You twist to grab your toddler and suddenly freeze—a sharp, immobilizing ache locks your lower back. Instantly, you’re counting the hours: How long will this back pain take to heal? You’re not alone. Eight out of ten adults face this question after a strain from lifting, poor sleep posture, or even a sneeze. The urgent truth? Most acute back pain resolves faster than feared—yet recovery timelines swing wildly based on your injury type, age, and immediate actions. Ignoring early warning signs can turn a 2-week setback into months of discomfort. This guide cuts through the guesswork with medically verified healing milestones, so you know exactly what to expect and how to accelerate your return to pain-free movement.
Stop wondering when you’ll sit comfortably again or lift groceries without wincing. We’ve mapped the precise progression from Day 1 agony to full recovery using evidence-based data. You’ll discover why 90% of acute cases heal within 6 weeks, when to worry about chronic pain, and the exact treatments that slash recovery time by 50%. Whether you’re an athlete, senior, or new parent, this roadmap puts you in control of your healing journey.
Acute Back Pain Recovery Timeline
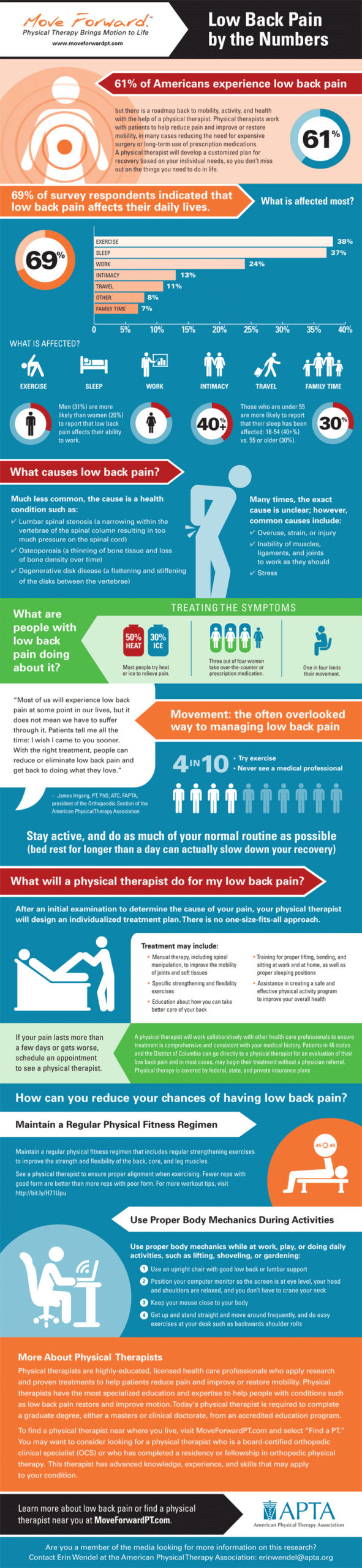
Most sudden back pain follows a predictable healing arc if managed correctly. During Days 1–3, inflammation peaks as your body protects damaged tissues—making simple tasks like standing from a chair intensely painful. This critical phase requires smart movement, not complete rest. By Days 4–7, expect 30–50% pain reduction as swelling decreases. You’ll likely walk short distances again but avoid twisting motions that reignite spasms.
Week 2–3 marks your functional turning point. Pain typically drops to a manageable 3/10, allowing sitting for 30+ minutes and light chores. This is when consistent progress separates quick healers from those stuck in limbo. If you’re not hitting these markers, investigate treatment options immediately. By Week 4–6, 90% of acute cases achieve near-total resolution—returning to work, exercise, and normal life. Pushing too hard too soon risks setbacks, so honor your body’s pace.
Subacute vs Chronic Back Pain Duration
When Healing Stalls Beyond Six Weeks
If pain persists past 6 weeks but under 3 months, you’ve entered the subacute phase—a warning zone where 20–30% of acute cases get trapped. Here, recovery isn’t automatic; it demands targeted intervention like physical therapy. Without action, mild strains evolve into stubborn pain cycles. The silver lining? With consistent treatment, most still heal within 6–12 weeks. Track milestones like walking without limping or sleeping through the night—these signal you’re on track.
Chronic Pain Realities After Three Months
Beyond 12 weeks, the goal shifts from cure to management. Only 30–40% achieve complete pain elimination, but functional improvement remains possible over 6–18 months. Key indicators like consistent 2/10 pain levels during daily tasks signal progress. Crucially, chronic pain doesn’t mean permanent disability—75% gain significant function with multidisciplinary care (physical therapy, pain psychology, and movement retraining). Don’t resign yourself to suffering; seek specialists who treat pain as a complex condition, not just a symptom.
Healing Factors That Speed or Slow Recovery
Your Age Matters More Than You Think
Healing speed plummets after 40. Adults 20–40 typically resolve muscle strains in 2–4 weeks thanks to robust tissue repair. Between 40–60, add 1–2 weeks to standard timelines as collagen production slows. Over 60, anticipate 50% longer recovery—6–10 weeks for similar injuries—due to reduced blood flow and bone density. Yet seniors can still heal well with modified protocols: gentle water aerobics replaces high-impact exercises, and vitamin D supplementation supports bone health.
Injury Type Dictates Your Exact Timeline
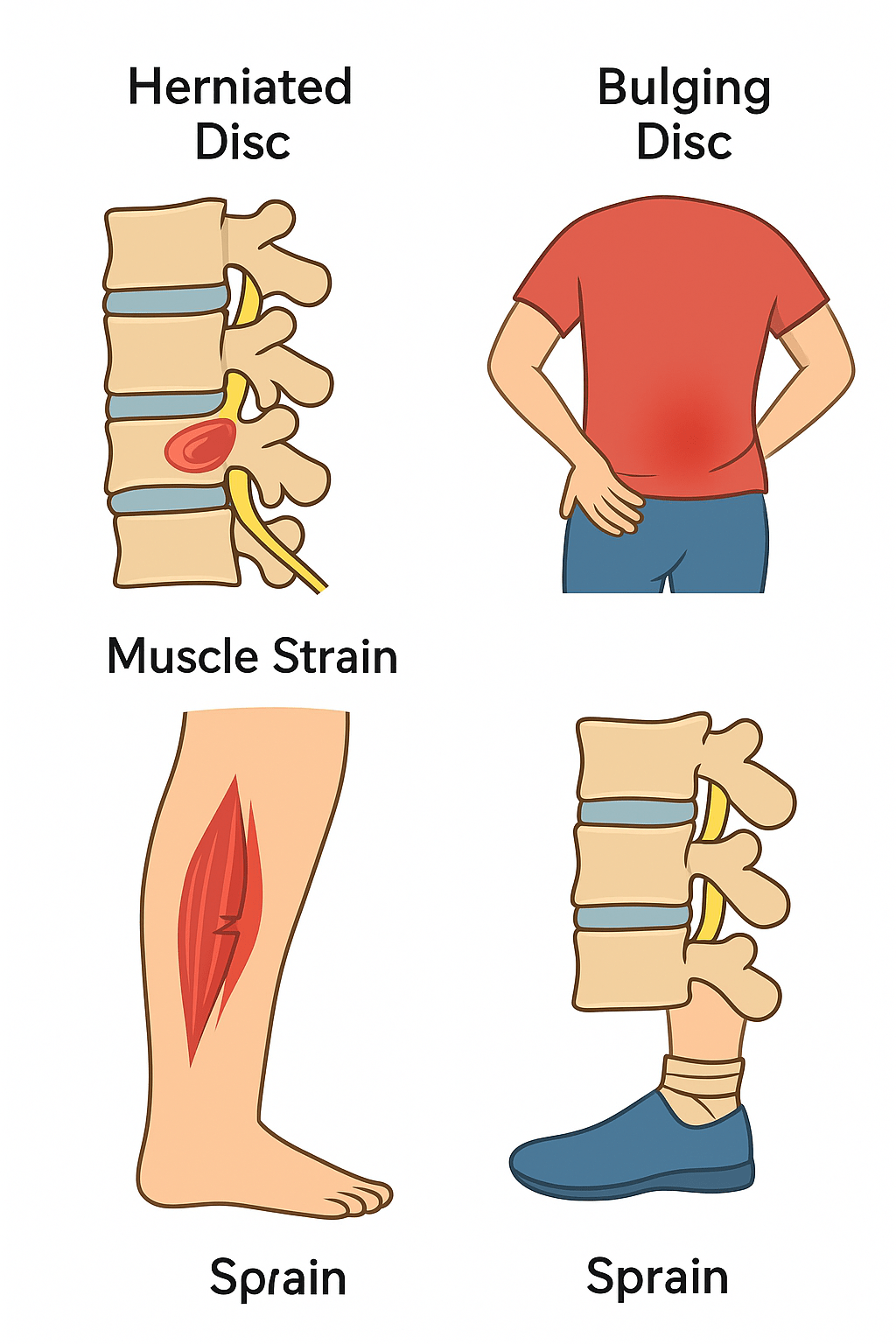
Not all back pain heals equally. A minor muscle strain (1–3 weeks) demands different care than a herniated disc (4–12 weeks). Sciatica from nerve compression takes 4–12 weeks depending on severity—sharp leg pain means slower healing than localized back aches. Crucially, severe disc injuries require patience; rushing into heavy lifting before Week 8 often causes relapses. Match your recovery plan to your specific diagnosis, not generic advice.
Treatment Speed Multipliers
Seeking help within 48 hours slashes healing time by 30–50%—this narrow window prevents protective muscle spasms from becoming chronic. Physical therapy delivers the fastest results: 60% achieve full recovery by Week 4 with guided movement retraining. Conversely, waiting over a week extends recovery by 1–2 weeks, while untreated cases risk chronic pain (40% develop persistent issues). Skip passive treatments like prolonged bed rest—active care like walking and targeted stretches accelerates tissue repair far more than pills or ice alone.
Recovery Milestones to Track Progress
Week 1–2 Checkpoints That Predict Success
Monitor these tangible signs: Can you walk 500 feet without stopping? Does pain drop 30% when lying flat? Improved sleep quality is a critical indicator—waking only once nightly versus hourly. Missing these suggests inadequate treatment. If pain hasn’t decreased by Day 7, consult a specialist; delays here often prolong recovery by weeks.
Week 6–8 Goals for Full Function
By this stage, you should carry groceries without grimacing and sit through a movie. Pain becomes occasional (2/10) rather than constant, flaring only after overexertion. Work capacity hits 80–100% of pre-injury levels—key for avoiding disability cycles. If not, reassess your rehab: weak core muscles often undermine progress. A single physical therapy session can correct technique flaws stalling your recovery.
Warning Signs of Delayed Healing
Red Flag Timeline Markers Needing Urgent Action
Zero improvement after 2–3 weeks of proper care demands medical evaluation—this signals possible nerve compression or structural damage. Worse, pain that initially eases then rebounds sharply suggests improper healing. New numbness in legs or foot weakness requires same-day assessment; these indicate worsening nerve issues. Ignoring these signs risks permanent damage, turning a 6-week recovery into a 6-month ordeal.
Psychological Barriers Doubling Your Pain Duration
Depression or anxiety can double healing time by amplifying pain perception. Work dissatisfaction or fear of re-injury creates mental blocks that physically slow tissue repair. Address these early: cognitive behavioral therapy reduces chronic pain risk by 50% when combined with movement therapy. Don’t dismiss emotional strain—it’s as critical as physical treatment.
Accelerate Healing: Week-by-Week Protocol
Immediate Actions (First 48 Hours)
Apply ice for 15 minutes hourly to reduce inflammation—skip heat initially, which increases swelling. Take NSAIDs like ibuprofen with food to avoid stomach irritation. Most crucially, practice relative rest: move gently within pain limits (e.g., slow walking) but avoid aggravating activities. Sleep with a pillow under your knees if back-sleeping or between legs if side-sleeping—this maintains spinal alignment overnight.
Week 3–6 Progression That Prevents Relapse
Introduce bird-dog exercises (on hands and knees, extend opposite arm/leg) to rebuild core stability without strain. Return to work with ergonomic tweaks: a lumbar cushion for chairs or standing desks for desk jobs. Add swimming or cycling for low-impact cardio—these boost blood flow to healing tissues without jarring your spine. Stop any exercise causing radiating pain; it’s your body’s stop sign.
Special Population Considerations
Athletes: Avoid the “Almost Good” Trap
Your fitness gives a 25% healing edge, but returning to sport too soon guarantees reinjury. At Week 4, test with sport-specific drills: can you lunge without pain? If not, delay full return. Football players need 8–12 weeks for cutting movements; weightlifters require 10–16 weeks before heavy deadlifts. A sports physical therapist designs drills mimicking your sport’s demands—this targeted approach prevents 70% of recurrences.
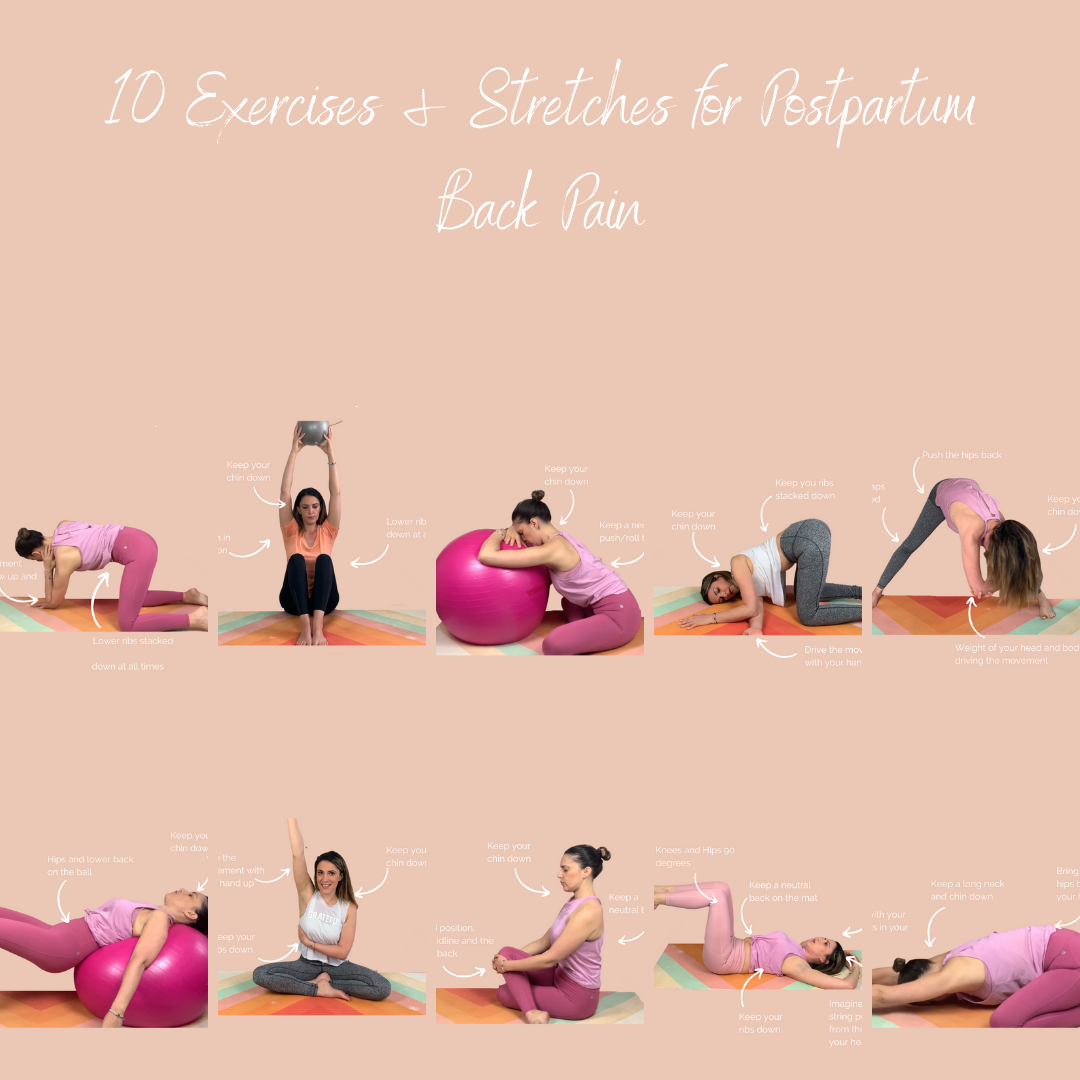
Pregnancy-Related Pain: Hormones Change the Clock
Postpartum recovery varies wildly due to lingering relaxin hormones that loosen ligaments. While some heal in 6 weeks, others take 6 months—especially with multiples or C-sections. Safe strategies include pelvic tilts (on back with knees bent, flatten spine toward floor) and avoiding baby-carrying twists. Postpartum physical therapy cuts healing time by 40%, focusing on diastasis recti repair and posture.
Bottom Line: Your back pain timeline hinges on precise factors, but most acute cases resolve within 4–6 weeks with smart action. The critical keys? Start gentle movement within 48 hours, match treatment to your injury type, and track weekly milestones like walking distance or sitting tolerance. If pain persists beyond 3 weeks or shows red flags like leg numbness, seek specialized care immediately—delays turn manageable pain into chronic disability. Remember, 90% of people fully recover; your proactive choices today determine whether you’re in that majority or the 10% facing long-term struggles. Start your healing roadmap now, not “when it gets worse.”

