That sharp stab when you bend for your coffee mug. The grinding ache that follows a day of gardening. The stiffness that makes mornings feel like a battle. If you’ve experienced these, you’re in overwhelming company—80% of adults face disabling lower back pain at some point. Yet most sufferers never pinpoint why their spine rebels. Understanding the true causes of lower back pain transforms guesswork into targeted action. This guide cuts through medical jargon to reveal the eight most frequent culprits, helping you identify your specific trigger and take control of relief.
Lower back pain isn’t a single condition but a symptom with diverse origins. Ignoring the root cause often leads to wasted time on ineffective treatments. Whether your discomfort flares suddenly after lifting a suitcase or creeps in from years of desk work, this breakdown empowers you to communicate precisely with healthcare providers. You’ll learn to distinguish between everyday muscle strains and serious red flags requiring immediate attention. Let’s uncover what’s really behind your back’s distress signals.
How Muscle and Ligament Injuries Trigger Pain
Sudden Lifts That Tear Your Back’s Support System
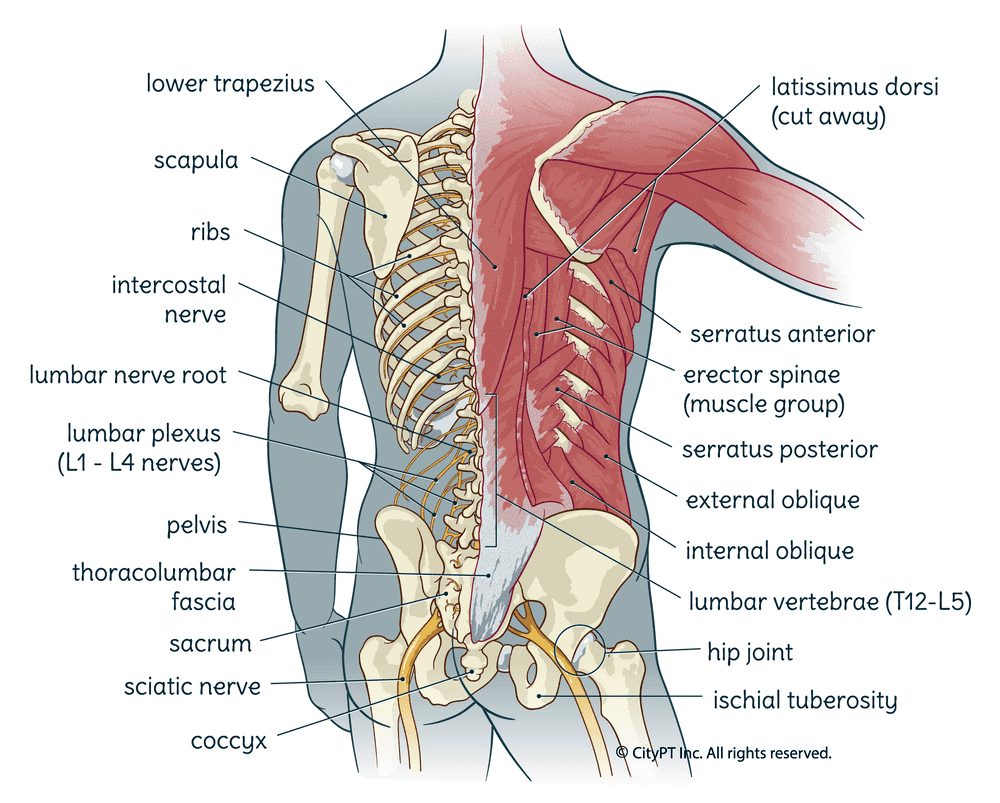
Twisting while hoisting heavy luggage or shoveling wet snow can instantly overstretch spinal ligaments and paraspinal muscles. These tissues tear at a microscopic level, triggering immediate inflammation and sharp localized pain. The damage typically announces itself within seconds—a warning that your back’s structural integrity has been compromised. Muscle spasms often follow as your body braces against further injury, creating a vicious cycle of pain and stiffness that worsens with movement.
Desk Jobs and Daily Habits That Wear Down Your Spine
Poor posture during marathon work sessions or repetitive bending during household chores creates insidious damage. Unlike acute injuries, this micro-trauma builds silently through cumulative stress on ligaments and muscles. You might dismiss early stiffness as “normal aging,” but it signals chronic inflammation from sustained strain. Office workers leaning forward at computers, truck drivers jostled by road vibration, or parents constantly bending to lift toddlers all accelerate this wear-and-tear process. The result? Progressive weakness that leaves your spine vulnerable to sudden breakdowns.
Critical warning signs needing medical evaluation:
– Muscle spasms persisting beyond two days despite rest
– Pain radiating below the knee into your calf or foot
– Inability to stand straight without severe discomfort
Disc Damage: The Silent Spine Saboteurs
Age-Related Disc Breakdown You Can’t Ignore
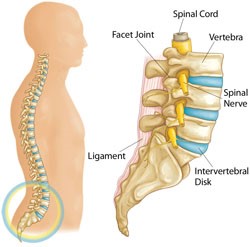
Your spinal discs act as shock absorbers, but they begin dehydrating around age 30. This natural degeneration reduces disc height and cushioning, causing vertebrae to rub closer together. While universal in aging, symptomatic degenerative disc disease creates deep aching pain centered in the lower back that may spread to your buttocks or thighs. Morning stiffness often lingers longer than 30 minutes, and pain intensifies when sitting for extended periods or twisting your torso. This isn’t “just aging”—it’s your spine signaling compromised stability.
Bulging vs. Herniated Discs: Know the Difference
A bulging disc occurs when weakened outer layers allow inner gel material to protrude outward without rupturing—like a tire sidewall swelling. This often causes central or bilateral back pain that worsens when bending forward. A herniated disc takes it further: a complete tear in the disc’s outer layer ejects nucleus material directly into your spinal canal. This compresses nerve roots, triggering classic sciatica—sharp, shooting pain down one leg accompanied by numbness or tingling in your foot. Heavy lifting with poor form or even a forceful sneeze can cause this rupture.
Herniation emergency indicators:
– Electric-shock pain traveling down your leg when sitting
– Foot drop (tripping due to weak ankle lift)
– Numbness in your inner thigh or groin area
Nerve Compression: When Back Pain Becomes Leg Pain
Sciatica’s Distinctive Burning Trail
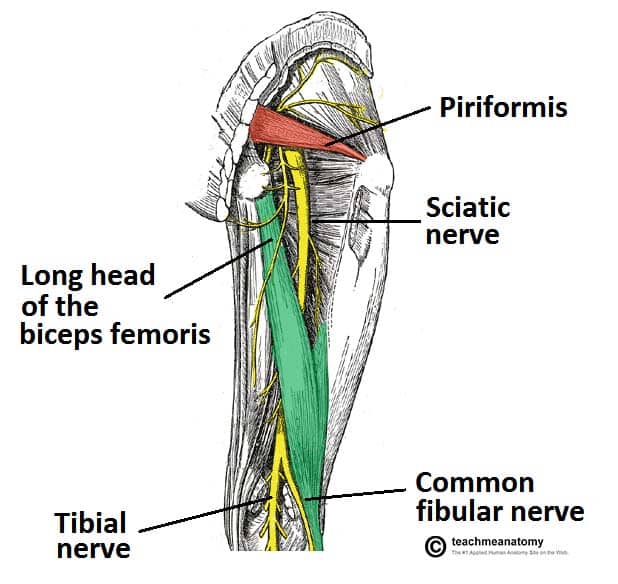
True sciatica isn’t back pain—it’s nerve pain radiating from your buttock down the back of your leg, often reaching your foot. This burning or shooting sensation intensifies when coughing, sneezing, or sitting upright for more than 20 minutes. Unlike muscle strain, sciatica follows a precise path corresponding to compressed nerve roots (L4-S1). You might feel it as tingling in your big toe or deep ache in your calf, but it always originates from irritated nerves—not your spine itself.
Top Compression Culprits Beyond Herniated Discs
While herniated discs cause most sciatica cases, other triggers include:
– Spinal stenosis: Narrowed nerve pathways from arthritic bone spurs
– Piriformis syndrome: A tight buttock muscle pinching the sciatic nerve
– Spondylolisthesis: Vertebra slippage compressing exiting nerves
– Foraminal narrowing: Age-related narrowing where nerves exit the spine
Structural Spine Failures You Must Recognize

Spinal Stenosis’ Walking Paradox
This condition creates a unique symptom pattern: bilateral leg pain, cramping, or heaviness that strikes only when walking upright. Unlike vascular claudication, stenosis pain vanishes when you sit or bend forward—like pushing a shopping cart. The narrowing of your spinal canal (from thickened ligaments or arthritic joints) compresses nerve roots during extension. If standing triggers symptoms within 5-10 minutes, but leaning on a grocery cart provides instant relief, stenosis is likely the cause of lower back pain.
Vertebral Slippage From Stress Fractures
Spondylolisthesis occurs when a vertebra slides forward over the one below, usually at L4-L5 or L5-S1. Isthmic types stem from stress fractures in the pars interarticularis (common in gymnasts or weightlifters), while degenerative types arise from facet joint arthritis. Beyond localized back pain, you’ll notice tight hamstrings limiting forward bends and possible radiating leg symptoms if the slippage compresses nerves. A telltale sign is pain worsening when arching your back during activities like vacuuming.
Inflammatory Arthritis: The Younger Patient’s Surprise
Osteoarthritis’ Morning Stiffness Clue
Facet joint osteoarthritis creates localized lower back aching that intensifies with backward bending or twisting. Morning stiffness lasting 30+ minutes distinguishes it from simple muscle strain. You might feel referred pain in your buttocks or thighs, but it rarely travels below the knee. This degeneration accelerates with obesity or occupations involving repetitive spinal loading. If pain improves after 20 minutes of movement but flares during prolonged standing, facet joint arthritis is a probable cause.
Ankylosing Spondylitis’ Night Pain Pattern
This inflammatory condition often starts before age 40 with insidious lower back pain that worsens at night and improves with exercise. Unlike mechanical pain, it intensifies with rest and may alternate between buttocks. Early signs include gradual loss of spinal flexibility—struggling to touch your toes or turn your head while reversing. If morning stiffness exceeds 60 minutes and responds poorly to standard painkillers, seek evaluation for inflammatory causes of lower back pain.
Organ-Related Pain Masquerading as Back Trouble
Kidney Stones vs. Infections: Location Tells All
Kidney stone pain originates in your flank (side of waist), radiating downward to the groin in colicky waves. Nausea and blood-tinged urine often accompany it. Pyelonephritis (kidney infection) creates a constant dull ache under your ribcage at the costovertebral angle, plus fever and burning urination. Both mimic back pain but lack positional triggers—your discomfort won’t change when bending or sitting.
Female-Specific Triggers Every Woman Should Know
Pregnancy causes lower back pain in 50-70% of women due to weight shift, ligament laxity, and uterine pressure. Ovarian cysts create cyclic pain worsening before periods, while endometriosis causes deep pelvic aching that radiates to the back during menstruation. Fibroids may produce constant pressure-like pain. If your back discomfort correlates with your menstrual cycle or pregnancy, gynecological evaluation is essential.
When Lifestyle Choices Become Pain Triggers
Four Modifiable Risk Factors You Control
Smoking starves spinal discs of oxygen, accelerating degeneration. Sedentary habits weaken core muscles that stabilize your spine—like removing suspension from a car. Obesity adds 4-6 pounds of extra load per pound gained, straining discs and joints. Chronic stress heightens pain sensitivity through muscle tension and nervous system changes. Fixing these won’t reverse existing damage but prevents progression of lower back pain.
Non-Changeable Risks Requiring Smart Management
Age over 30 increases disc degeneration risk; genetics influence susceptibility to arthritis. Women face higher rates during reproductive years due to hormonal shifts. While you can’t alter these, understanding them helps target prevention: prioritize core strengthening if you have family history, or manage weight aggressively with genetic risk.
Emergency Signs That Demand Immediate Action
Seven Red Flags You Must Never Ignore
Seek urgent care if back pain accompanies:
– Bowel or bladder incontinence (cauda equina syndrome)
– Progressive leg weakness or foot drop
– Unexplained fever with severe back pain
– History of cancer plus new persistent pain
– Night pain that worsens when lying flat
– Saddle anesthesia (numbness in inner thighs)
– Trauma from fall or accident with osteoporosis
Age-Based Warning Thresholds
First-time severe back pain under age 20 often indicates serious conditions like infection or tumor. Over age 50, new pain warrants prompt evaluation due to higher fracture and cancer risks. Don’t dismiss “just back pain” in these age groups—early intervention prevents permanent damage.
Key Takeaway: Your lower back pain likely stems from multiple overlapping causes—not just one simple issue. Muscle strains often combine with disc changes or lifestyle factors to create persistent discomfort. By identifying your specific pain pattern (does it radiate? worsen with sitting? follow your menstrual cycle?), you target treatments effectively. Start with modifiable risks: quit smoking, strengthen your core, and adjust workstation ergonomics. When symptoms persist beyond two weeks or include red flags, consult a spine specialist for precise diagnosis—because treating the right cause of lower back pain brings real relief.

