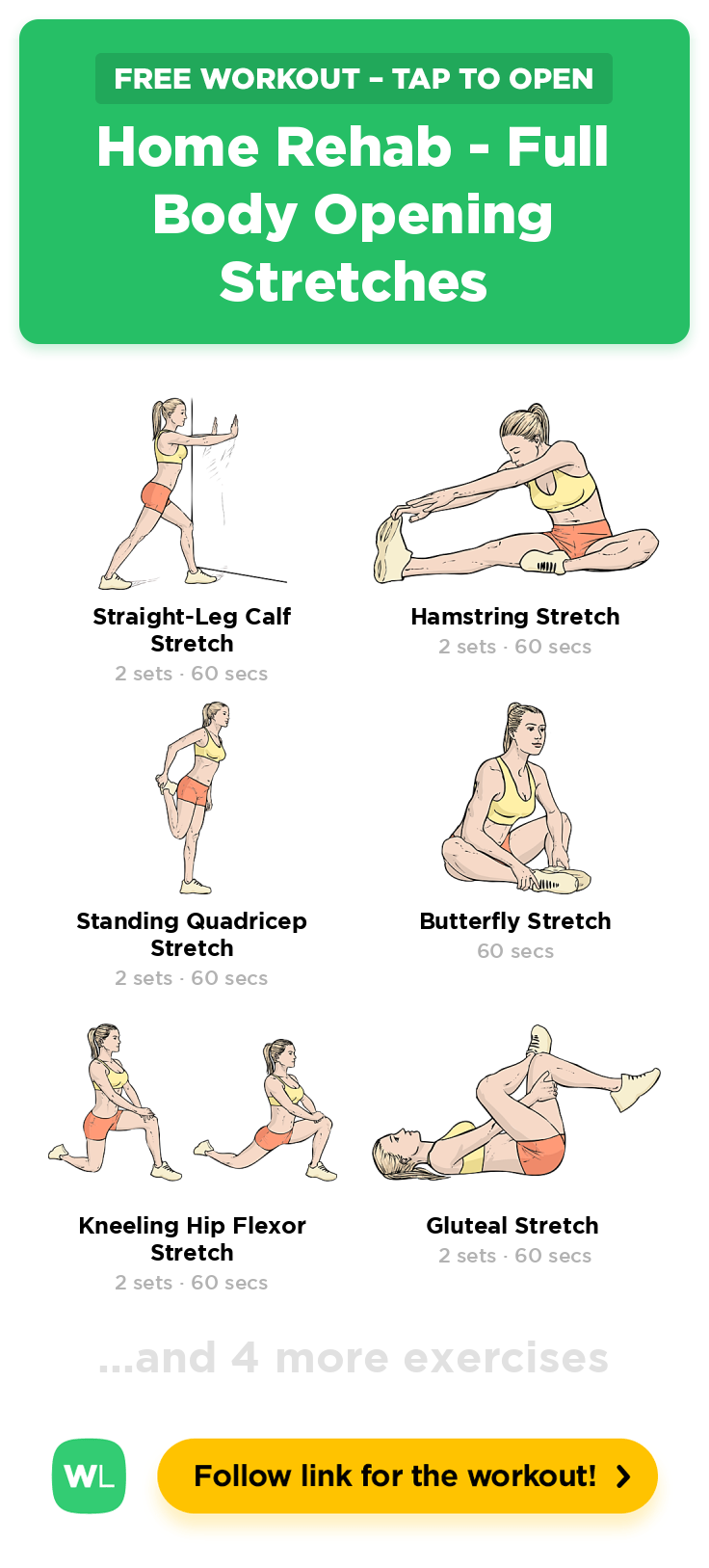
Hold each stretch 30 seconds, twice daily. For the hamstring stretch, sit on a chair edge, straighten one leg, and hinge forward from hips until you feel gentle tension behind your thigh. The hip-flexor release requires a half-kneeling lunge while tucking your pelvis under until you feel a stretch in the front of your hip. Try the standing child pose by placing hands on a chair seat and folding forward to relax your lower back. Finish with knees-to-chest: lie supine and gently hug both knees toward your chest.
Strengthen Your Core in 10 Minutes
| Exercise | Sets × Reps | Target |
|---|---|---|
| Pelvic Tilts | 2×15 | Deep abdominals |
| Bridges | 2×12 | Glutes & low back |
| Bird-Dog | 2×8 each side | Multifidus stability |
| Side Plank | 2×30 sec | Lateral core |
Start with pelvic tilts while seated at your desk—gently rock your pelvis forward and backward to activate deep core muscles. Progress to bridges (supine hip lifts) and bird-dog (opposite arm-leg extensions) once pain decreases. Hold side planks against a wall if full floor version strains your back.
Fix Your Standing Workstation

Footwear Upgrade
Choose shoes with cushioned soles, proper arch support, and heel height under 2 cm. Replace footwear every 500 miles or 6 months—collapsed midsoles transfer impact directly to your spine. Avoid high heels that tilt your pelvis forward.
Mat & Surface Fixes
Use a 3/4-inch thick antifatigue mat to absorb vibration. Install an 8-inch footrest to alternate leg stance, reducing static load. If possible, add a sit-stand desk and change positions every 30-45 minutes—movement is medicine for standing back pain.
Posture Reset Drill
Hourly, roll shoulders back, engage your abs gently (as if zipping tight jeans), unlock knees slightly, and tuck your chin. This “posture reset” combats the spinal compression that builds during prolonged standing.
When to See a Doctor
Schedule Within 1 Week
Book an appointment if pain persists beyond 7 days despite home care, or if you experience leg numbness/tingling. Nighttime pain that wakes you also warrants professional evaluation within a week.
Emergency Red Flags
Seek immediate care for loss of bladder/bowel control, foot drop (inability to lift toes), fever with back pain after travel, or new pain with cancer history. These indicate potentially serious conditions requiring urgent imaging.
Medical Treatments Beyond Pills
Physical therapy (2-3 sessions/week for 4-6 weeks) combines manual therapy with progressive loading exercises. Trigger-point injections relieve muscle knots, while epidural steroids target disc-related leg pain. Facet joint blocks under fluoroscopy help arthritic joints. For chronic cases unresponsive to conservative care, ReActiv8 neurostimulation shows 67% pain resolution in trials by reactivating dormant multifidus muscles.
Long-Term Prevention Plan
Commit to core/hip strengthening 3× weekly and 20-minute brisk walks on alternate days. Schedule annual ergonomic assessments—especially if you work standing jobs. Replace supportive shoes every spring and quit smoking immediately (it doubles disc degeneration risk). Maintain BMI under 25; each lost pound reduces spinal load by 4 pounds. Take vitamin D 800-1000 IU daily to support bone health.
Quick Reference Cheat Sheet
Morning: 5-minute stretch flow before coffee
Workday: Micro-break every 30 minutes, antifatigue mat under feet
Evening: Heat therapy + core routine, no phone in bed
Weekly: Check shoe wear patterns, posture mirror test
Most standing-related back pain resolves within 2-4 weeks with consistent movement and load management. Start implementing these strategies today—your spine will thank you tomorrow. Remember: 97% of cases are mechanical and self-limiting with proper care. Don’t wait for pain to dictate your life when simple solutions exist right now.