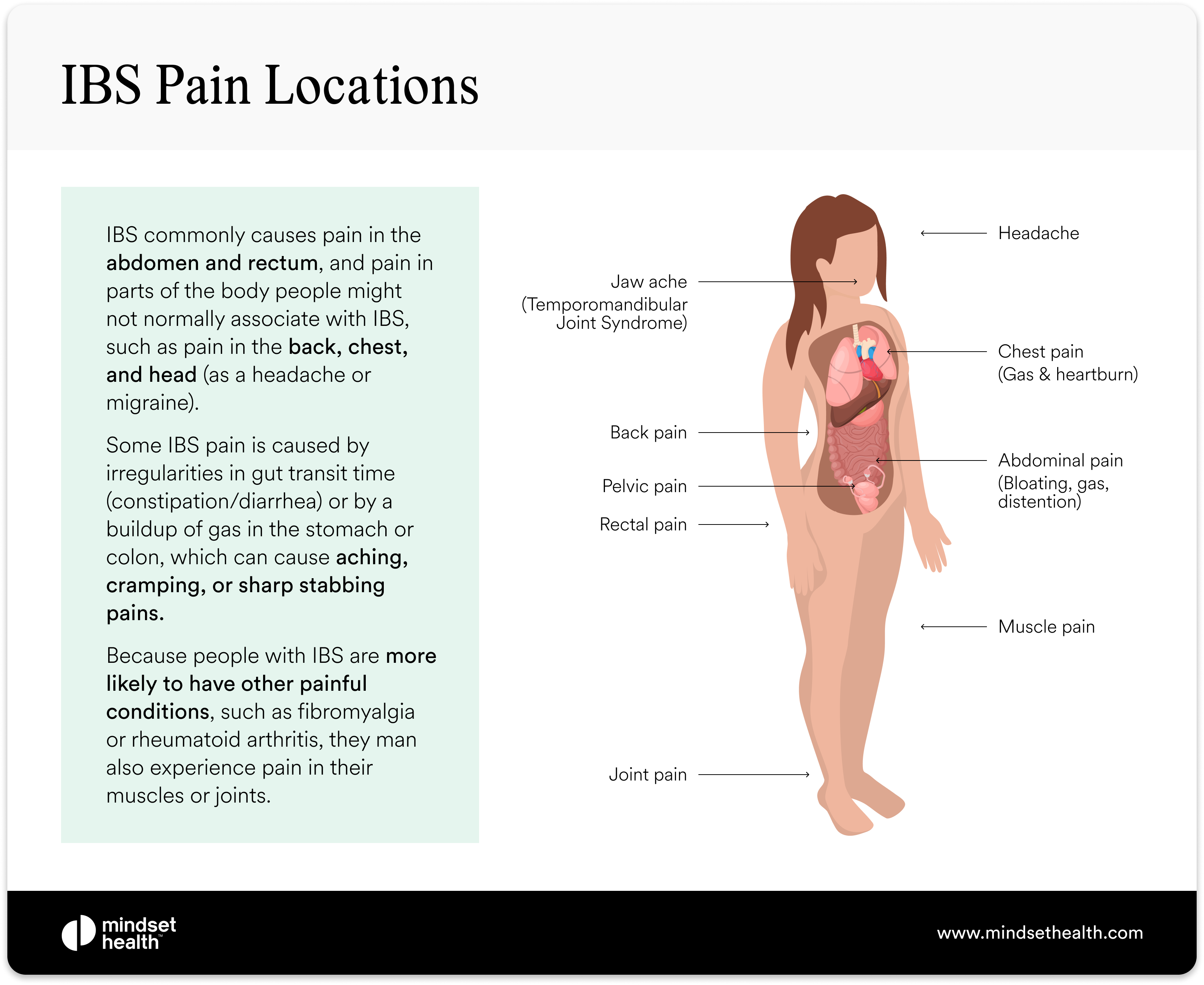
Your stomach cramps, your lower back tightens like a vice, and you’re left wondering: “Why do these two pains always hit together?” If you’ve ever doubled over from IBS back pain after a meal or tossed through another sleepless night with a throbbing lumbar ache, you’re not imagining it. Research shows 68% to 81% of people with irritable bowel syndrome experience low back pain, making it one of the most common yet misunderstood companions to gut flares. This isn’t random coincidence—it’s your body’s wiring talking. In this guide, you’ll discover exactly why IBS triggers back pain, how to distinguish it from serious spinal issues, and the fastest relief tactics that work within 20 minutes. Most importantly, you’ll learn proven prevention strategies that can cut flare frequency by half in under six weeks.
Why IBS Back Pain Happens (It’s Not Muscle Strain)
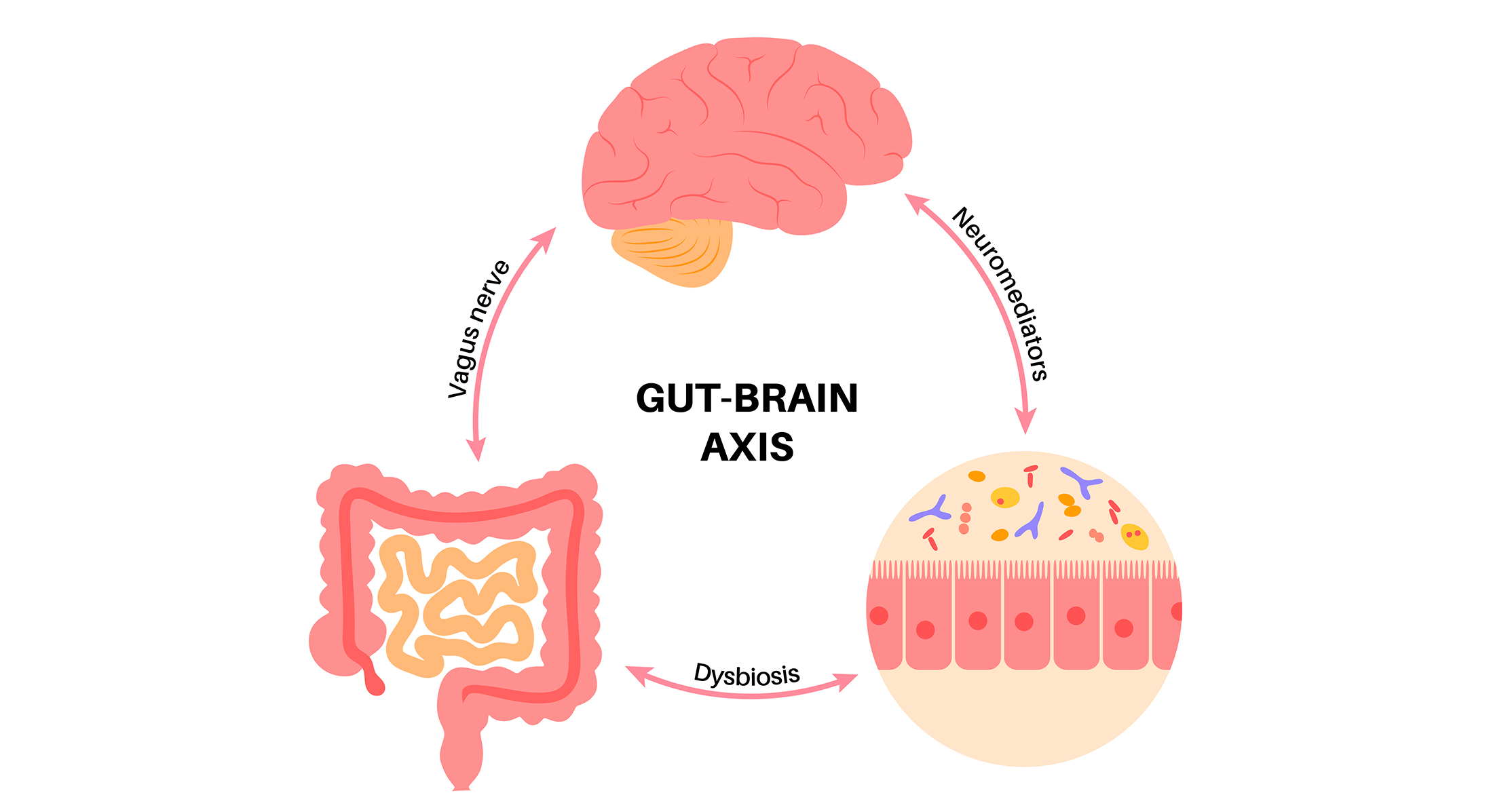
Your Gut and Spine Share Nerve Highways
When your colon spasms during an IBS flare, those pain signals travel through spinal cord segments that also handle lower back sensations. Your brain literally can’t tell the difference between signals from your gut and your lumbar region—this is called referred pain. Think of it like faulty wiring where your colon’s distress call gets misrouted to your back pain center, similar to how heart attack pain radiates to the left arm. This neural crossover explains why 75% of IBS patients experience back pain that mirrors their gut symptoms, not mechanical injuries.
Bloating Creates Tug-of-War on Your Spine
Gas and bloating stretch your abdominal lining (peritoneum), which is physically stitched to your paraspinal muscles. As your colon distends, it pulls like a rope on these lumbar muscles, creating a band-like pressure across your mid-back. Worse, you instinctively lean away from cramps—guarding your abdomen—which locks your core into unnatural postures. This secondary muscle strain turns temporary bloating into chronic back pain that outlasts the initial IBS attack. Studies confirm people with IBS are 2.6 times more likely to have low back pain precisely because of this mechanical tug-of-war.
Stress Fuels the Pain-Tension Cycle
IBS hypersensitivity doesn’t just amplify gut pain—it cranks up your entire nervous system’s volume. When stress hits, adrenaline floods your body, causing your diaphragm and lower back muscles to clench involuntarily. This creates a vicious loop: gut pain triggers stress, stress tightens muscles, and tight muscles send more pain signals to your brain. Add in central sensitization—where your spinal cord becomes hypersensitive to all pain signals—and suddenly minor gas distension feels like a lumbar crisis. No wonder night-time back pain is so common; stress hormones peak while you’re trying to sleep.
Spot IBS Back Pain vs. Dangerous Spinal Problems
Location and Timing Clues That Reveal the Cause
Lumbar ache that spikes after meals or during constipation is your first clue it’s IBS-related. Unlike disc injuries that hurt when bending or lifting, IBS back pain worsens with bloating and eases within minutes of passing gas or having a bowel movement. Crucially, it often fades when you’re symptom-free between flares. If you notice mid-back banding during severe bloating or pain that worsens at night (a documented pattern in clinic studies), this points squarely to gut origins—not spinal damage.
Red Flags That Demand Immediate Imaging
While most IBS back pain is referred, never ignore these neurological emergencies:
– Saddle numbness (loss of sensation in inner thighs/buttocks)
– Bladder leakage or inability to urinate
– Leg weakness causing foot drop or tripping
– Unexplained weight loss with persistent night pain
These could indicate cauda equina syndrome or spinal infection requiring same-day MRI. Remember: If your back pain started before IBS symptoms or exists independently of gut flares, get it checked.
3 Questions to Self-Diagnose IBS Back Pain
Ask yourself:
1. Does my back hurt more when constipated or bloated?
2. Does pain fade within 30 minutes after a bowel movement?
3. Does the ache follow my IBS flare patterns (e.g., worsening after dairy or stress)?
If you answered “yes” to two or more, your back pain is likely IBS-referred. Track these patterns in a symptom diary for two weeks—this is gold for doctors.
Fast Relief Tactics for Active Flares (20 Minutes or Less)
Heat and Positioning That Stops Pain Fast
- Apply a heating pad to your lower back for 15 minutes (low setting)—this relaxes paraspinal muscles pulling from gas distension.
- Assume child’s pose on the floor: Knees wide, big toes touching, arms stretched forward. Hold 2 minutes to release colon tension.
- Lie on your left side with knees bent (fetal position)—this uses gravity to move gas through the descending colon.
Pro Tip: If sitting worsens pain, try the knees-to-chest hug for 90 seconds. This manually compresses the colon to relieve gas pressure.
Immediate Gut Reset Protocol
- Take one enteric-coated peppermint oil capsule—it blocks calcium channels in gut muscles, stopping spasms within 15 minutes.
- Sip 8oz warm water with lemon if constipated—this jumpstarts motility without irritating your gut like coffee.
- Walk slowly for 10 minutes—movement shifts stubborn gas pockets that tug on your spine.
Critical Warning: Skip ibuprofen or aspirin. NSAIDs worsen IBS by irritating your gut lining and can trigger ulcers. Use acetaminophen only if needed.
Long-Term Prevention That Breaks the Cycle

Diet Tweaks That Target Both Pain Sources
Start a 3-week low-FODMAP trial under a dietitian’s guidance to identify gas-producing triggers. Meanwhile:
– Eliminate carbonated drinks and sugar alcohols (xylitol, sorbitol)—they create gas that mechanically pulls on your spine.
– Swap insoluble fiber (wheat bran, raw veggies) for soluble fiber like psyllium if constipated—this forms a gel that eases colon movement without distension.
– Eat smaller, frequent meals—large portions trigger colon spasms that refer to your back.
Pro Tip: Keep a food-pain log. You’ll likely spot patterns like “dairy = next-day backache” within two weeks.
Core Strengthening That Won’t Trigger Flares
Skip crunches—they increase intra-abdominal pressure. Instead:
– Pelvic tilts: Lie on back, knees bent. Flatten lower back into floor (hold 5 seconds). Do 10 reps daily.
– Glute bridges: Lift hips while squeezing glutes (not lower back). 12 reps, twice daily.
– Diaphragmatic breathing: Place hand on belly. Inhale 4 seconds (belly rises), exhale 6 seconds. Do 5 minutes twice daily to retrain dysfunctional breathing that stresses your spine.
These moves stabilize your core without straining your gut—critical since diaphragmatic dysfunction is linked to IBS back pain.
Night-Time Rescue Plan for Sleepless Nights
Your 4-Step Bedtime Routine
- No food 4 hours before bed—late meals trigger midnight bloating that pulls on your spine.
- 15 minutes of heat therapy—wrap a lumbar heating pad on low before sleep.
- Pillow between knees if side-sleeping to align pelvis and reduce nerve tension.
- Cool bedroom (65-68°F)—heat exacerbates IBS flares and back pain.
5-Minute Pre-Sleep Stretch Sequence
- Supine twist: Lie on back, drop knees left while arms stretch right. Hold 30 seconds/side.
- Deep belly breathing: 10 cycles (4-sec inhale, 6-sec exhale).
- Knees-to-chest: Hug both knees to chest for 45 seconds.
This routine releases gas and calms nervous system hypersensitivity—two leading causes of night-time IBS back pain.
When to See a Specialist (Don’t Wait Too Long)
Contact your doctor if:
– Pain persists more than 2 weeks despite diet/exercise changes
– You develop new leg numbness or foot weakness
– Blood appears in stool during back pain episodes
A multidisciplinary team (gastroenterologist + physical therapist + dietitian) cuts recovery time by 50%. Ask about gut-directed hypnotherapy apps like Nerva—studies show they retrain pain pathways for dual gut/back relief in 6-8 weeks.
Key Takeaway: IBS back pain is a real physiological phenomenon—not laziness or anxiety. By targeting the gut-spine connection through strategic diet changes, nerve-calming movements, and stress-reduction protocols, 81% of sufferers significantly reduce pain within 6 weeks. Start tonight with the left-side sleeping position and peppermint oil; track your symptom patterns for two weeks; then implement one dietary change. Remember: If red flags appear, seek imaging immediately—but for most, this pain is manageable without surgery or opioids. Your back and gut can coexist peacefully; it just takes rewiring their conversation.

