Your back aches relentlessly, your mind races with worry, and you desperately search for answers: “How long will this pain last?” This is one of the most common questions people ask when they realize their back pain might be connected to anxiety. Unfortunately, medical science hasn’t established a reliable timeline for how long anxiety-related back pain typically persists. Unlike a muscle strain with predictable healing phases, anxiety-induced back pain defies simple duration estimates because it involves complex interactions between your nervous system, muscular system, and psychological state.
When anxiety triggers physical symptoms like back pain, it creates a frustrating cycle where physical discomfort fuels more anxiety, which then intensifies the pain. People experiencing this often feel confused and frustrated when they can’t find clear answers about recovery timeframes. The truth is, searching for a specific number of days or weeks this pain will last sets you up for unnecessary disappointment. Instead, understanding why duration varies so dramatically—and focusing on actionable management strategies—provides a more realistic path forward.
Research reveals that anxiety back pain stems from physiological processes like muscle tension, heightened pain sensitivity, and nervous system activation. However, no credible medical studies have established standardized duration patterns for this specific pain type. This isn’t due to lack of interest—rather, the inherent complexity of separating psychological factors from physical symptoms makes creating universal timelines impossible. Your unique biology, stress history, coping mechanisms, and even belief systems all interact to create a pain experience that’s highly individualized.
Why Anxiety Back Pain Duration Defies Simple Timelines
The Individual Variability Factor
Your anxiety back pain duration depends on factors that make each person’s experience unique. Some people notice relief within hours of implementing calming techniques, while others experience symptoms for extended periods. This variation occurs because anxiety affects physical symptoms differently based on genetic predispositions, past trauma, current stress load, and even cultural background. Two people with identical anxiety scores might have completely different pain durations simply because their bodies process stress in distinct ways.
The Challenge of Isolating Anxiety as the Sole Cause
Medical professionals struggle to determine exactly how long anxiety back pain lasts because it rarely exists in isolation. Most people have a combination of factors contributing to back pain—poor posture, physical inactivity, previous injuries, or structural issues—that intertwine with anxiety’s effects. This complexity makes it impossible to isolate anxiety as the single cause and measure its specific pain duration. When you search for “how long does anxiety back pain last,” you’re asking a question that medical science currently cannot answer with precision because real-world cases involve multiple overlapping factors.
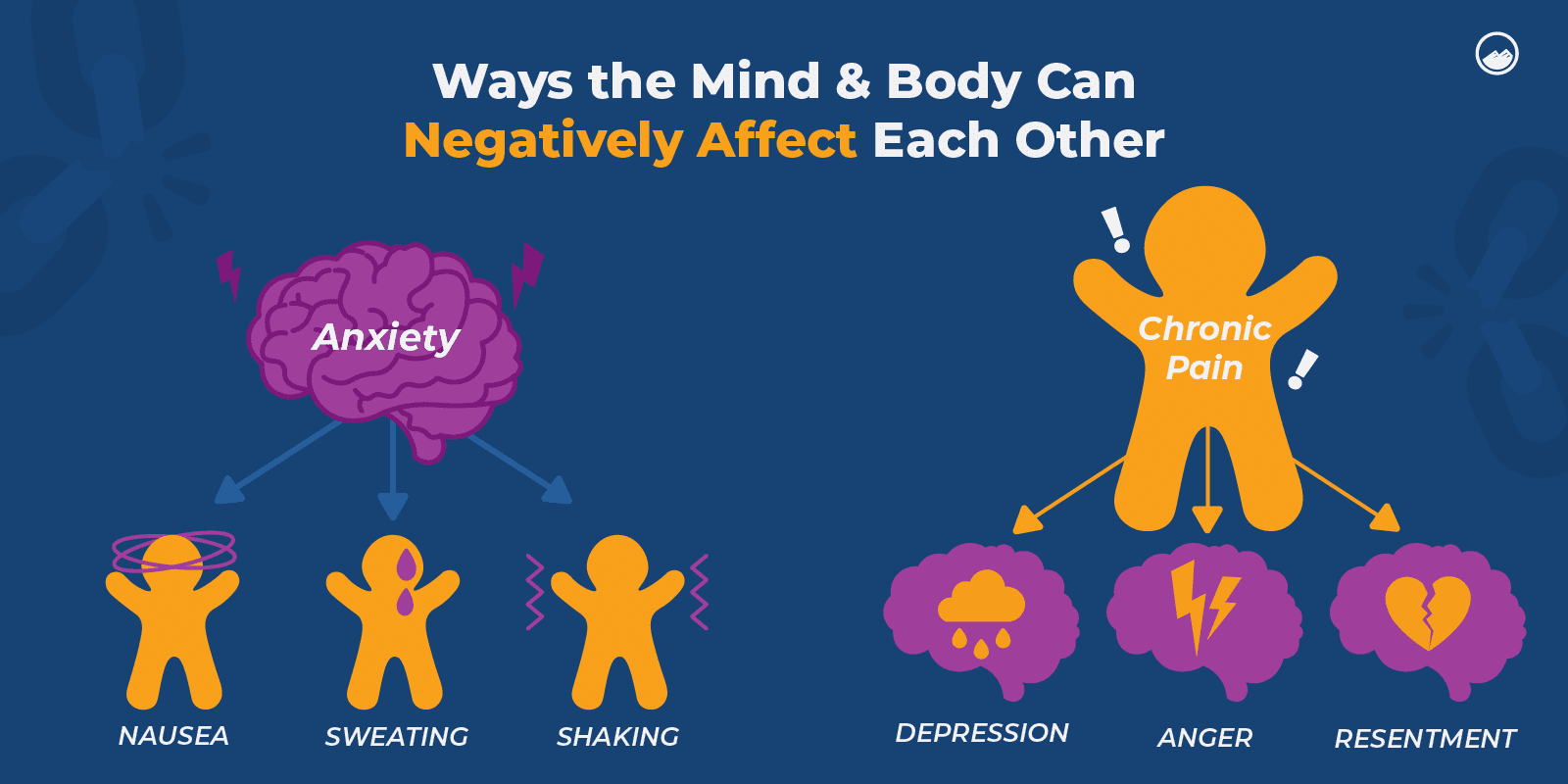
The Dynamic Nature of Mind-Body Connection
Unlike a physical injury with predictable healing stages, anxiety back pain operates within a constantly shifting system. Your pain levels can fluctuate dramatically within a single day based on stressors, sleep quality, and even your expectations about pain. This fluidity means that even if someone could establish an “average” duration, it wouldn’t reliably predict your personal experience. The mind-body connection works in real-time, making your pain duration less about fixed timelines and more about your ongoing response to stressors.
Recognizing and Managing Your Unique Pain Pattern
Identifying Anxiety-Related Back Pain Signals
While we can’t predict how long your pain will last, you can learn to recognize patterns specific to anxiety-induced back pain. Look for these telltale signs: pain that intensifies during stressful situations but eases during relaxation, discomfort that moves around your back rather than staying in one spot, and symptoms that worsen with emotional distress but improve with calming activities. Keeping a symptom journal that notes your pain levels alongside emotional states and stressors helps identify your personal triggers and responses—more valuable than seeking a universal timeline.
Immediate Action Steps That Work Regardless of Duration
Stop waiting for a countdown timer on your recovery and start implementing these evidence-based strategies today. When pain strikes, practice diaphragmatic breathing for five minutes: inhale deeply through your nose for four counts, hold for seven, and exhale slowly through pursed lips for eight. This immediately activates your parasympathetic nervous system, reducing muscle tension. Combine this with gentle movement—walking slowly while focusing on relaxing your shoulders—to break the anxiety-pain cycle within minutes, regardless of how long your overall symptoms might persist.
Tracking Your Personal Progress Indicators
Since universal timelines don’t apply, create your own meaningful benchmarks for improvement. Notice subtle changes like: “I could sit through dinner without adjusting my posture,” “My morning stiffness lasted 10 minutes instead of 30,” or “I noticed tension building and released it before it became painful.” These personalized indicators provide more relevant progress markers than arbitrary duration expectations. Document these small victories daily—they reveal your unique healing trajectory better than any generic timeline ever could.
When to Seek Professional Guidance

Warning Signs Beyond Anxiety-Related Pain
While anxiety can cause significant back discomfort, certain symptoms require immediate medical evaluation regardless of duration concerns. Seek prompt attention if you experience bowel or bladder changes, numbness in your saddle area, pain that wakes you from sleep, or weakness in your legs. These red flags indicate potential neurological issues that need evaluation separate from anxiety management. Understanding these distinctions prevents dangerous delays in appropriate treatment while acknowledging that most anxiety-related back pain doesn’t follow predictable timelines.
Building a Targeted Support Team
Create a care approach that addresses both physical and psychological components without promising specific durations. Work with a physical therapist who understands the mind-body connection and a mental health professional experienced in somatic symptoms. This collaborative approach focuses on functional improvement rather than arbitrary timeframes—helping you regain activities you’ve avoided rather than counting days until “recovery.” Professionals versed in this intersection recognize that progress isn’t linear and avoid making duration predictions that could undermine your confidence.
Creating Sustainable Management Strategies

Developing Your Personal Response Protocol
Design a customized action plan that responds to your unique pain-anxiety patterns. For example: “When I notice tension building in my upper back during work, I’ll take three deep breaths, perform shoulder rolls, and walk to get water.” Having specific, practiced responses ready reduces the fear of pain persistence. Include both physical interventions (gentle stretches, heat application) and cognitive techniques (reframing anxious thoughts) tailored to your most common triggers. This proactive approach puts you in control regardless of how long symptoms might last.
Integrating Preventive Wellness Practices
Shift your focus from duration concerns to building resilience against future episodes. Incorporate daily practices that address both anxiety and physical tension: 10 minutes of mindfulness meditation upon waking, regular movement breaks if you sit for work, and weekly activities that promote both physical and emotional release like yoga or nature walks. Consistency matters more than intensity—even five minutes daily of targeted practice creates meaningful change over time. These habits build your capacity to handle stress before it manifests physically, reducing both frequency and intensity of symptoms.
Reframing Your Relationship with Pain
The most powerful shift you can make is changing how you perceive your pain. Instead of asking “How long will this last?” ask “What is my body trying to communicate?” and “What can I do right now to respond supportively?” This mindset transformation reduces the secondary anxiety about pain duration that often worsens symptoms. When you stop fighting against your experience and start working with it, many people find their symptoms become more manageable—even if they don’t follow a predictable timeline.
Bottom Line: The question “how long does anxiety back pain last” reflects our natural desire for certainty, but the reality is more complex than any timeline can capture. Rather than fixating on duration—which varies too widely to predict—focus on developing responsive strategies that work within your unique experience. By tracking your personal patterns, implementing targeted interventions, and building resilience through consistent practice, you gain control over your symptoms regardless of how long they persist. Remember that progress with anxiety-related pain isn’t measured in days until “cure” but in increased functionality, reduced intensity, and greater confidence in managing symptoms as they arise. Your journey isn’t about waiting for pain to end—it’s about reclaiming your life while navigating discomfort with growing skill and self-compassion.

