You’re waiting in line at the pharmacy when a familiar ache begins in your lower back. But the moment you start walking to your car, the pain vanishes completely. If this scenario sounds familiar, you’re experiencing a specific type of back pain that plagues millions—discomfort that appears exclusively during standing but disappears with movement. This frustrating phenomenon affects approximately 80% of adults at some point in their lives, yet few understand why standing triggers pain while walking provides relief. The key lies in how your spine handles static versus dynamic loads, and with the right approach, you can eliminate this standing-specific pain for good.
Unlike walking, which naturally shifts weight and engages different muscle groups, standing locks your spine into one position. During static standing, your spine bears significantly more pressure as discs compress and muscles tighten without the natural pumping action movement provides. Blood flow decreases to critical areas, inflammation builds, and before you know it, that familiar ache sets in. The good news? By understanding the precise mechanisms behind standing-induced back pain and implementing targeted solutions, you can stand comfortably for as long as needed without pain.
Why Standing Creates Back Pain But Walking Doesn’t
Standing triggers back pain through a unique compression cascade that walking naturally prevents. When you stand still, your spine experiences increased static load as discs compress within minutes. This continuous pressure forces your lower back muscles into sustained contraction without relief, rapidly decreasing blood flow and triggering inflammation. The resulting muscle fatigue sends pain signals that walking immediately resolves by shifting weight distribution and restoring circulation.
Critical differences between standing and walking:
– Spinal loading: Standing creates 40% more continuous pressure on spinal structures than walking
– Muscle engagement: Walking naturally alternates muscle groups while standing locks muscles in one position
– Blood flow: Movement during walking pumps oxygenated blood to fatigued tissues
– Disc hydration: Walking creates natural pumping action that hydrates spinal discs
Unlike walking’s dynamic motion, standing forces your body into a single posture without micro-movements. This explains why even brief walking breaks provide instant relief—movement restores the natural biomechanics your spine needs to function pain-free.
Common Causes Behind Standing-Specific Pain

Postural Stress Patterns
Poor standing posture creates the foundation for standing-induced pain. Slouching or leaning forward increases spinal compression while inadequate core engagement forces your lower back muscles to work overtime. Look for these postural red flags:
– Shoulders rounded forward while standing
– Weight shifted primarily to one leg
– Knees locked straight
– Arch collapsed in feet
Quick posture check: Stand against a wall with your head, shoulders, and buttocks touching it. There should be just enough space for your palm behind your lower back. If you can fit a fist, your posture needs correction.
Muscle Imbalance Syndrome
Weak core and glute muscles force your lower back to compensate during standing. The transverse abdominis—your deepest abdominal muscle—should activate automatically to support your spine. When it doesn’t, your erector spinae muscles take over, leading to rapid fatigue and pain.
Simple muscle test: Can you maintain a slight abdominal brace while standing for 30 seconds without lower back muscles burning? If not, muscle imbalance is likely causing your pain.
Structural Conditions
Several medical conditions specifically worsen during standing:
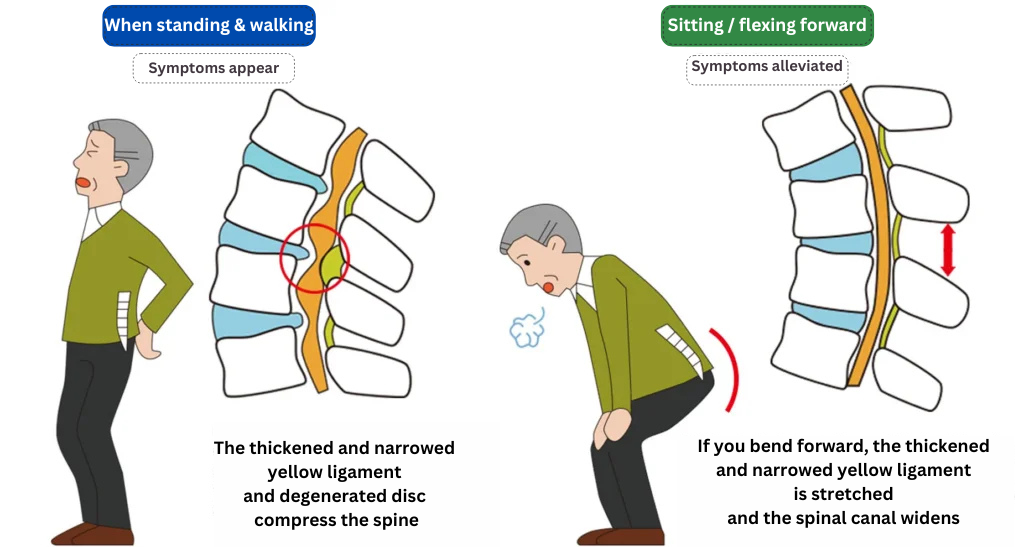
Spinal stenosis narrows spinal spaces, creating nerve compression that intensifies when upright. Herniated discs may bulge more under standing pressure, causing radiating pain. Spondylolisthesis—a slippage of vertebrae—becomes more pronounced when standing still, triggering localized pain.
Immediate Pain Relief Strategies
30-Second Standing Relief Sequence
When pain strikes while standing, implement this micro-movement routine:
- Shift weight to your left leg for 10 seconds
- Transfer weight to right leg for 10 seconds
- Gently rock forward onto balls of feet, then back onto heels
- Take 3-5 steps in place, lifting knees slightly
This sequence disrupts the muscle tension cycle and restores circulation, providing relief within seconds.
Temperature Therapy Protocol
For acute pain (first 48 hours): Wrap a cold pack in thin cloth and apply to your lower back for 20 minutes. Cold reduces inflammation and numbs pain signals.
For chronic pain: Use a heating pad on medium setting for 20 minutes. Heat relaxes muscle spasms and improves blood flow, accelerating healing.
Emergency Stretch Sequence
Keep these three standing stretches in your pain-relief toolkit:
Standing Child’s Pose: Place hands on wall at shoulder height, walk hips back while keeping arms straight. Hold for 20-30 seconds.
Pelvic Tilt: While standing, gently tuck your tailbone under, then release. Repeat 10 times slowly.
Hip Flexor Stretch: Step one foot back, bend front knee, and gently press hips forward. Hold 20-30 seconds per side.
Prevent Standing Pain Long-term
Posture Correction System
Transform your standing posture with these daily practices:
Morning alignment check: Stand against a wall with head, shoulders, and buttocks touching. Practice maintaining this posture throughout the day, ensuring weight distributes evenly across both feet.
Core activation drill: Throughout the day, practice gently drawing your navel toward your spine (without holding your breath). This engages deep core muscles automatically during standing.
Workstation Optimization
Create an environment that supports your spine:
Anti-fatigue mats reduce pressure by 50% compared to hard floors. Place one wherever you stand for extended periods—kitchen, workspace, or workshop.
Footwear upgrade: Replace shoes every 300-500 miles of wear. Look for shoes with firm midsoles and adequate arch support. Avoid completely flat shoes or high heels.
Progressive Strengthening Program
Week 1-2: Master the basics
– Wall sits: 3 sets of 30 seconds
– Bird dog: 3 sets of 10 per side
– Glute bridges: 3 sets of 15
Week 3-4: Increase challenge
– Single-leg bridges: 3 sets of 12 per leg
– Side planks: 3 sets of 20 seconds per side
– Dead bugs: 3 sets of 10 per side
Week 5+: Maintain and progress
– Add resistance bands
– Increase hold times
– Incorporate functional movements
Medical Treatment Options

When to Seek Professional Help
Immediate consultation required if you experience:
– Numbness or tingling down both legs
– Loss of bladder or bowel control
– Severe pain following a fall or accident
– Fever with back pain
Schedule within 48 hours for:
– Pain persisting beyond one week
– Radiating pain past your knee
– Progressive weakness in legs
Professional Treatment Pathways
Physical therapy offers the highest success rates for standing-induced back pain. A skilled therapist will assess your movement patterns, identify specific muscle imbalances, and create a customized strengthening program. Most patients see improvement within 6-8 visits.
Medication management may include short-term NSAIDs like ibuprofen for inflammation, or muscle relaxants for severe spasms. These work best alongside movement-based treatments rather than as standalone solutions.
Daily Prevention Habits
Micro-break Strategy
Set phone alarms every 20-30 minutes during prolonged standing. Use these breaks for:
– 30 seconds of gentle stretching
– Brief walk to change posture
– Core activation exercises
Evening Recovery Routine
End each day with 5 minutes of spinal decompression:
– Lie on your back with knees bent
– Gently draw knees to chest, hold 30 seconds
– Perform 10 gentle pelvic tilts
– Finish with 2 minutes of diaphragmatic breathing
Weekly Progress Tracking
Monitor your standing tolerance weekly:
– Week 1: Track pain onset time (when pain starts)
– Week 2: Note pain intensity (1-10 scale)
– Week 3: Measure standing duration before discomfort
– Week 4: Assess overall daily pain frequency
Success indicators: Increasing standing time, decreasing pain intensity, and longer intervals between pain episodes signal effective treatment.
Key takeaway: Back pain while standing but not walking typically stems from postural stress and muscle imbalances rather than serious structural damage. With targeted strengthening, posture correction, and lifestyle modifications, most people achieve significant improvement within 4-8 weeks. The key lies not in avoiding standing, but in preparing your body to handle it efficiently through proper muscle activation and movement patterns. By implementing these specific strategies, you can stand comfortably for as long as needed without pain returning the moment you stop moving.

