That sharp twinge in your lower back after deadlifts isn’t just another workout ache—it’s your body screaming for attention. Whether you’re a weekend warrior or seasoned lifter, lower back pain can derail your fitness journey faster than any plateau. The good news? Most exercise-induced back pain responds beautifully to targeted fixes, not extended couch time.
This guide walks you through a systematic approach to eliminate workout-related back pain and prevent it from returning. You’ll learn exactly what’s causing your pain, how to fix it step-by-step, and which gym mistakes to avoid forever. How to fix lower back pain from working out starts with understanding your specific pain triggers and implementing the right recovery protocol immediately.
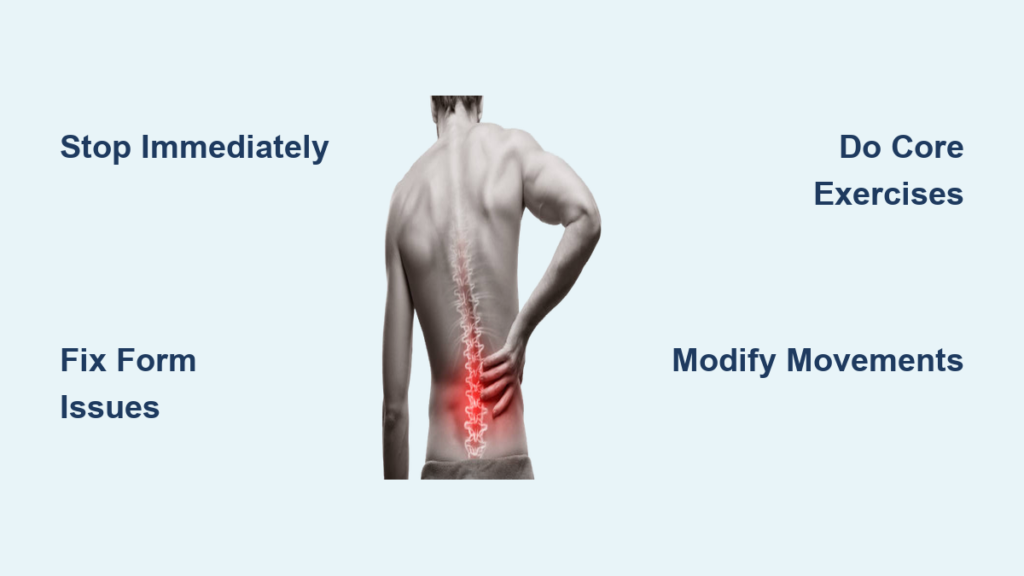
Stop Workout Pain Immediately
First 48 Hours Protocol
When back pain strikes mid-workout, stop immediately. Continuing through pain turns minor irritation into major injury. Apply ice wrapped in a towel for 15-20 minutes every 2-3 hours during the first two days—never apply ice directly to skin. Take ibuprofen (200-400mg) or naproxen (220mg) following package directions, but avoid heat which increases inflammation.
Keep gentle movement with short walks every few hours. This prevents stiffness without aggravating injured tissues. If pain spikes above 7/10 or you experience numbness down both legs, seek medical care immediately. Rest doesn’t mean complete immobilization—gentle movement promotes blood flow to healing tissues while avoiding positions that increase pain.
Pain Scale Assessment
Rate your pain honestly from 1-10. Red flag symptoms demanding immediate medical attention include numbness in groin or inner thighs, loss of bladder/bowel control, fever with back pain, or pain after significant trauma. Distinguish muscle pain (aching, localized tenderness) from nerve pain (sharp, shooting sensations). Note which movements trigger pain—this guides your recovery strategy.
Document your pain triggers in a workout journal. Did it happen during deadlift lockout? When rising from a squat? This specificity helps tailor your recovery approach. Pain during movement doesn’t automatically mean damage—it’s often your nervous system signaling improper mechanics that need correction.
Identify Your Pain Source

Movement Pattern Failures
Your back pain rarely originates from your back. Anterior pelvic tilt—that excessive lower back arch with protruding belly—creates chronic lumbar stress during squats and deadlifts. This stems from tight hip flexors overpowering weak glutes.
Gluteal amnesia forces your lower back muscles to do the glutes’ job during hip extension. Watch for this during deadlifts when your lower back arches instead of your hips driving forward. Film yourself lifting to catch these subtle form breakdowns before they cause pain.
Exercise-Specific Risks
Deadlifting with rounded spine generates dangerous shear forces on spinal discs. Squatting with excessive forward lean shifts your center of gravity, overloading lumbar extensors. Overhead pressing with hyperextended back compresses posterior vertebral elements.
Sit-ups with anchored feet create 3,300 Newtons of compressive force—more than most heavy deadlifts. High-impact activities on hard surfaces transmit shock waves through already irritated tissues. Identify which movements consistently trigger your pain to modify or eliminate them from your routine.
4-Phase Recovery Timeline
Phase 1: Acute Recovery (Days 1-7)
Focus solely on pain reduction and gentle mobility. Perform supine pelvic tilts: lie on your back, knees bent, gently flatten your lower back into the floor by tilting your pelvis. Hold 5 seconds, repeat 15 times.
Execute cat-camel stretches on hands and knees, slowly alternating between arching and rounding your spine through pain-free ranges. Add diaphragmatic breathing: lie on your back, hands on your belly, breathe deeply expanding your abdomen for 5-10 minutes daily. Avoid any movements causing pain beyond mild discomfort during this critical healing phase.
Phase 2: Restore Mobility (Weeks 2-4)
Address restrictions while maintaining pain-free movement. Hip flexor stretches in half-kneeling position: kneel on one knee, other foot forward, shift hips forward until you feel the stretch in front of your back hip. Hold 30 seconds each side.
Hamstring stretches lying on your back: loop a towel around your foot, straighten your leg while keeping your back flat on the floor. Add bird-dog exercises: from hands and knees, extend opposite arm and leg while maintaining neutral spine. Progress only when you can complete exercises without pain—rushing this phase causes setbacks.
Phase 3: Build Stability (Weeks 4-8)
Develop core endurance and motor control. Progress to dead bug exercises: lie on your back, arms and legs in the air, lower opposite arm and leg while keeping your back flat against the floor.
Implement side planks: lie on your side, prop up on your forearm, lift hips creating a straight line. Start with 20-second holds. Add hip hinge practice with a dowel rod held against your spine to maintain three contact points. Focus on quality over quantity—perfect execution of 10 repetitions beats sloppy execution of 20.
Phase 4: Strength Integration (Weeks 8-12)
Restore functional patterns with progressive loading. Begin bodyweight squats focusing on hip hinge initiation and neutral spine. Progress to Romanian deadlifts with light dumbbells, emphasizing perfect hip hinge mechanics.
Reintroduce compound movements at 50-60% of previous loads, prioritizing form over weight. Single-leg work like split squats and step-ups rebuild stability while maintaining pelvic alignment. Track your progress with video analysis to ensure proper mechanics as loads increase.
Essential Corrective Exercises
:max_bytes(150000):strip_icc()/BasicBridgeExcercise_annotated-e564888866a746b8bbe02c9a9acbf3e5.jpg)
Core Activation Sequence
Start with supine abdominal hollowing: lie on your back, gently draw your navel toward your spine without moving your pelvis. Hold 10 seconds for 10 repetitions.
Progress to prone planks starting on knees, advancing to full planks with leg lifts. Pallof presses using cables or bands: stand perpendicular to resistance, press handle straight out resisting rotation. Perform these exercises before every workout to activate key stabilizers and prevent pain recurrence.
Glute Activation Protocol
Glute bridges progress from double-leg to single-leg variations. Clamshells with resistance band: lie on your side, knees bent 90 degrees, open top knee while keeping feet together. Lateral band walks with mini-band around ankles maintain athletic stance.
Activate your glutes before lifting with 2 sets of 20 banded clamshells. This simple step prevents gluteal amnesia during compound lifts. Feel the burn in your glutes, not your lower back—that’s the sign you’re doing it right.
Modify Problem Exercises
Squat and Deadlift Fixes
Reduce squat depth to pain-free range using box squats for consistent depth. Elevate bar height during deadlifts using blocks or trap bar variations. Replace sit-ups with dead bugs or plank variations.
Substitute overhead movements with landmine presses or incline dumbbell presses. Modify running by increasing cadence to 170-180 steps per minute, reducing stride length. Your workout should challenge you without punishing your back—adjust exercises to match your current capabilities.
Programming Adjustments
Reduce training volume by 50-60% during return phases. Extend warm-up to 15 minutes including dynamic mobility work. Increase rest periods to 3-4 minutes between heavy sets. Include core and hip activation work before every session.
Tempo matters—slow down the eccentric (lowering) phase of lifts to 3-4 seconds. This builds strength through full ranges of motion without excessive compressive forces. Start lighter than you think you need and progress only when pain-free.
Prevention Framework
Pre-Workout Protocol
Begin with 5 minutes light cardio, then dynamic hip circles, leg swings, and torso rotations. Perform 15 glute bridges, 20 clamshells each side, 10 bird-dogs before loading. Practice unloaded versions of planned exercises focusing on perfect form.
Your warm-up should mirror your workout—if deadlifting, practice hip hinges with a broomstick. If pressing overhead, perform thoracic rotations. This neural priming reduces injury risk by 30% according to strength research.
Movement Quality Standards
Maintain neutral spine during all loaded movements using mirrors or video feedback. Exhale during exertion phases to enhance core stability. Control eccentric phases to reduce injury risk. Limit range of motion to maintain proper pelvic alignment.
Film yourself lifting monthly to catch subtle form breakdowns before they become pain generators. Your spine should remain in neutral position throughout lifts—no excessive arching or rounding.
Daily Recovery Habits
15-20 minutes daily mobility focusing on tight areas identified through movement screens. Foam rolling 2-3 times weekly for hip flexors, glutes, and thoracic spine. Sleep 7-9 hours nightly to support tissue recovery. Walk 8,000-10,000 steps daily distributed throughout the day.
Recovery isn’t passive—it’s an active process of addressing imbalances before they become problems. Pain is preventable with consistent maintenance, not just something to fix after it happens.
When to Seek Professional Help
Immediate Medical Care
Seek emergency care for severe pain following trauma, progressive weakness or numbness, or loss of bowel/bladder control. Fever with back pain or pain worsening beyond 48-72 hours despite rest requires evaluation.
Don’t ignore neurological symptoms—tingling, numbness, or weakness that travels down your legs indicates nerve involvement needing professional assessment. Early intervention prevents chronic issues that take months to resolve.
Professional Resources
Physical therapists specializing in sports medicine provide movement analysis and corrective exercises. Sports chiropractors offer manual therapy and joint mobilization. Certified strength coaches refine technique and program design. Persistent pain beyond 6 weeks warrants medical imaging.
Invest in expert guidance—a single session with a qualified professional can identify issues you’ve missed for months. Your body is worth the investment for long-term pain-free training.
Bottom line: Most workout-related lower back pain resolves with systematic approach to movement quality, not extended rest. Start with Phase 1 regardless of your fitness level, progress only when pain-free, and never sacrifice form for heavier weights. Your back will thank you with years of pain-free training ahead. Implement these how to fix lower back pain from working out strategies consistently, and you’ll build resilience that keeps you lifting pain-free for the long haul.