That persistent ache in your lower back that refuses to fade might be more than just a muscle strain. While 80% of adults experience back pain in their lifetime, cancer-related lower back pain follows a distinct pattern that demands attention. Unlike ordinary back issues, cancer pain often intensifies at night, persists despite rest, and signals potential spinal metastasis—affecting 30-70% of cancer patients. Recognizing these subtle differences could mean the difference between timely intervention and permanent damage.
Most back pain resolves within weeks, but cancer pain behaves differently. It typically worsens progressively over 4-6 weeks without improvement from standard treatments like ice, heat, or over-the-counter medications. If your lower back pain feels unlike any you’ve experienced before—especially with unexplained weight loss or night sweats—you need immediate evaluation. This guide reveals the specific warning signs, diagnostic pathways, and treatment options for cancer-related lower back pain.
Nighttime Lower Back Pain That Worsens When Lying Down
Cancer-related lower back pain often intensifies dramatically at night, disrupting sleep despite comfortable positioning. This happens because tumors release inflammatory molecules that accumulate when you’re inactive. Unlike mechanical pain that improves with rest, cancer pain becomes more pronounced when lying down—many patients report needing to walk around to find relief.
If you’re waking up between 2-4 AM with deep, unrelenting lower back pain that doesn’t respond to position changes, this warrants immediate medical attention. Track your pain pattern for three nights—cancer pain typically follows a consistent nighttime worsening pattern rather than occasional discomfort.
Progressive Lower Back Pain Despite Conservative Treatment
Cancer pain shows no improvement with standard back pain remedies. If your lower back pain continues escalating over 4-6 weeks despite:
– Regular stretching exercises
– Over-the-counter pain medications
– Heat or cold therapy
– Activity modification
This progressive worsening signals potential malignancy. Document your pain levels daily using a 0-10 scale—cancer pain typically increases by at least 2 points weekly without intervention. Pay special attention if pain begins interfering with basic activities like putting on shoes or standing from a seated position.
Systemic Symptoms Accompanying Lower Back Cancer Pain
Cancer-related lower back pain rarely appears in isolation. Watch for these critical accompanying signs:
- Unexplained weight loss exceeding 10 pounds in 6 months without dieting
- Persistent low-grade fever above 100.4°F without infection
- Severe fatigue that doesn’t improve with rest
- Drenching night sweats requiring clothing changes
- New bowel or bladder changes like incontinence
These systemic symptoms combined with persistent lower back pain create a red flag pattern that demands immediate imaging. Don’t dismiss these as “just stress” or “aging”—they often indicate cancer spread requiring urgent treatment.
Movement-Independent Lower Back Pain Patterns
Unlike muscle strains that flare with specific movements then improve, cancer pain maintains steady intensity regardless of position. If your lower back pain:
– Persists while sitting, standing, and lying down
– Doesn’t change with stretching or position changes
– Feels deep and constant rather than sharp and localized
This movement-independent pattern suggests bone involvement rather than soft tissue injury. Cancer pain often feels like a “toothache in the spine”—deep, throbbing, and unrelieved by typical remedies. Pay attention if pain remains consistent whether you’re active or resting.
Lung Cancer’s Silent Lower Back Invasion
Lung cancer affects 25% of patients with lower back pain as their initial symptom. The pain typically presents as a deep, constant ache between shoulder blades that gradually spreads downward. Many patients dismiss this as poor posture or sleeping wrong, delaying diagnosis by months.
If you’re a current or former smoker experiencing persistent lower back pain with:
– Shortness of breath during mild activity
– Chronic cough that worsens at night
– Coughing up blood-tinged sputum
Request immediate imaging. Smokers have 5.2-13 times higher lung cancer risk, and new back pain in this population requires urgent evaluation.
Prostate and Breast Cancer Spinal Spread Patterns
Men with prostate cancer often experience deep, boring lower back pain that may radiate to hips—a sign the cancer has spread to bone. This pain frequently mimics arthritis, leading to inappropriate treatment with physical therapy alone.
Women with breast cancer may notice subtle, intermittent lower back aches that become constant over weeks. Pay special attention if pain worsens during your menstrual cycle, which can mask symptoms as “hormonal.”
Both cancers commonly metastasize to the spine, yet only 1% of breast cancer patients present with back pain as their first symptom. Any persistent lower back pain in cancer survivors warrants immediate investigation.
Kidney Cancer’s Characteristic Lower Back Ache
Kidney cancer produces a constant dull ache in the lower back, typically on one side. Unlike kidney stones that cause sharp, intermittent pain, cancer-related pain remains steady and gradually intensifies. Patients often report:
- Flank tenderness when pressure is applied
- Blood in urine (visible or microscopic)
- Persistent one-sided lower back discomfort
This pain pattern frequently gets misdiagnosed as muscle strain. If lower back pain persists beyond 6 weeks with any urinary changes, demand further testing.
Diagnostic Imaging That Detects Spinal Metastases

Standard X-rays miss 30-50% of early metastatic lesions because cancer must destroy significant bone before appearing on imaging. If your doctor orders only X-rays for persistent lower back pain, request an MRI—the gold standard for detecting spinal tumors.
MRI reveals:
– Soft tissue masses compressing nerves
– Bone marrow changes before visible bone destruction
– Multiple tumor sites simultaneously
– Spinal cord compression requiring emergency treatment
Don’t accept “normal X-rays” as reassurance—many spinal metastases appear only on advanced imaging. Push for appropriate testing if your lower back pain follows cancer warning patterns.
Immediate Red Flags Requiring Emergency Care
:max_bytes(150000):strip_icc()/spinal-cord-compression-4706467_color-d7ad5f748ada48318e63c1f9e9ca074e.gif)
Call 911 or go to the ER immediately if you experience:
– Sudden leg weakness or paralysis
– Loss of bladder or bowel control
– Numbness spreading up from feet
– Severe lower back pain with fever over 101°F
– Inability to walk or stand
These symptoms indicate spinal cord compression—a medical emergency that can cause permanent paralysis within hours. Don’t wait for morning—seek immediate care if neurological symptoms accompany your lower back pain.
Pain Management Strategies That Target Cancer Pain
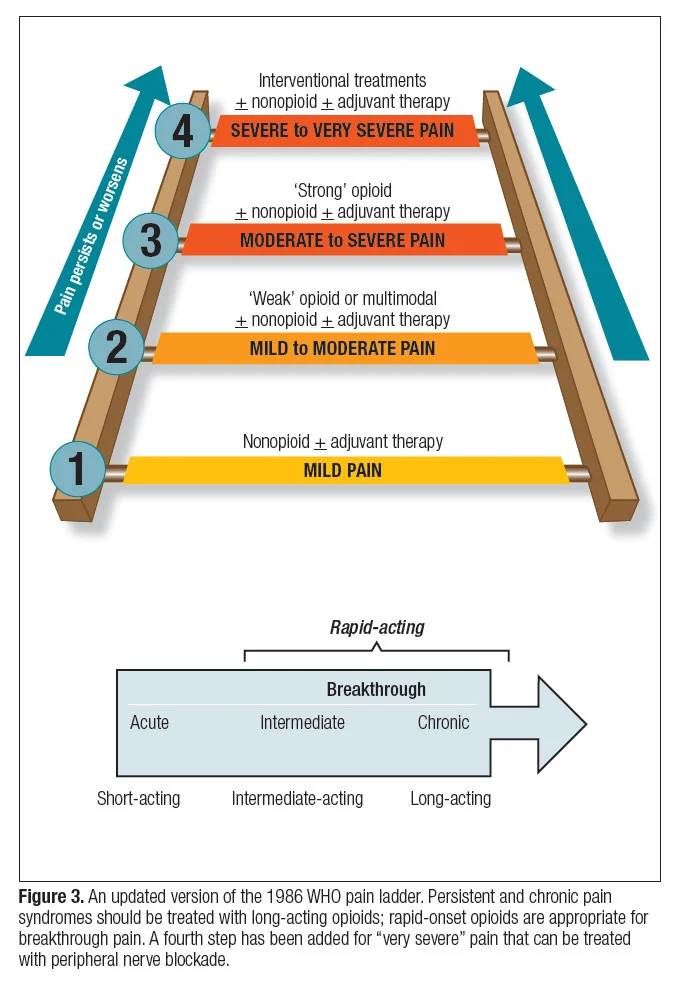
Cancer pain requires a specialized approach different from ordinary back pain. The medication ladder for cancer-related lower back pain includes:
- Non-opioid medications: NSAIDs like ibuprofen for mild pain
- Weak opioids: Tramadol for moderate pain
- Strong opioids: Morphine for severe pain
- Adjuvant medications: Antidepressants for nerve pain
Never self-medicate—cancer pain medications can dangerously interact with chemotherapy. Always coordinate with your oncology team, who will adjust doses based on your specific cancer and treatments.
At-Home Positioning Techniques for Lower Back Cancer Pain
Optimize your sleep position to minimize nighttime pain:
– Side-lying with pillow between knees reduces spinal stress
– Elevated head position decreases nighttime pain flares
– Firm mattress prevents spinal sagging during sleep
– Adjustable bed allows position changes without strain
For daytime relief:
– Frequent position changes every 20-30 minutes
– Ergonomic seating with lumbar support
– Shower chair eliminates standing fatigue
– Walking program maintaining bone density
These simple modifications significantly improve comfort when dealing with cancer-related lower back pain.
When to Demand Further Testing for Lower Back Pain
Don’t accept “just back pain” as an explanation if you experience:
– Pain lasting more than 6 weeks
– Progressive worsening despite treatment
– Pain unrelated to movement or position
– Pain with unexplained weight loss
– Pain with new neurological symptoms
Push for advanced imaging if you have:
– Personal or family cancer history
– Smoking history
– Previous cancer diagnosis
– Age over 50 with new persistent pain
Trust your instincts—if something feels different about your lower back pain, insist on thorough evaluation. Early detection of spinal metastases preserves neurological function and significantly improves treatment outcomes.
Final Warning Signs You Must Take Seriously
Cancer-related lower back pain follows distinct patterns that set it apart from ordinary back issues. While most back pain resolves within weeks, cancer pain persists, progresses, and often signals serious underlying disease. The key red flags—night pain, systemic symptoms, progressive worsening, and neurological changes—demand immediate attention.
Remember: persistent lower back pain lasting over 6 weeks with any warning signs requires urgent medical evaluation. Early detection of spinal metastases can prevent paralysis, maintain quality of life, and significantly impact treatment outcomes. Don’t dismiss new or changing back pain—your spine health directly affects your independence and mobility. If your lower back pain feels different from anything you’ve experienced before, seek care immediately. Your life may depend on it.

