Eight out of ten adults will experience back pain this year—yet most find relief without surgery or strong drugs. Whether you woke up stiff after gardening or aggravated an old injury, targeted self-care can calm spasms and restore mobility within days. The key? Combining movement, positioning, and evidence-based techniques to relax tense muscles and reduce nerve irritation. This guide delivers actionable steps you can start today to quiet back pain, backed by clinical research showing exercise and posture adjustments outperform prolonged rest for 85% of cases with no structural cause.
Ice First, Heat Later for Immediate Relief
Stop Inflammation Fast With Ice
Apply ice packs within the first 72 hours of sharp pain onset—this slashes inflammation and numbs nerve signals. Wrap frozen peas or a gel pack in a thin towel, then position it over your lower back for 20 minutes. Wait 40 minutes before reapplying, repeating 3–4 times daily. Stop immediately if your skin turns bright red or feels numb, as this indicates tissue damage. Never place ice directly on skin; the cold must penetrate gradually to avoid frostbite while calming micro-tears in strained muscles.
Switch to Heat After Day 3
Once acute inflammation subsides (around day 4), swap ice for gentle heat to boost blood flow and relax stubborn knots. Use a heating pad set to low for 15–20 minutes, or try a warm shower targeting your lower back. Never sleep with a heating pad—this risks severe burns even on low settings. For deeper relief, pair heat with the “Supine Hamstring Stretch”: lie on your back, loop a towel around one foot, and gently straighten your leg until you feel a mild pull. Hold 30 seconds, then switch sides. This combo softens tight muscles pulling your spine out of alignment.
Safe Movement Beats Bed Rest Every Time
Break the Pain-Immobilization Cycle
Prolonged bed rest worsens back pain by weakening core muscles and stiffening joints—limit reduced activity to 1–2 days maximum. Start moving as soon as you can tolerate it, even if just walking to the bathroom. Each step pumps nutrient-rich fluid into spinal discs while preventing scar tissue formation. If pain spikes above 5/10 during movement, pause and return to ice therapy before trying again. Remember: mild soreness is normal, but sharp or radiating pain means you’ve pushed too far.
Build Your Walking Tolerance Gradually
Begin with 5-minute walks at a slow pace around your home, focusing on tall posture—imagine a string pulling your head toward the ceiling. Add 2–3 minutes every other day, aiming for 20–30 minutes daily within two weeks. Stop immediately if pain shoots down your leg or you feel numbness in your feet—these signal nerve compression needing medical evaluation. Outdoor walks on soft surfaces like grass further reduce spinal load compared to hard floors. Consistent walking improves pain scores by 40% in chronic cases within 8 weeks, per clinical studies.
Fix Sitting and Standing Posture in Minutes

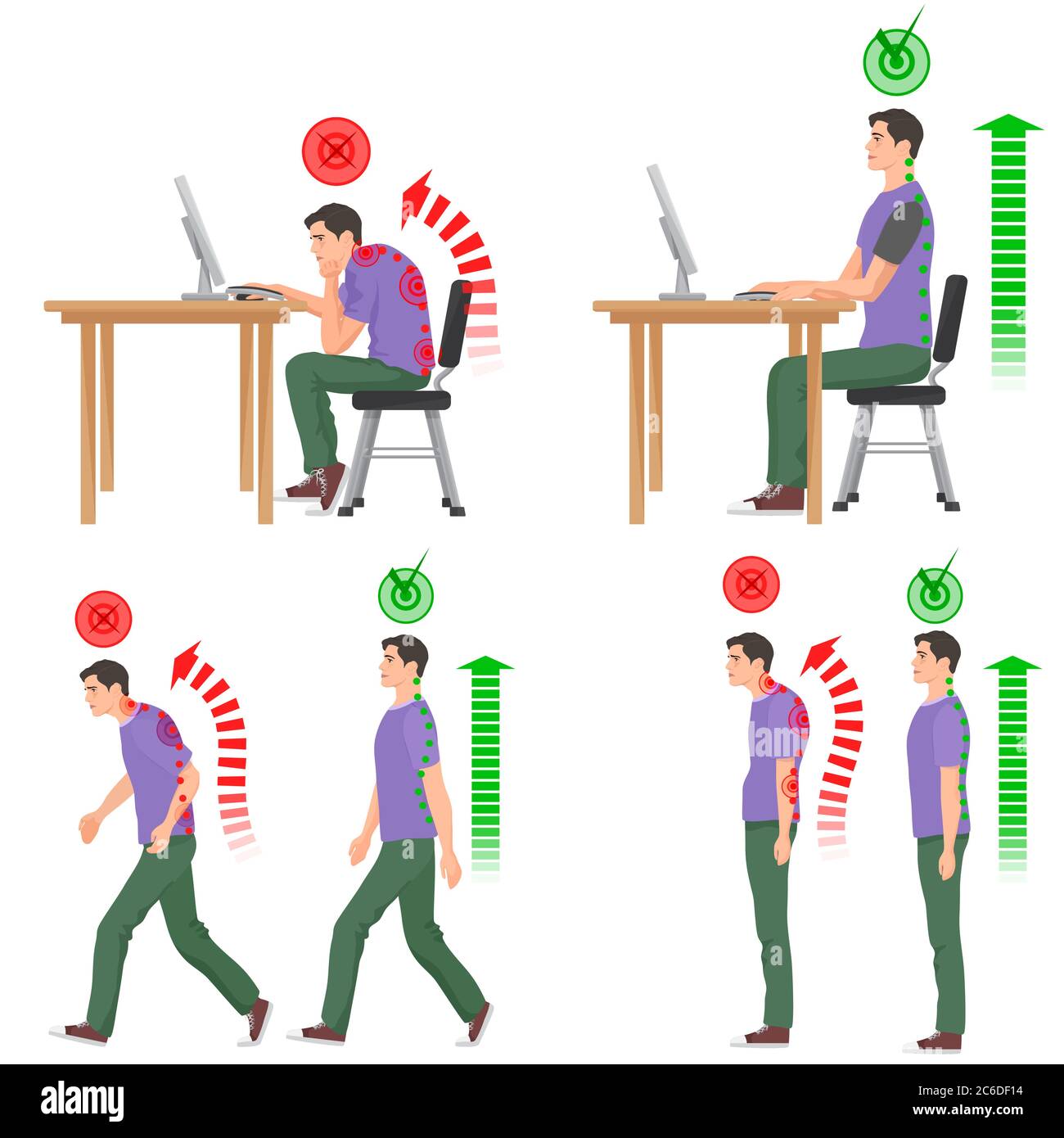
Transform Your Workspace in 60 Seconds
Place a rolled towel at the curve of your lower back while sitting—this maintains your spine’s natural “S” shape. Position your hips and knees at 90°, feet flat on the floor, and set a phone timer to stand every 15 minutes. Laptop users: stack books under your screen until the top third aligns with your eyes to avoid forward head tilt. These tweaks prevent disc compression from slouching, which increases spinal pressure by 40% versus standing.
Reset Your Standing Stance Instantly
When waiting in line or cooking, distribute weight evenly on both feet and tuck your hips under slightly to eliminate swayback. Gently engage your core as if zipping a tight pair of jeans—this activates stabilizing muscles without straining. Shift weight side-to-side every minute to prevent stiffness. Avoid locking your knees; a micro-bend in joints reduces disc pressure by 25% during prolonged standing.
5-Minute Stretch Routine for Morning Stiffness
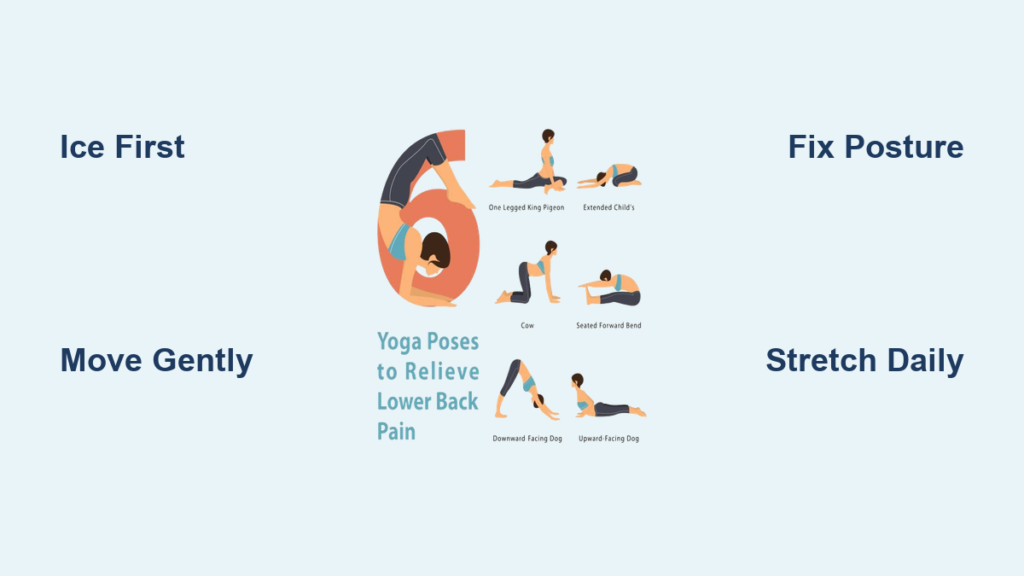
Wake Up Your Spine With These Moves
Start your day with Knee-to-Chest (30 seconds per leg) to decompress lumbar discs, followed by Lower Back Rotations (roll bent knees side-to-side 5 times) while keeping shoulders glued to the floor. Finish with Cat-Camel on hands and knees: arch your back toward the ceiling like a Halloween cat (hold 3 seconds), then sag downward like a swayback horse (hold 3 seconds). Repeat 10 times. These target the multifidus muscles—the deep stabilizers that shut down during pain flares.
Wind Down With Evening Release
Before bed, hold Child’s Pose for 30 seconds (knees wide, big toes touching, arms reaching forward) to stretch your entire back chain. Follow with Supine Hamstring Stretches (30 seconds per leg using a towel) and Diaphragmatic Breathing: lie flat, hand on belly, inhale for 4 seconds (expanding abdomen), exhale for 6 seconds (drawing navel toward spine). Repeat 6 cycles. This sequence reduces overnight muscle guarding by calming the nervous system.
Core Stability Exercises That Actually Work
Master the Bridge for Pelvic Control
Lie on your back, knees bent, feet flat. Tighten your abs and glutes, then lift your hips until your body forms a straight line from knees to shoulders. Hold for 3 breaths while pressing your lower back into the floor—never arch excessively. Start with 5 reps, building to 3 sets of 15. This targets the transverse abdominis, your body’s natural “corset” that stabilizes the spine during movement.
Perfect Bird Dog for Balance
On all fours, extend your right arm and left leg until level with your torso. Hold 5 seconds while keeping your hips square to the floor—imagine balancing a tray on your back. Return slowly and switch sides. Begin with 5 reps per side, progressing to 3 sets of 10. This trains anti-rotation stability critical for lifting safely. Stop if you feel lower back strain; reduce range until your core engages properly.
Sleep Positioning Hacks for All-Night Relief
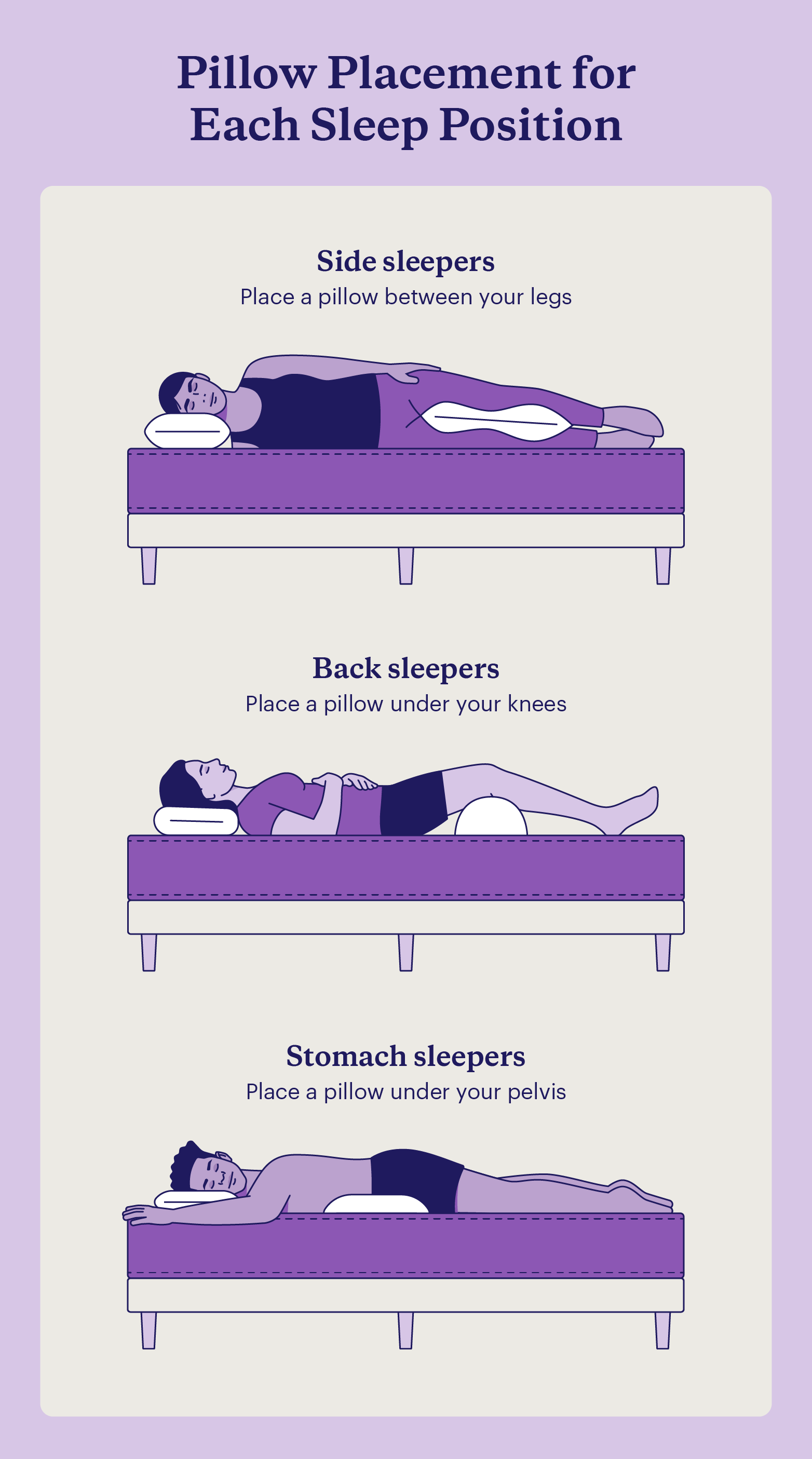
Side-Sleepers: Pillow Power
Place a firm pillow between your knees to prevent hip rotation that twists your spine. Keep knees bent slightly toward your chest and hug a second pillow to avoid shoulder rolling. If pain persists, try the “fetal position” with knees drawn toward your navel—this opens spinal joints by 15%.
Back-Sleepers: Lumbar Support Is Key
Slide a pillow under your knees to reduce disc pressure by 30%. Add a small lumbar roll (a rolled towel works) if your mattress sags. Avoid thick pillows that push your head forward—this strains neck muscles connected to your upper back. Place a pillow under your ankles if legs feel heavy overnight.
When OTC Medications Help—and When They Don’t
Smart NSAID Use for Inflammation
Take ibuprofen (200–400 mg) with food every 6–8 hours only for the first 3–5 days to avoid stomach damage. Never exceed 2400 mg daily. If NSAIDs upset your stomach, switch to topical creams with menthol that cool surface nerves without internal side effects. Crucially: meds mask pain but don’t fix the cause—pair them with movement to prevent chronicity.
Red Flags That Require a Doctor
Seek immediate help for groin numbness, leg weakness, or loss of bladder control—these signal cauda equina syndrome. Also consult a professional if pain lasts over 6 weeks despite daily walking and stretching. Most cases improve within 4 weeks with consistent self-care, but imaging (like MRI for nerve issues) may be needed if red flags emerge.
Long-Term Prevention: Your 15-Minute Daily Plan
Commit to this sequence every morning: 2-minute walk warmup, 10 bridges, 10 bird dogs per side, 15 cat-camels, and 2 minutes of diaphragmatic breathing. Progress slowly—increase reps by 10% every 3 days only if pain stays below 5/10. Add swimming or Iyengar yoga twice weekly to build resilient core strength. Quit smoking and lose 5–10 pounds if overweight; every 10-pound loss reduces spinal load by 40 pounds during movement. Hydrate well—discs are 80% water and need fluid to stay shock-absorbent.
Final Takeaway: Most back pain relaxes fastest with movement, not rest. Start today with the 5-minute morning stretch routine and strict 15-minute sitting breaks. Ice first, then heat; walk daily; and master the bridge exercise. If numbness, weakness, or pain beyond 6 weeks occurs, get evaluated—but 90% of cases resolve with these consistent, drug-free steps. Your spine heals best when you move it intelligently, not avoid it.