That sharp, burning sensation wrapping around your left chest and back has you worried—rightfully so. When pain strikes simultaneously in these areas, your mind races to the worst possible scenarios. Is it your heart? Something less dangerous? Left chest pain and back discomfort together create one of medicine’s most challenging diagnostic puzzles because the symptoms overlap between life-threatening cardiac events and less serious conditions. This guide walks you through the critical differences, helping you understand when to call 911 versus scheduling a routine checkup—potentially saving your life in the process.
Left chest pain and back symptoms affect millions of Americans each year, yet few understand how to distinguish between harmless heartburn and a heart attack in progress. The reality is that cardiac-related discomfort often radiates to the back, creating confusion about the true source. By learning the specific patterns each condition follows, you’ll gain the knowledge to make informed decisions when pain strikes. Let’s explore what your body is trying to tell you through these specific pain patterns.
Spot the Cardiac Pain Pattern: Exertion and Relief Cycle

Heart-related discomfort follows a predictable rhythm that sets it apart from other causes. When your left chest pain and back discomfort consistently appears during physical activity—like climbing stairs or rushing to catch a bus—and mysteriously vanishes after resting for 5-10 minutes, your heart is sending an urgent warning signal. This exertion-rest cycle occurs because narrowed coronary arteries can’t supply enough blood to meet your heart’s increased demands during activity.
Don’t mistake this pattern for simple indigestion. Unlike gastrointestinal issues, cardiac pain doesn’t change with body position or deep breathing. The discomfort typically feels like pressure, squeezing, or fullness rather than sharp stabbing pain. Many heart attack survivors report initially dismissing their symptoms as “just gas” because they didn’t expect heart pain to manifest in their back.
How Cardiac Pain Differs from Esophageal Pain
- Cardiac: Starts predictably with exertion, stops with rest, unaffected by antacids
- GERD: Worsens after meals or when lying down, improves with antacids
- Esophageal spasms: Sudden severe squeezing, sometimes triggered by specific foods
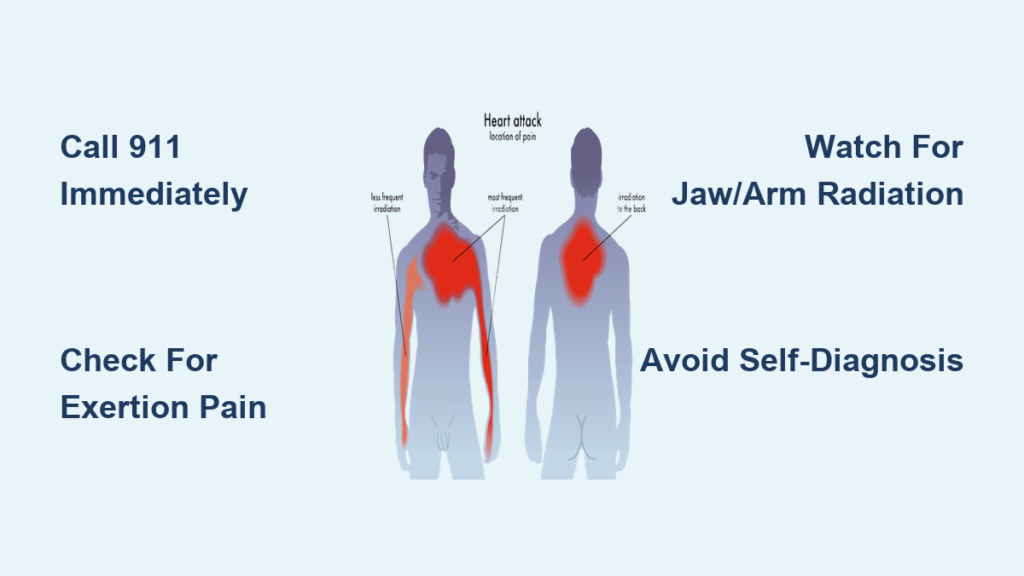
Recognize Heart Attack Danger Signs That Demand 911

Left chest pain coupled with back discomfort becomes critically dangerous when accompanied by specific warning signs. If you experience chest pressure spreading to your jaw, left arm, or between your shoulder blades—especially when combined with shortness of breath—you’re facing a potential cardiac emergency. These symptoms indicate your heart muscle may be starving for oxygen right now.
Never dismiss these combinations, even if the pain seems mild:
– Left chest pain with sudden cold sweats or nausea
– Back pain that arrives with unexplained fatigue
– Discomfort that wakes you from sleep
– Pain that intensifies over several minutes
Doctors prioritize cardiac evaluation because heart disease kills quickly—every minute counts during a heart attack. The diagnostic sequence begins with immediate electrocardiogram (ECG) and cardiac enzyme tests, not antacids or lifestyle advice. This protocol exists because heart disease remains the most dangerous possibility when left chest pain and back discomfort overlap.
Decode GERD’s Burning Pain Pattern

Gastroesophageal reflux disease (GERD) creates a burning sensation that climbs upward toward your neck and throat—often mistaken for cardiac pain. This heartburn originates when stomach acid splashes into your esophagus, causing inflammation that mimics heart attack symptoms. The pain typically centers under your breastbone but can radiate to your back, creating confusion about its source.
Look for these GERD-specific indicators:
– Burning pain that worsens when bending over or lying flat
– Symptoms appearing 1-3 hours after meals
– Relief from over-the-counter antacids within 30 minutes
– No connection between pain and physical activity
Heartburn affects over 60 million Americans monthly, making it the most common digestive symptom in the United States. However, its frequency doesn’t reduce its potential to mimic cardiac emergencies—especially when left chest pain and back discomfort occur together.
Identify Esophageal Emergencies Requiring Immediate Care
Esophageal rupture presents with dramatic symptoms—sudden, severe left chest pain and back pain following intense vomiting or medical procedures involving your esophagus. This rare but life-threatening condition requires immediate surgical intervention as stomach contents leak into your chest cavity. Unlike cardiac pain, esophageal rupture pain often worsens with swallowing and may be accompanied by fever.
Esophageal spasms create intense squeezing sensations that perfectly mimic heart attacks. These spasms can occur spontaneously or following meals, making differentiation challenging without medical testing. If your left chest pain and back discomfort happens only when swallowing or is triggered by very hot or cold beverages, esophageal issues become more likely.
Watch for esophageal-specific red flags:
– Pain that increases when swallowing liquids or solids
– Discomfort localized to the center of your chest (not left-sided)
– Symptoms that occur only after specific food triggers
– History of swallowing difficulties before the pain began
Navigate the Medical Testing Sequence Properly
When you report left chest pain and back discomfort to your doctor, expect a specific diagnostic sequence designed to rule out life-threatening conditions first. This protocol exists because heart disease kills quickly while esophageal disorders typically progress more slowly. The standard evaluation follows this critical order:
Emergency department protocol:
1. Immediate electrocardiogram (ECG) – Checks for heart rhythm abnormalities
2. Cardiac enzyme blood tests – Detects heart muscle damage
3. Chest x-ray – Evaluates heart size and lung conditions
4. Only after cardiac causes ruled out: Esophageal testing
This systematic approach protects you from missing dangerous cardiac conditions while efficiently identifying treatable esophageal disorders. Never skip steps in this sequence—doing so could mean missing a heart attack in progress.
When to Drive to ER vs. Schedule Appointment
Call 911 immediately if your left chest pain and back discomfort:
– Starts during physical activity and persists after resting 10 minutes
– Radiates to your jaw, left arm, or between shoulder blades
– Comes with sudden shortness of breath at rest
– Occurs with unexplained nausea or cold sweats
– Feels like “an elephant sitting on your chest”
Schedule same-day medical evaluation for:
– Recurring heartburn despite antacid use
– Pain that improves when sitting upright
– Discomfort triggered by specific foods
– Swallowing difficulties with chest pain
– Symptoms that don’t follow cardiac patterns
Remember: When in doubt, get checked out. Emergency departments would rather evaluate a false alarm than miss a heart attack in progress. Your symptoms deserve professional assessment—not internet diagnosis.
Avoid Dangerous Self-Treatment Mistakes
Never self-diagnose left chest pain and back discomfort. Assuming your symptoms are “just heartburn” could delay treatment for a heart attack in progress. Similarly, treating every episode with antacids when cardiac issues are present wastes critical treatment time. The overlap between cardiac and esophageal symptoms makes professional evaluation essential for your safety.
For patients with classic GERD symptoms without cardiac red flags, doctors may prescribe acid-blocking medications as a diagnostic trial. However, this approach only applies to very typical cases with no warning signs. If your left chest pain and back discomfort appears during exertion or wakes you from sleep, cardiac evaluation must come first.
Prevent Future Pain Episodes with Targeted Strategies
GERD prevention requires specific lifestyle adjustments:
– Elevate head of bed 6-8 inches using blocks (not just pillows)
– Wait 3 hours after eating before lying down
– Eliminate common triggers: coffee, alcohol, spicy foods, chocolate
– Maintain healthy weight to reduce abdominal pressure
– Quit smoking to strengthen your esophageal sphincter
Cardiac risk reduction demands consistent action:
– Follow prescribed exercise routines (always consult your doctor first)
– Adopt a Mediterranean-style diet rich in vegetables and healthy fats
– Monitor and manage blood pressure and cholesterol levels
– Practice stress-reduction techniques like deep breathing
– Attend all recommended cardiac checkups
Critical takeaway: Left chest pain extending to your back demands professional medical evaluation—no exceptions. While GERD and esophageal disorders cause similar symptoms, heart disease remains the most dangerous possibility when these areas hurt simultaneously. When pain strikes, err on the side of caution: emergency departments would rather evaluate a false alarm than miss a heart attack. Your symptoms deserve expert assessment, not internet diagnosis. Remember that cardiac pain often presents differently in women, with back pain being a more common symptom—don’t dismiss your discomfort based on stereotypes. If you experience left chest pain and back discomfort that concerns you, seek immediate medical attention. Your life could depend on it.