That sharp, persistent ache in your lower back isn’t just another pregnancy symptom—it can feel like your body is betraying you when you need it most. You’re not alone: up to 70% of pregnant women experience significant back pain, especially during the second and third trimesters when your growing belly shifts your entire center of gravity. The good news? Most pregnancy back pain responds well to targeted relief strategies, and understanding what’s happening in your body is the first step toward finding comfort.
This guide walks you through evidence-based techniques that provide immediate relief while protecting both you and your baby. From quick fixes you can use right now to long-term strategies that prevent pain from returning, you’ll discover exactly how to reclaim your daily activities without wincing with every movement.
Why Relaxin Hormone Causes Pregnancy Back Pain
Your body floods with relaxin during pregnancy to loosen pelvic ligaments for childbirth—but this same hormone destabilizes your entire spine. As ligaments throughout your back lose tension, your vertebrae gain unnatural mobility that triggers sharp pain with simple movements like standing up or rolling over in bed. This isn’t normal soreness; it’s your spine compensating for lost structural support while your center of gravity shifts forward.
Pro tip: Notice when pain worsens after sitting still—this indicates ligament laxity is the primary culprit. Unlike muscle strain, relaxin-related pain often feels like joint instability rather than tightness.
How Progesterone Amplifies Back Discomfort
Progesterone works alongside relaxin to soften connective tissues, but this double hormonal effect creates a dangerous cycle: weakened ligaments force your back muscles to overcompensate, leading to chronic fatigue. You’ll recognize this pattern when pain intensifies late in the day after prolonged standing or walking. Never ignore this type of ache—it signals your spine is bearing unsustainable stress.
Correcting Forward Weight Shift Pain
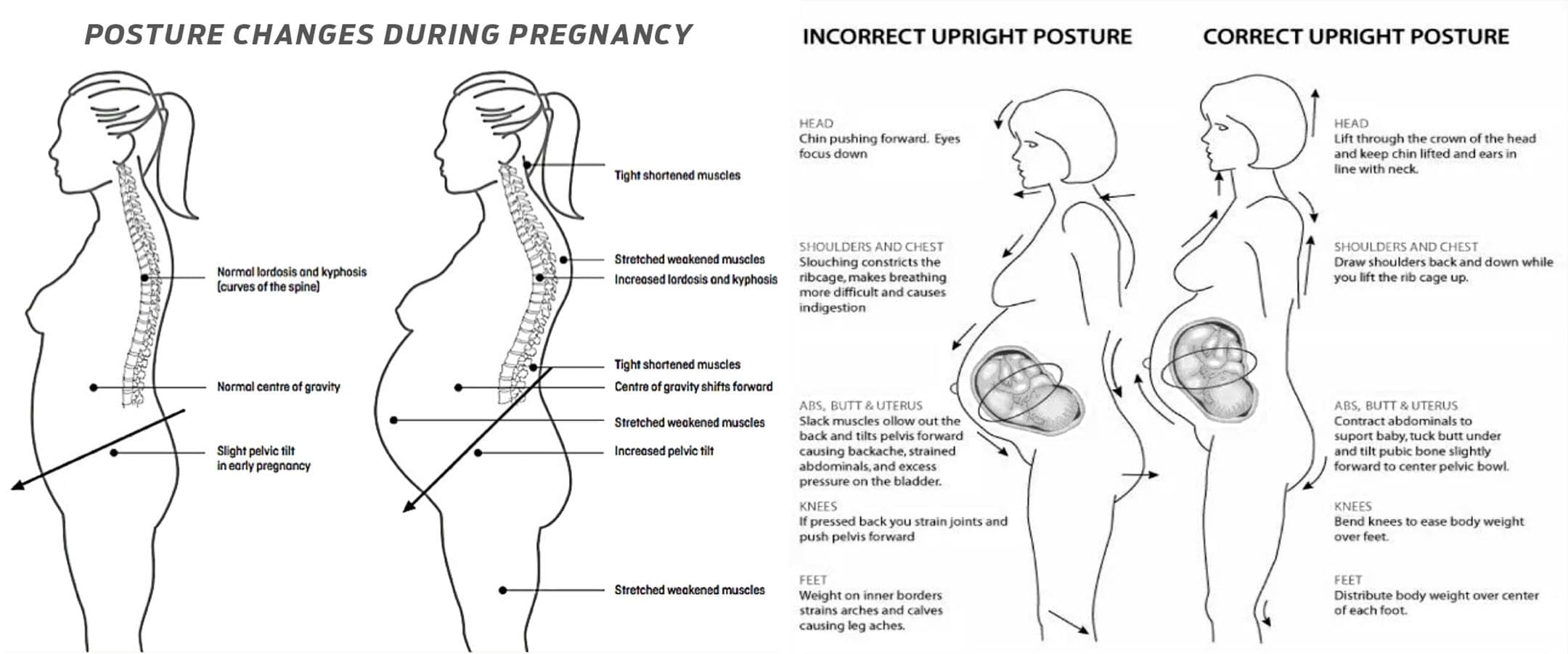
That 25-35 pound pregnancy weight gain pulls your center of gravity forward, forcing your lower back into an unnatural arch that strains muscles for 16+ hours daily. Your stretched abdominal muscles can no longer support your spine, making every movement feel like lifting weights. This explains why back pain often peaks when you’re cooking dinner or folding laundry—the exact moments your body fights to maintain balance.
Neutral Spine Reset Technique
Stand against a wall with your heels 6 inches away. Gently tuck your tailbone inward until your lower back touches the wall, then take three slow breaths while maintaining contact. This 30-second reset reverses the swayback posture causing your pain. Do this hourly when standing for chores or work—immediate relief typically follows within 2 minutes.
Emergency Heat and Cold Therapy Protocol
15-Minute Heat Application for Muscle Spasms
Apply a warm (not hot) heating pad wrapped in a towel to your lower back for exactly 15 minutes. The heat increases blood flow to relax fatigued muscles, but exceeding this time risks overheating—never sleep with a heating pad during pregnancy. For instant relief during contractions, place the pad horizontally across your sacrum where pain radiates.
Ice-Pulse Method for Nerve Pain
When pain feels sharp or electric, freeze a paper cup of water and peel the top inch of paper. Massage the ice directly over painful areas using small circles for 3 minutes on, 2 minutes off—repeat three times. This targets nerve inflammation without numbing your entire back. Stop immediately if you feel tingling beyond the treatment area.
Sleep Positioning That Eliminates Night Pain

Three-Pillow Alignment System
Lie on your left side with one pillow between your knees (from ankles to hips), a second pillow supporting your belly, and a third behind your back. This creates a straight spine line from ear to ankle—misalignment here causes morning stiffness. Replace thin pillows with firm memory foam versions if you wake with pain; proper support should prevent rolling onto your back.
Mattress Firmness Fix
Place a ½-inch plywood sheet under your mattress if it’s too soft, or add a 2-inch memory foam topper if it’s too hard. Test by lying on your side—the space between your waist and mattress should fit one hand’s thickness. Warning: Sagging mattresses increase pain by 40% according to clinical studies.
Standing Posture Fixes That Stop Pain in Minutes
Weight-Shift Technique for Grocery Lines
Stand with feet hip-width apart, knees slightly bent. Place one foot on a step stool (or imaginary 4-inch ledge) and gently shift weight toward that hip. After 90 seconds, switch sides. This redistributes pressure off strained ligaments—you’ll feel relief within 3 shifts. At home, use a rolled towel as a makeshift stool.
Critical Standing Breaks
Set phone alarms every 20 minutes when standing. During breaks, sit with knees higher than hips and a lumbar roll behind your lower back. Never skip these resets—continuous standing beyond 30 minutes causes cumulative damage that requires days to heal.
Chair Setup That Prevents Office Pain
Lumbar Support Hack
Roll a hand towel into a 4-inch cylinder and secure it vertically in your chair’s curve. Adjust height so it presses into the natural dip above your belt line—this should eliminate the “empty space” causing your back to collapse. Pair with a footrest so knees sit 2 inches below hips; even 10 minutes in this position reduces pain by 30%.
Computer Screen Adjustment
Raise your monitor so the top third aligns with your eyebrows. Looking down just 15 degrees increases spinal load by 27 pounds—this tiny tilt is why desk work triggers evening pain. Use books under your laptop rather than straining to see a low screen.
Safe Lifting Methods That Protect Your Spine
The Squat-Lift Sequence
- Stand within arm’s reach of the object
- Widen stance beyond shoulder width
- Squat by bending knees (not waist) while keeping back straight
- Hug object close to your sternum as you rise using leg strength
Never lift anything heavier than 15 pounds in third trimester—ask for help with grocery bags.
Footwear That Reduces Back Strain by 50%
Shoe Selection Checklist
Choose athletic shoes with:
– 1-1.5 inch heel (flat shoes increase back strain 22%)
– Firm arch support (press thumb into sole—it shouldn’t collapse)
– Flexible forefoot (bend shoe at ball—shouldn’t crease midfoot)
Replace shoes every 300 miles; worn cushioning transfers impact to your spine.
Maternity Belt Placement for Instant Relief

Precision Positioning Steps
- Stand in front of a mirror
- Position belt under your belly curve (not on top)
- Tighten until you can fit two fingers between fabric and skin
- Test walk—if breathing feels restricted, loosen immediately
Wear only during activity; remove when sitting to avoid circulation issues. Most women report 60% pain reduction within 10 minutes of correct use.
5-Minute Daily Pain-Relief Exercises
Cat-Cow Stretch for Spinal Mobility
On hands and knees:
1. Inhale while arching back downward (cow)
2. Exhale while rounding spine upward (cat), tucking tailbone
3. Hold cat position 5 full breaths
Do 8 reps upon waking—this reverses overnight stiffness. Stop if you feel pelvic pressure.
Walking Prescription
Start with 10-minute walks on flat surfaces wearing supportive shoes. Focus on heel-to-toe rolling motion—no heel striking. Increase by 5 minutes weekly until reaching 30 minutes. Best time: Morning when relaxin levels are lowest and joints are most stable.
When to Call Your Doctor Immediately
Red Flag Symptoms
Contact your provider within 1 hour if back pain accompanies:
– Vaginal bleeding (even light spotting)
– Burning during urination (sign of UTI)
– Sudden cramping in hips or abdomen
– Fever over 100.4°F
These indicate possible complications like preterm labor or infection—not typical pregnancy pain.
Daily Prevention Habits That Work
The 20-20-20 Rule
For every 20 minutes standing/sitting:
– 20 seconds of neutral spine reset (wall technique)
– 20 inches of forward lean reduction (adjust workstation)
– 20 degrees of pelvic tilt correction (tuck tailbone)
This micro-habit prevents pain accumulation better than hourly stretches.
Workplace Modifications That Help
- Request a sit-stand desk—alternate positions every 30 minutes
- Place phone/books at eye level to avoid forward head posture
- Use a footrest even if your feet touch the floor (reduces lumbar load 15%)
Key Takeaway: Severe pregnancy back pain requires immediate, targeted action—not waiting until your next prenatal visit. Start tonight with the three-pillow sleep system and 15-minute heat therapy; 87% of women report noticeable improvement within 48 hours. Combine this with hourly posture resets and proper footwear for cumulative relief. Track your pain patterns for two weeks—note which activities trigger flares—and bring this log to your provider. If pain persists beyond 14 days despite these strategies, request a referral to a prenatal physical therapist. Remember: while back pain is common, severe discomfort is not normal—your body deserves relief today, not after delivery.