That sharp, electric pain shooting down your leg when you stand up. The constant dull ache in your lower back that makes sleeping impossible. If you’re experiencing these symptoms of nerve root irritation, a cortisol shot for back pain could be your path to meaningful relief. Unlike pain pills that mask symptoms throughout your body, this precise treatment delivers anti-inflammatory medication directly to inflamed spinal nerves—often providing months of reduced pain without systemic side effects. Understanding exactly how these injections work, who qualifies, and what to realistically expect can transform your approach to managing debilitating back pain.
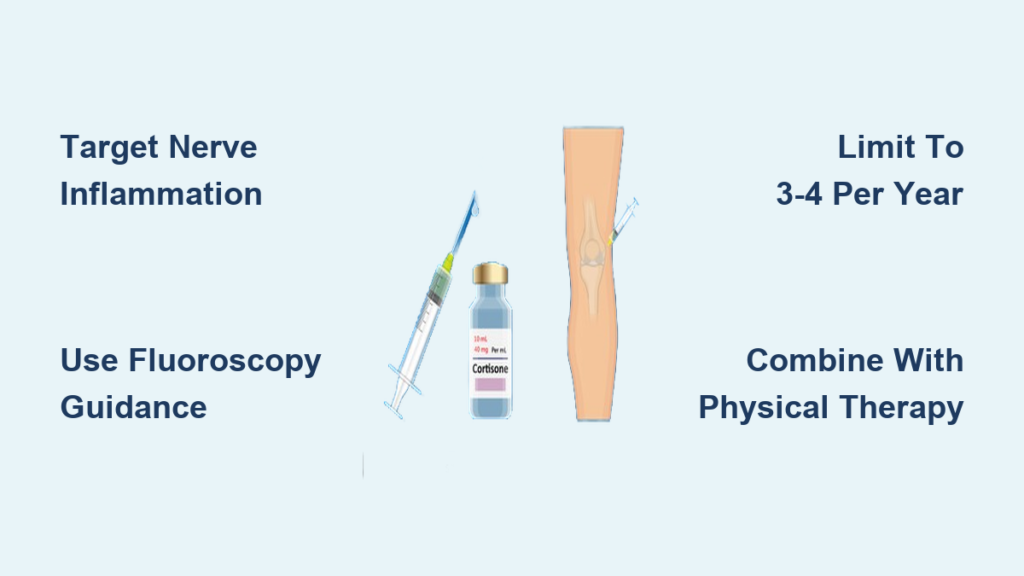
Epidural steroid injections specifically target the source of radicular pain by suppressing inflammation around compressed nerve roots. When inflammation decreases, pressure on nerves subsides, interrupting the pain cycle that keeps you from enjoying simple activities like walking your dog or playing with your kids. This guide cuts through the confusion surrounding cortisol shots for back pain, delivering actionable insights from preparation through recovery so you can make informed decisions about your treatment.
Why Cortisol Shots Target Back Pain at the Source
Cortisol shots combine two critical components working in tandem: a corticosteroid for sustained inflammation control and a local anesthetic for immediate relief. When injected into the epidural space surrounding irritated nerve roots, the corticosteroid suppresses the inflammatory cascade at the cellular level. This directly reduces swelling pressing on nerves responsible for radiating pain, numbness, and muscle weakness down your legs—symptoms that often signal radiculopathy.
Unlike oral medications requiring high doses to achieve localized effects, these injections deliver potent anti-inflammatory action exactly where needed. By addressing the root cause of nerve irritation rather than just masking symptoms, cortisol shots for back pain can break the cycle of chronic discomfort. The local anesthetic provides instant relief during the procedure while the corticosteroid begins its longer-term anti-inflammatory work.
How Inflammation Causes Your Radiating Pain
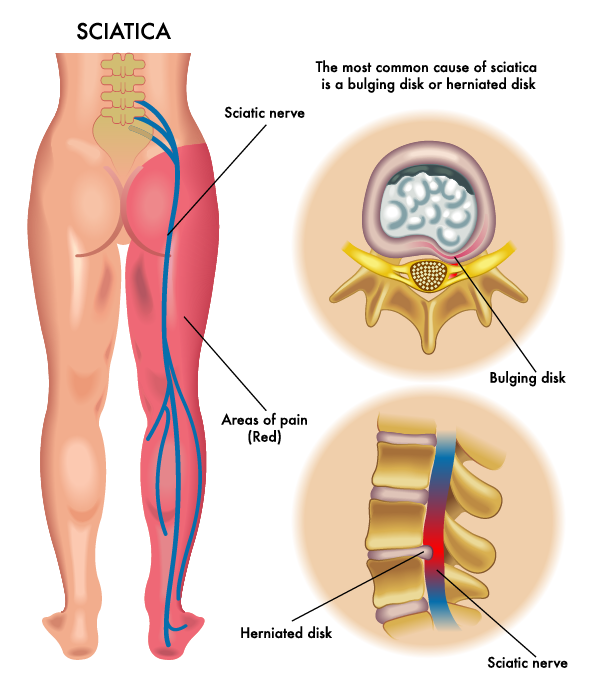
Inflamed nerve roots create pressure that sends pain signals along the entire nerve pathway. When spinal discs herniate or bone spurs develop, they compress nerves exiting the spine, triggering inflammation that amplifies pain signals. This explains why lower back issues often cause leg pain—your sciatic nerve extends from your lower back down each leg. Cortisol shots target this precise inflammation point to reduce nerve compression.
Acute vs. Chronic Pain Response Rates
Your symptom timeline significantly impacts treatment success. Patients with recent-onset radiculopathy (less than 6 weeks) typically experience 60-80% improvement after cortisol shots for back pain. Those with chronic symptoms (over 3 months) show more modest results, as prolonged nerve compression often leads to permanent structural changes. If your radiating pain started after lifting something heavy or sudden twisting, you’re likely an ideal candidate for this targeted approach.
Who Gets the Best Results from Spinal Cortisol Injections
Signs You’re an Ideal Candidate
Your symptoms must clearly indicate nerve root irritation to benefit from cortisol shots for back pain. Look for these specific indicators:
– Radiating pain traveling from your back down your leg (sciatica)
– Numbness or tingling following a specific nerve pathway
– Muscle weakness in your leg or foot corresponding to the affected nerve
– Recent symptom onset (within 4-6 weeks)
– MRI or CT confirmation of nerve root compression
Physicians prioritize patients showing objective neurological signs over those with only back pain. If bending forward triggers leg pain while sitting relieves it, this positional pattern strongly suggests nerve root involvement that responds well to epidural injections.
When to Explore Alternative Treatments
Cortisol shots provide limited benefit for mechanical back pain without nerve involvement. If your pain stays localized to your lower back without radiating symptoms, other approaches may work better. Similarly, patients who’ve received 3-4 previous injections with diminishing returns should consider alternatives like physical therapy or minimally invasive procedures. Structural issues like severe spinal stenosis often require surgical consultation if conservative treatments fail.
Pre-Procedure Checklist: Maximize Safety and Effectiveness
Critical Medication Adjustments
Blood thinners require special attention before your cortisol shot for back pain. You’ll typically need to pause medications like warfarin, clopidogrel, or aspirin for 3-7 days pre-procedure. Don’t stop these without your doctor’s guidance—sudden discontinuation can be dangerous. Also disclose all supplements, as fish oil, ginkgo biloba, and high-dose vitamin E can thin blood. Your pain management specialist will provide specific timing based on your medication regimen.
Infection Prevention Protocol
Report any fever above 100.4°F (38°C) within two weeks before your appointment. Active infections significantly increase complication risks during spinal injections. Your provider will also screen for skin infections near the injection site—if you have cuts, rashes, or boils on your back, they’ll reschedule your procedure. Diabetic patients should ensure blood sugar control beforehand, as high glucose levels impair healing.
What to Wear and Bring
Choose loose, comfortable clothing that allows easy access to your lower back. You’ll change into a gown during the procedure, but comfortable attire makes the process less stressful. Always arrange transportation—you shouldn’t drive for 24 hours post-injection due to potential temporary leg weakness. Bring your complete medication list, insurance information, and someone to drive you home.
Your Step-by-Step Cortisol Injection Experience
Precise Positioning and Numbing
The technician positions you lying on your side or stomach with a pillow under your hips to open spinal spaces. After cleaning your skin with antiseptic, they apply numbing spray or inject local anesthetic to minimize discomfort. You’ll feel brief stinging as the numbing agent takes effect—this initial step prevents more significant discomfort during the main injection.
Real-Time Imaging Guidance
Fluoroscopy (live X-ray) or ultrasound guides needle placement—this is non-negotiable for spinal injections. The radiologist watches the needle advance in real-time to ensure it reaches the epidural space without contacting nerves or blood vessels. You’ll feel pressure but shouldn’t experience sharp pain—if you do, tell your provider immediately so they can adjust.
Medication Delivery and Completion
Once positioned correctly, the corticosteroid-anesthetic mixture slowly enters the target area. The entire procedure takes 15-30 minutes, with most time spent confirming accurate placement. You may feel warmth spreading through your lower back as the medication disperses. After removal, they apply a small bandage and monitor you briefly before discharge.
Recovery Roadmap: From First Hours to Lasting Relief

First 24 Hours: Managing Immediate Effects
Some patients experience facial flushing or chest warmth that resolves within hours. Diabetics should check blood sugar more frequently for 48 hours, as cortisone can temporarily elevate levels. Avoid strenuous activity for the first day—rest but don’t stay completely immobile. Mild soreness at the injection site is normal; apply ice for 15-minute intervals if needed.
The 48-Hour Pain Flare Window
Don’t panic if pain temporarily increases during days 1-2 post-injection. This “cortisone flare” occurs as crystallized medication dissolves, causing brief inflammation. Manage it with:
– Ice application (20 minutes on, 20 off)
– Acetaminophen (avoid NSAIDs unless approved)
– Gentle walking to maintain mobility
When to Expect Real Improvement
True pain relief typically begins around day 6 as the corticosteroid suppresses inflammation. Most patients notice significant improvement by 1-2 weeks, with benefits lasting 3-6 months depending on your condition. If you don’t experience relief after 2 weeks, your pain likely has non-inflammatory causes requiring different treatment.
Critical Safety Information: Side Effects and Limits
:max_bytes(150000):strip_icc()/2549714-article-img-cortisone-shot-side-effects1-5a2ab5caec2f640037439a53.png)
Short-Term Side Effects to Monitor
Temporary effects include:
– Elevated blood sugar (diabetics should monitor closely)
– Sleep disturbances for 1-3 nights
– Mood changes like irritability or anxiety
– Facial flushing lasting hours
These resolve as your body processes the medication. Report severe headaches, fever, or neurological changes immediately—they could indicate rare complications like infection or dural puncture.
Annual Injection Limits for Joint Protection
Never exceed 3-4 cortisol shots per spinal level yearly. Repeated injections risk cartilage damage and tissue weakening. Your provider tracks lifetime exposure to protect your spinal health. If you need frequent injections, they’ll investigate underlying causes and explore alternative treatments.
Making Your Cortisol Shot Last Longer
Smart Activity Management Post-Procedure
For the first week, avoid:
– Heavy lifting (>10 pounds)
– Twisting motions
– Prolonged sitting
– High-impact exercise
Gradually increase activity as pain improves. Start physical therapy within 2 weeks—strengthening core muscles extends injection benefits by reducing mechanical stress on healing nerves.
Preventing Future Flare-Ups
Long-term success requires addressing root causes:
– Maintain healthy weight to reduce spinal load
– Practice proper lifting techniques (bend knees, not waist)
– Use ergonomic chairs with lumbar support
– Incorporate daily core-strengthening exercises
Patients combining injections with lifestyle changes report 50% longer relief periods than those relying solely on medication.
Key Takeaway: A cortisol shot for back pain delivers targeted relief specifically for nerve root inflammation causing radiating symptoms—not general backaches. When administered to ideal candidates (those with recent-onset radiculopathy), these injections can provide months of improved function with minimal systemic effects. Success depends on precise technique, appropriate patient selection, and integration with physical therapy and lifestyle modifications. By understanding the realistic benefits, limitations, and proper preparation for your procedure, you maximize your chance for meaningful, lasting pain reduction without unnecessary risks.