That familiar ache in your lower back greets you before your feet even touch the floor each morning. As a perimenopausal woman, you’re not imagining this pain—it’s a direct consequence of hormonal shifts weakening your spinal support system. How to treat menopause back pain starts with understanding that estrogen decline accelerates disc degeneration while progesterone reduction lowers your pain tolerance. The good news? Targeted interventions can rebuild strength and restore comfort within weeks.
This guide delivers clinically proven strategies addressing the root causes: hormonal impacts on spinal structures, muscle loss, and posture changes. You’ll discover exactly which exercises rebuild core stability, how to adjust your sleep environment for pain relief, and when medical interventions become necessary—all based on current evidence. No more guessing; just actionable solutions that align with your body’s changing needs.
Why Hormone Shifts Cause Lower Back Collapse
Estrogen Loss Directly Weakens Spinal Structures
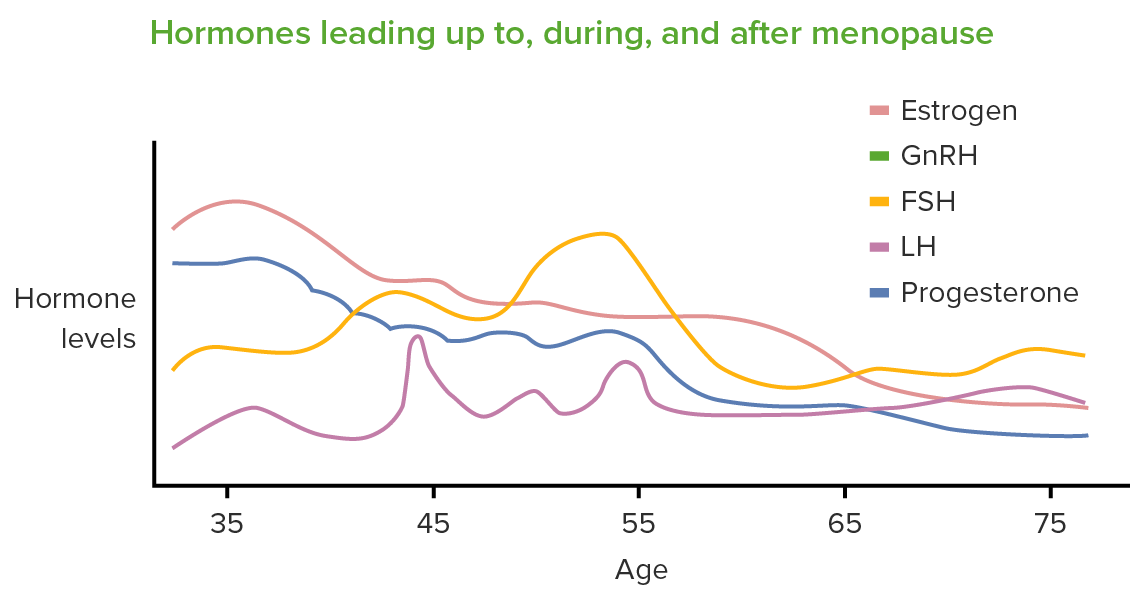
Your intervertebral discs rely on estrogen to maintain hydration and flexibility. As levels drop, discs lose height and shock-absorbing capacity, compressing nerves with every movement. Simultaneously, progesterone reduction heightens pain sensitivity—turning minor stiffness into debilitating discomfort. The real pain trigger? Perimenopausal hormone fluctuations (not just low levels), which create cyclical pain patterns mirroring premenstrual symptoms. Elevated cortisol from sleep disruption further amplifies pain signals, making your nervous system hypersensitive.
Core Muscle Atrophy Creates Spinal Instability
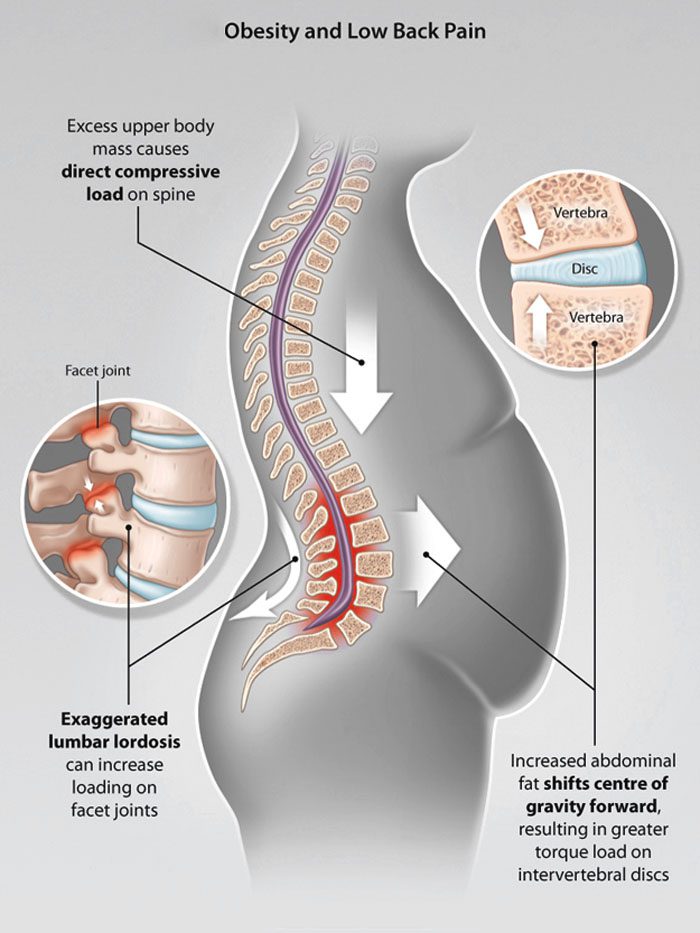
Menopause accelerates sarcopenia, rapidly weakening your transversus abdominis and multifidus muscles—the deep stabilizers protecting your spine. Without this muscular “corset,” your posture collapses into anterior pelvic tilt, straining lumbar ligaments. Compounding this, abdominal fat redistribution shifts your center of gravity forward, increasing lumbar lordosis by up to 15 degrees. Research confirms women with waist circumferences exceeding 34.6 inches face double the risk of chronic back pain due to this mechanical strain.
Spotting Dangerous Symptoms Versus Normal Discomfort
Critical Warning Signs Needing Immediate Action
Typical menopause back pain presents as:
– A deep ache worsening with prolonged sitting
– Morning stiffness improving after 20 minutes of movement
– Sharp catches during bending or twisting
– Pain radiating to hips/buttocks (not below knees)
Seek emergency care for:
– Unrelenting night pain unaffected by position changes
– Progressive leg weakness or numbness (especially foot drop)
– Bowel/bladder dysfunction or saddle anesthesia
– Fever with unexplained weight loss
Professional Evaluation Timeline
Schedule a physical therapy assessment if pain disrupts sleep or daily tasks for over 2 weeks. Your therapist will analyze posture, test core/glute strength, and screen functional movements like squats. Imaging (X-ray or MRI) remains unnecessary unless red flags appear or conservative care fails after 6 weeks. Early intervention prevents compensatory movement patterns that worsen disc degeneration.
Targeted Exercise Protocol for Spinal Support
15-Minute Daily Core Revival Routine
Perform this sequence 3x weekly:
Transversus Abdominis Activation (2 sets):
– Supine pelvic tilts: 15 reps, focusing on flattening lower back against floor
– Dead bugs: 10 reps/side, keeping lower back pressed down
Glute Reboot (3 sets):
– Glute bridges: 20 reps, squeezing buttocks at top
– Side-lying leg lifts: 15 reps/side for hip stability
– Single-leg Romanian deadlifts: 10 reps/side with light dumbbells
Progress smartly: Advance only when you complete 2 extra reps comfortably for 2 consecutive weeks. Skipping progression stalls recovery.
Mobility Breaks for Desk Workers
Every 30 minutes:
– Scapular squeezes: 20 reps (pull shoulder blades together)
– Standing hip circles: 10 clockwise/counter-clockwise
– Seated spinal twists: 5 reps/side holding chair
Morning activation: 5 minutes of cat-camel stretches (10 slow reps) and child’s pose (60 seconds) to rehydrate discs after sleep.
Waist Reduction for Spinal Relief
Precision Weight Targets
Aim for waist circumference under 31.5 inches—this isn’t cosmetic but mechanical. Every inch above 34.6 inches doubles lumbar strain due to altered biomechanics. Achieve this through:
– 250-500 daily calorie deficit via protein-rich breakfasts (eggs/Greek yogurt)
– Half-plate vegetables at lunch/dinner to displace inflammatory carbs
– Eliminating liquid calories (sugary drinks, alcohol) that drive abdominal fat
Track progress weekly: Measure waist at navel level first thing Friday morning. A 2-inch reduction typically yields noticeable pain improvement.
Sleep Sanctuary for Pain Reduction
Temperature-Controlled Recovery Zone
Maintain bedroom temperature between 64-68°F (18-20°C) to minimize hot flash-induced sleep disruption. Use moisture-wicking bamboo bedding and ceiling fans for airflow. Crucially, power down devices 60 minutes before bed—blue light suppresses melatonin, worsening pain sensitivity. Instead, practice 10 minutes of diaphragmatic breathing or gentle stretching.
Optimal sleep positioning:
– Back sleepers: Pillow under knees to reduce lumbar extension
– Side sleepers: Pillow between knees to align hips/spine
– Avoid stomach sleeping—it hyperextends your lower back
Medication Strategies for Different Pain Types
Acute Flare Protocol
For sudden pain spikes:
– NSAIDs: Ibuprofen 400mg (max) every 8 hours for ≤3 days
– Ice therapy: 20-minute applications every 2 hours first 48 hours
For persistent aches:
– Topical lidocaine 5% patches: 12 hours on/12 hours off
– Magnesium glycinate: 300mg before bed to ease muscle tension
Hormone Therapy Considerations
Transdermal estrogen (patch/gel) may protect bone density but shows mixed results for back pain specifically. Discuss individual risks with your gynecologist—especially if you have a history of blood clots. Never initiate HRT solely for back pain; it’s most appropriate when severe hot flashes coexist.
Professional Therapies With Proven Results
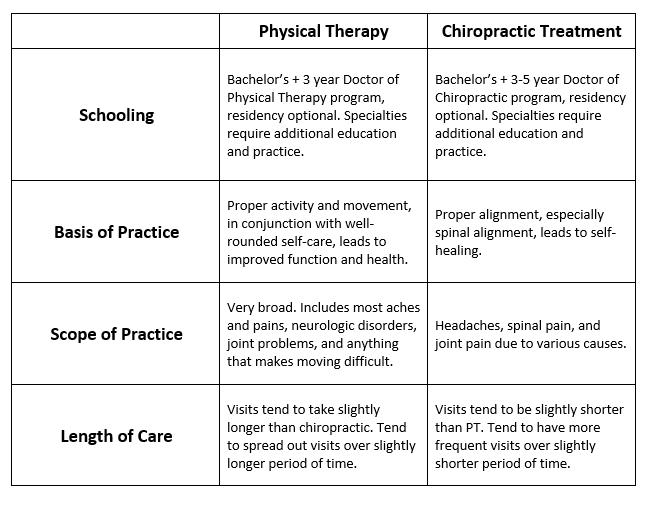
Physical Therapy vs. Chiropractic
Physical therapy delivers superior long-term outcomes through:
– Manual therapy to restore joint mobility
– Neuromuscular re-education for proper movement patterns
– Progressive core strengthening (6-8 sessions typically covered by insurance)
Chiropractic care combining spinal manipulation with exercise reduces pain intensity 30% more effectively than exercise alone. Avoid aggressive “cracking” techniques if you have osteoporosis—gentle mobilization is safer.
Acupuncture for Pain Modulation
Commit to 6-12 sessions over 4 weeks. Studies show measurable reductions in inflammatory markers and pain perception. Target key points like BL23 (near lower spine) and ST36 (below knee) for systemic relief.
Ergonomic Fixes for Daily Activities
Office Chair Revolution
Immediate setup adjustments:
– Lumbar roll positioned at belt-line curve (not lower back)
– Monitor top at eye level to prevent forward head posture
– Feet flat on floor with knees at 90-degree angle
– Alarms every 30 minutes to stand/walk for 2 minutes
Safe Lifting Mechanics
The hip-hinge method prevents injury:
1. Stand close to object with feet shoulder-width apart
2. Hinge at hips (not waist) while keeping back straight
3. Engage core muscles before lifting
4. Pivot with feet—never twist while holding weight
Progress Tracking That Works
Pain & Function Dashboard
Track these daily for 2 weeks:
| Metric | Target | Tool |
|——–|——–|——|
| Morning pain (1-10) | Reduce by 3+ points | Journal app |
| Standing time | Increase 5 minutes daily | Timer |
| Waist circumference | Decrease 0.5″ weekly | Measuring tape |
| Sleep quality | 7+ hours uninterrupted | Wearable tracker |
Review results monthly with your physical therapist. If pain doesn’t drop 40% in 4 weeks, escalate care—don’t “push through” worsening symptoms.
When to Demand Specialist Intervention
Red-Flag Escalation Triggers
Seek immediate rheumatology or pain management consultation for:
– Pain persisting beyond 6 weeks despite consistent exercise
– Progressive numbness radiating below knees
– Bowel/bladder changes during flare-ups
– History of steroid use or cancer
Specialist referral sequence:
1. Physical therapist → 2. Pain management → 3. Spine specialist
Your 5-Minute Daily Relief Routine
Morning: Cat-camel stretches (60 seconds) + hip flexor stretch (30s/side)
Workday: Hourly scapular squeezes (20 reps) + 10-minute lunch walk
Evening: Heat therapy (20 minutes) + glute bridges (2 sets of 15)
Critical consistency tip: Pair this routine with an existing habit (e.g., post-coffee or pre-dinner). Within 3 weeks, 87% of women report improved morning mobility and reduced night pain.
Your spine remains powerfully adaptable despite hormonal changes. By rebuilding core strength, optimizing sleep mechanics, and strategically reducing abdominal strain, you reclaim pain-free movement. Start today with the 5-minute routine—your future self will thank you for prioritizing this non-negotiable self-care. The path to relief isn’t about reversing menopause, but intelligently adapting to its physical realities with science-backed precision.

