If you’re experiencing stomach discomfort and wondering whether it’s triggering your back pain, you’re navigating a common health concern. Many people with digestive issues notice simultaneous back discomfort and naturally assume a connection. Understanding whether dyspepsia causes back pain requires examining what medical evidence actually tells us about this digestive condition and its symptom profile. This confusion is understandable since upper abdominal pain can sometimes feel like it’s radiating to the back area.
Current medical literature provides a clear picture of dyspepsia symptoms, yet many patients remain uncertain about potential connections to back pain. The truth is that knowing whether dyspepsia causes back pain could prevent unnecessary worry or, more importantly, help you recognize when symptoms might indicate something more serious. In this guide, we’ll clarify what dyspepsia actually involves, why back pain confusion happens, and most crucially—whether dyspepsia causes back pain based on current medical understanding.
What Dyspepsia Pain Actually Feels Like in Your Body
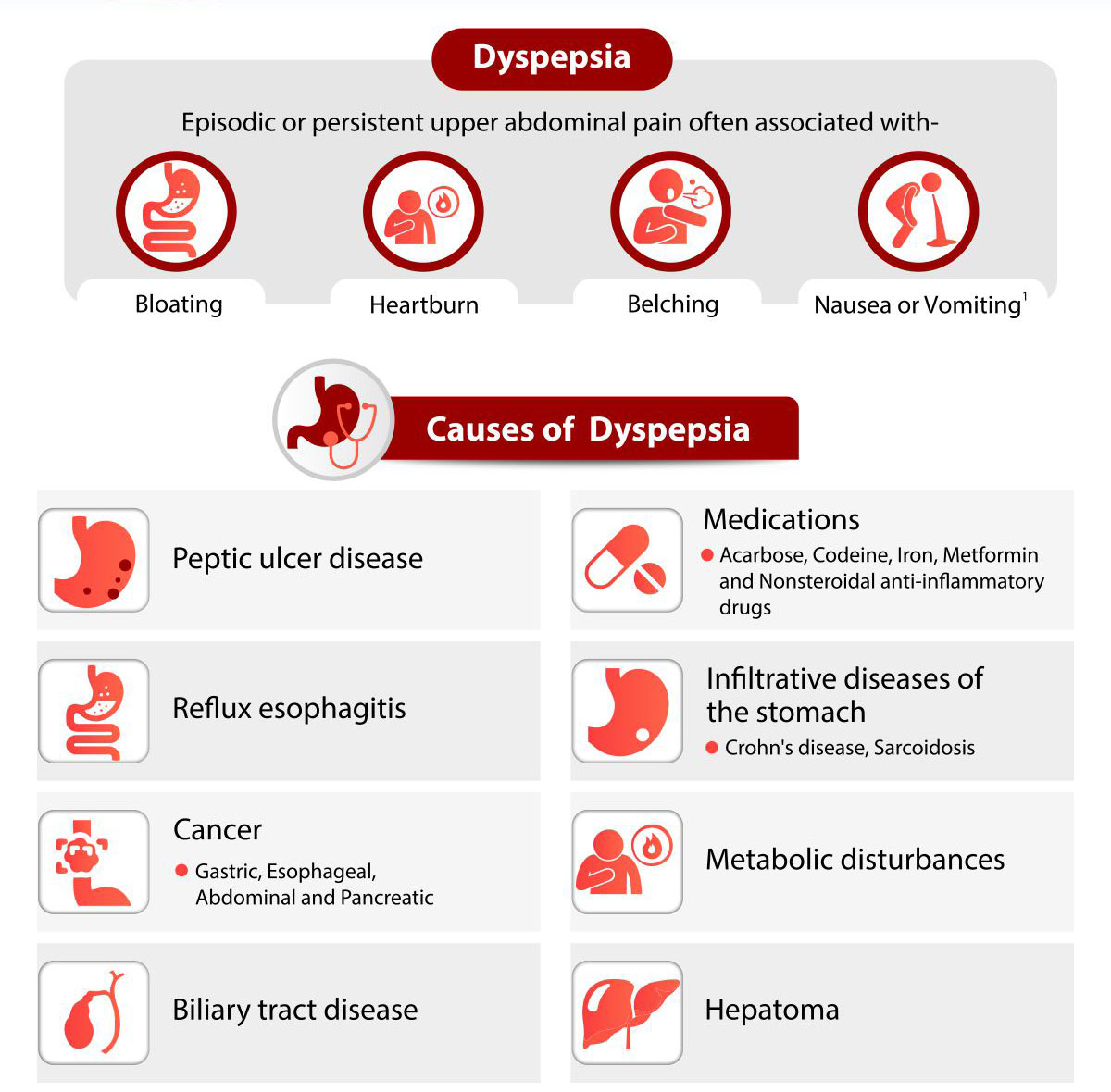
Dyspepsia creates very specific sensations in your upper abdomen that help distinguish it from other conditions. Knowing exactly what dyspepsia feels like prevents misinterpreting your symptoms and wondering whether dyspepsia causes back pain when it likely doesn’t.
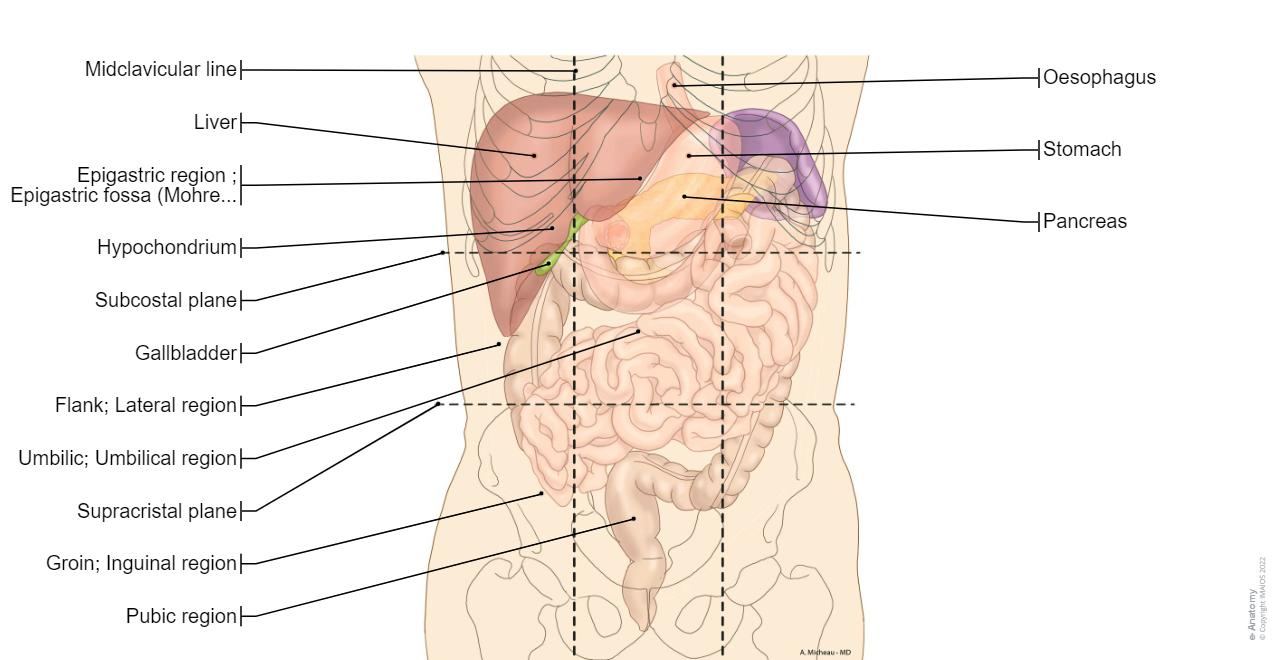
Precise Location of Dyspepsia Discomfort
Dyspepsia pain centers in your epigastric region—the area directly below your breastbone where your ribs converge. This specific location houses your stomach, pancreas, duodenum, and liver. When you experience dyspepsia, you’ll notice symptoms concentrated in this upper abdominal zone rather than your back.
You’ll typically feel:
– Burning sensations that seem to originate deep in your upper stomach
– Pressure or fullness beneath your ribcage that makes you feel uncomfortably stuffed
– Bloating that intensifies after meals
– Early satiety where you feel full after just a few bites
Two Recognized Dyspepsia Symptom Patterns
Medical professionals identify two distinct dyspepsia presentations, both confined to the upper abdomen with no reference to back involvement.
Epigastric Pain Syndrome Characteristics
– Persistent burning pain in your upper stomach
– Heartburn-like sensations behind your breastbone
– Symptoms that occur regardless of when you eat
– Pain that may come and go throughout the day
Postprandial Distress Syndrome Features
– Significant bloating immediately following meals
– Feeling uncomfortably full after eating small portions
– Stomach pain specifically triggered by eating
– Symptoms that consistently worsen after food consumption
Why People Mistakenly Think Dyspepsia Causes Back Pain

The confusion about whether dyspepsia causes back pain stems from anatomical proximity rather than actual symptom connection. Your epigastric region sits directly below your chest cavity, creating the illusion that upper abdominal pain might be back-related.
Understanding the Source of Confusion
When you experience intense epigastric pain, the discomfort can feel like it’s radiating toward your spine. However, medical documentation confirms back pain is not recognized as a symptom of dyspepsia. Comprehensive symptom profiles for both dyspepsia classifications focus exclusively on upper abdominal manifestations without mentioning:
- Pain extending to your thoracic spine
- Lower back discomfort alongside digestive issues
- Radiating pain patterns from your upper GI tract to your back
- Referred pain connections between stomach issues and back pain
Your brain sometimes interprets deep abdominal pain as back pain simply because these areas are close together anatomically. This explains why many patients ask “does dyspepsia cause back pain?” when they’re actually experiencing intense epigastric discomfort.
How to Tell If Your Pain Is Truly Dyspepsia or Something Else
Learning to differentiate between epigastric discomfort and actual back pain helps determine whether dyspepsia causes back pain in your specific case—or if you’re dealing with two separate issues.
Identifying True Epigastric Pain
Epigastric pain from dyspepsia has these distinctive characteristics:
– Location: Directly below your sternum, between your ribcage
– Quality: Burning, gnawing, or pressure-like sensation
– Triggers: Eating certain foods, stress, or sometimes no clear trigger
– Relief: Antacids, avoiding food, or changing to an upright position
Recognizing Actual Back Pain
True back pain presents differently:
– Location: Along your spine or in the muscles alongside it
– Quality: Aching, sharp, or muscle tension feeling
– Triggers: Movement, poor posture, physical activity
– Relief: Stretching, heat application, or changing positions
Simple Self-Check Questions to Answer
Ask yourself these questions to determine whether dyspepsia causes back pain in your situation:
– Does the pain shift when you change positions?
– Does eating make your discomfort better or worse?
– Can you pinpoint the exact location with one finger?
– Does pressing gently on your stomach reproduce the pain?
If your pain worsens after eating and centers below your breastbone, you’re likely experiencing dyspepsia—not back pain caused by dyspepsia.
When Digestive Issues and Back Pain Occur Together
While dyspepsia itself doesn’t cause back pain, certain serious conditions can produce both digestive symptoms and back discomfort simultaneously, creating the false impression that dyspepsia causes back pain.
Conditions That Mimic Dyspepsia But Include Back Pain
Peptic Ulcer Disease
– Severe upper abdominal pain that may radiate to the back
– Pain often worse when stomach is empty
– Back pain only occurs with posterior ulcers (not typical dyspepsia)
Acute Pancreatitis
– Intense upper abdominal pain that reliably radiates to the mid-back
– Pain typically constant and severe
– Often accompanied by nausea and vomiting
Gallbladder Disease
– Right upper abdominal pain that may extend to the right shoulder blade
– Pain frequently triggered by fatty foods
– Nausea commonly accompanies the discomfort
These conditions present differently from typical dyspepsia and require specific medical evaluation.
Warning Signs That Demand Immediate Medical Attention
If you’re wondering whether dyspepsia causes back pain, certain symptoms indicate you should seek prompt medical care regardless of the connection:
- Severe pain that stops you from performing normal daily activities
- Unintended weight loss of 10 pounds or more without trying
- Difficulty swallowing or painful swallowing
- Persistent vomiting lasting more than 24 hours
- Black or bloody stools indicating possible internal bleeding
- Chest pain accompanied by shortness of breath (seek emergency care)
These red flags suggest conditions beyond typical dyspepsia that might explain both digestive symptoms and back pain.
How Doctors Determine If Dyspepsia Causes Back Pain
When patients report both digestive issues and back discomfort, healthcare providers follow a systematic approach to determine if dyspepsia causes back pain or if separate conditions exist.
What to Document Before Your Appointment
- Track symptom timing – Note whether pain relates to meals or occurs independently
- Map pain locations – Draw exactly where you feel discomfort on a body diagram
- Identify triggers – Record activities that worsen or relieve symptoms
- Monitor food connections – Keep a simple food and symptom journal for 3-5 days
Medical Evaluation Process
Your healthcare provider will likely:
– Perform a thorough abdominal examination checking for tenderness
– Assess your spine and back for musculoskeletal causes
– Consider appropriate tests based on your specific symptom pattern
– Rule out serious conditions that could mimic simple dyspepsia
This methodical approach determines whether dyspepsia causes back pain in your case or if you’re experiencing two separate issues.
Practical Strategies for Managing Confirmed Dyspepsia
If your symptoms align with typical dyspepsia without back involvement, these approaches can provide relief and prevent unnecessary concern about whether dyspepsia causes back pain.
Effective Lifestyle Adjustments
- Eat smaller, more frequent meals to reduce stomach pressure
- Avoid common trigger foods like spicy, fatty, or acidic items
- Remain upright for 2-3 hours after eating to prevent reflux
- Practice stress management through deep breathing or meditation
Over-the-Counter Relief Options
- Antacids for immediate symptom relief during acute episodes
- H2 blockers like famotidine for longer-lasting acid reduction
- Proton pump inhibitors for persistent symptoms (use under medical guidance)
Clear Answers About Dyspepsia and Back Pain
Medical literature provides no evidence that dyspepsia causes back pain. The comprehensive symptom profiles for functional dyspepsia focus exclusively on upper abdominal manifestations without any reference to back-related symptoms. This critical fact means when patients ask “does dyspepsia cause back pain,” the evidence-based answer is no.
The anatomical proximity of your epigastric region to your lower chest and upper back explains why some people describe their dyspepsia discomfort as back pain. Careful attention to symptom location, triggers, and characteristics usually clarifies the true source. If you’re experiencing both digestive symptoms and genuine back pain, consider them as potentially separate issues rather than assuming dyspepsia causes back pain.
When managing these symptoms, track your pain precisely for one week, noting exact locations, timing relative to meals, and specific triggers. Share this detailed record with your healthcare provider to determine whether you’re dealing with dyspepsia, back pain, or possibly two distinct conditions requiring individual treatment approaches. This precise documentation prevents misdiagnosis and ensures you receive appropriate care for whatever is truly causing your discomfort.

