That nagging ache in your lower back might not originate where you think. Millions suffer from persistent lumbar discomfort that actually stems from dormant glute muscles—a condition so widespread it’s earned the nickname “dead butt syndrome.” When your glutes fail to activate properly during movement, your lower back muscles compensate, creating a biomechanical chain reaction that leads to chronic pain, poor posture, and reduced mobility. This isn’t just about aesthetics; your glute muscles serve as your body’s primary shock absorbers and stabilizers.
Understanding the glute muscle causing back pain connection could be the missing piece in your pain puzzle. Most people waste months or years treating their back pain directly while ignoring the real culprit: underactive gluteal muscles that have stopped firing properly. In this guide, you’ll discover how to identify if your back pain stems from glute weakness, learn immediate activation techniques that provide relief within days, and implement a targeted strengthening protocol that addresses the root cause of your discomfort.
How Glute Dysfunction Overloads Your Lower Back
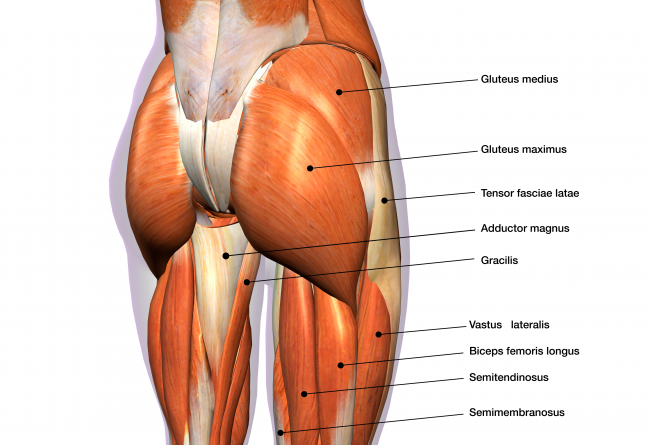
Your gluteus maximus isn’t just for sitting—it’s your body’s largest stabilizer muscle with direct fascial connections to your lower back through the thoracolumbar fascia. When these muscles weaken or become neurologically inhibited, your lumbar spine bears forces it was never designed to handle. Every time you bend to tie your shoes or stand up from your desk chair, your back muscles overwork to compensate for inactive glutes, creating microtrauma that accumulates into chronic pain.
The Compensatory Cascade That Creates Back Pain
When your glutes fail to activate during hip extension movements, your body initiates a dangerous compensation pattern:
- Lumbar over-recruitment: Your back muscles substitute for glute function during basic movements
- Pelvic instability: Your pelvis shifts position, altering spinal alignment
- Hamstring overload: These muscles work overtime, pulling on your sit bones
- Sciatic nerve irritation: Tight piriformis (a deep hip rotator) compresses the sciatic nerve
Notice if your lower back tightens immediately when attempting to perform a proper hip hinge. This is your body screaming that your glutes aren’t doing their job.
Why Sitting Creates “Gluteal Amnesia”
Prolonged sitting is the #1 cause of glute dysfunction leading to back pain. When you sit for hours:
- Hip flexors shorten and tighten
- Gluteal nerves become inhibited
- Your brain literally “forgets” how to activate these muscles
- Lumbar spine muscles take over stabilization duties
After just 90 minutes of continuous sitting, glute activation decreases by 50%—creating immediate biomechanical consequences the next time you stand up.
7 Warning Signs Your Back Pain Comes From Weak Glutes
Daily Movement Clues You Can’t Ignore
Your body sends clear signals when glute weakness causes back pain. Watch for these specific patterns:
- Sit-to-stand pain: Sharp lower back discomfort when rising from chairs or cars
- Morning stiffness: Back pain that improves after 20-30 minutes of movement
- Transition tenderness: Pain when changing positions (sitting to standing, lying to standing)
- Hamstring dominance: Feeling your hamstrings work harder than glutes during stairs or hills
- Standing fatigue: Back pain intensifies after 15-20 minutes of standing
- Hip hiking: One hip rises when walking or balancing on one leg
- Pelvic shift: Noticeable lean to one side when standing for photos
Try this quick test: stand with feet hip-width apart and squeeze your glutes as hard as possible. If you feel your lower back tighten before your glutes engage, you’ve identified the source of your pain.
Three At-Home Diagnostic Tests
The 30-Second Bridge Challenge
– Lie on your back with knees bent, feet flat
– Lift hips until body forms straight line from shoulders to knees
– Hold while keeping abdominal muscles engaged
– Warning sign: If your hamstrings cramp or lower back arches within 15 seconds, your glutes aren’t activating properly
The Single-Leg Stability Test
– Stand on one leg for 30 seconds
– Keep eyes forward, arms at sides
– Warning sign: If your opposite hip drops significantly or you wobble excessively, your gluteus medius is weak
The Chair Rise Assessment
– Sit in a standard chair without armrests
– Attempt to stand using only your glutes (no forward lean)
– Warning sign: If you must use momentum or push off with hands, your glutes aren’t generating sufficient power
10-Minute Daily Routine to Reactivate Dormant Glutes
Phase 1: Glute Awakening (Days 1-14)
Start with these neuromuscular re-education exercises before any strengthening:
Tennis Ball Reset (3 minutes total)
– Place tennis ball under right buttock while lying on floor
– Locate tender spots (avoid bony areas), hold pressure for 30 seconds
– Cross right ankle over left knee for deeper release
– Repeat on left side
– Pro tip: Do this while watching TV to build consistency
Duck Stand Activation (2 minutes)
– Stand with feet hip-width, toes turned out 30 degrees
– Rotate legs externally without moving feet
– Squeeze glutes while maintaining this position
– Hold for 15 seconds, rest 10 seconds, repeat 5 times
– Visual cue: You should feel tension in outer hips, not lower back
Phase 2: Progressive Strengthening (Weeks 3-6)

Glute Bridge Progression
– Beginner: 2 sets of 15 bridges, holding top position for 3 seconds
– Intermediate: Single-leg bridges, 2 sets of 10 per side
– Advanced: Bridge with resistance band above knees, 2 sets of 12
– Critical detail: Squeeze glutes at the top while engaging core—no lower back arching
Reverse Step-Lunge with Rotation (3 sets of 10 each side)
– Step backward off a 6-inch platform
– Rotate chest over front leg while lowering
– Keep front knee behind toes, chest upright
– Time investment: 5 minutes per session
– Warning: Stop immediately if you feel lower back strain
Fix Your Sitting Habits to Prevent Glute Shutdown
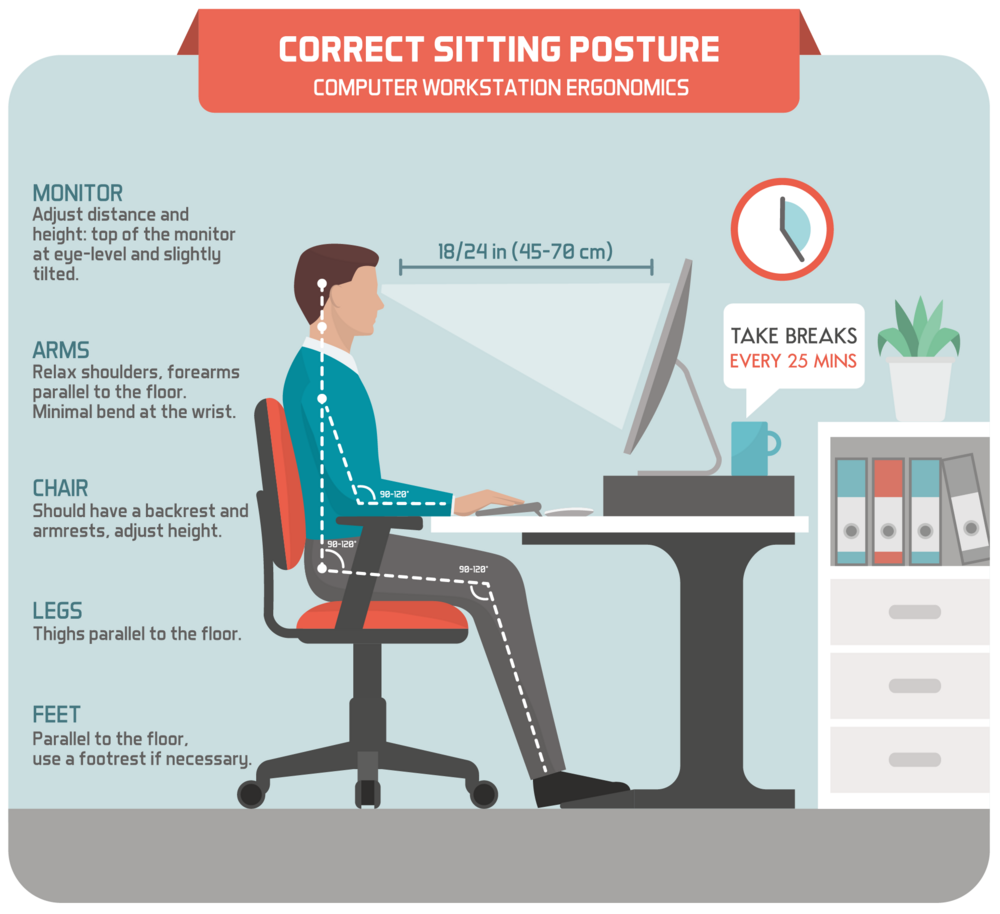
Office Survival Guide for Glute Health
Combat desk-related glute inhibition with these practical solutions:
The 25-5 Rule
– Sit for 25 minutes, then stand for 5 minutes
– During standing breaks: perform 10 bodyweight squats focusing on glute activation
– Set phone timer as reminder—your glutes will thank you within days
Chair Modifications That Work
– Place small rolled towel under sit bones to maintain pelvic neutrality
– Use standing desk for at least 2 hours daily
– Sit on stability ball for 30-minute intervals to engage core and glutes
Posture Reset Sequence (2 minutes every hour)
1. Hip flexor release: Kneel on one knee, tuck pelvis, hold 30 seconds each side
2. Glute firing: Stand tall, squeeze glutes hard for 10 seconds (5 reps)
3. Walking reset: 1 minute of purposeful walking, focusing on heel-to-toe roll
When to Consider Advanced Recovery Options
SoftWave Therapy for Stubborn Cases
If you’ve followed activation protocols for 4+ weeks with minimal improvement, consider these clinic-based treatments:
SoftWave Acoustic Therapy Benefits
– Breaks down fascial restrictions between glutes and lower back
– Stimulates nerve regeneration for improved muscle activation
– Reduces inflammation at cellular level
– Typical protocol: 6-8 sessions over 4-6 weeks (10-15 minutes per session)
Red Light Therapy Integration
– Use before exercise for activation (10 minutes)
– Apply after workouts for recovery (20 minutes)
– Target gluteal region directly with 660nm wavelength devices
– Cost-effective alternative: Home units starting at $200 provide clinic-like results
Daily Maintenance Protocol for Permanent Relief
Morning Activation Routine (4 minutes)
- 20 bodyweight squats (focus on sitting back into heels)
- 15 glute bridges (squeeze at top for 3 seconds)
- 30-second plank with conscious glute contraction
- Pro tip: Perform these before breakfast for maximum neural activation
Weekly Self-Assessment Checklist
- Bridge endurance: Can you hold bridge position for 60 seconds without lower back strain?
- Single-leg strength: Perform 15 single-leg bridges each side without wobbling?
- Functional test: Complete 10 deep squats with proper form and no back pain?
Critical Red Flags Requiring Professional Help
Seek immediate care if you experience:
– Bilateral leg numbness (affecting both legs)
– Bladder or bowel dysfunction
– Progressive leg weakness over several days
– Night pain preventing sleep for multiple consecutive nights
For persistent glute-related back pain, follow this professional pathway:
1. Start with: Exercise physiologist for comprehensive movement assessment
2. Progress to: Physical therapist specializing in glute activation protocols
3. Advanced cases: Sports medicine physician for diagnostic imaging if needed
The 3-Step Protocol That Ends Glute-Related Back Pain
Your glutes serve as your body’s primary defense against lower back pain—not just for appearance but for fundamental spinal protection. When weak glutes cause back pain, the solution isn’t more back exercises but rather targeted glute reactivation and strengthening. Most people experience noticeable pain reduction within 10-14 days of consistent glute activation work, with full recovery typically taking 6-8 weeks.
Begin with daily neuromuscular activation exercises to wake up dormant glutes, progress to controlled strengthening movements that build functional capacity, and maintain your results with strategic movement breaks throughout the day. Remember: your back pain might be shouting for attention, but your silent glutes are often the real conversation starters. Fix your foundation, and everything above it—including your pain—will finally find relief.