That persistent ache in your lower back has become more than just discomfort—it’s stealing your quality of life. You’ve tried everything: physical therapy sessions, over-the-counter pain relievers, even those steroid injections your doctor recommended. Yet the pain continues to disrupt your sleep, limit your activities, and make simple tasks like bending to tie your shoes feel impossible. If you’re considering low back pain surgery, you’re not alone—thousands of patients face this decision after conservative treatments fail to deliver lasting relief.
Most low back pain resolves naturally within three months through non-surgical approaches. However, for the small percentage of patients whose pain persists despite comprehensive conservative care, low back pain surgery may become a necessary consideration. Understanding when surgery transitions from last resort to logical next step empowers you to make informed decisions about your spinal health and long-term mobility.
Critical Warning Signs That Demand Surgical Consultation
Three Non-Negotiable Conditions for Surgery
Low back pain surgery only becomes appropriate when three specific conditions align simultaneously. First, your spine specialist must confirm the anatomical source of your pain through MRI or advanced imaging—this rules out cases where imaging shows abnormalities but no clear pain source. Second, you must have completed a thorough trial of conservative treatments including physical therapy, medications, and injections for several months without meaningful improvement. Third, your functional limitations must severely impact daily life—preventing you from working, caring for family members, or even sleeping through the night without pain medication.
Emergency Indicators Requiring Immediate Surgical Intervention
Certain symptoms signal neurological emergencies needing surgery within 24-48 hours. Foot drop, characterized by your inability to lift the front part of your foot while walking, indicates severe nerve compression requiring urgent attention. New bowel or bladder dysfunction—particularly loss of control—combined with saddle anesthesia (numbness in the genital area) suggests cauda equina syndrome, a medical emergency where delayed low back pain surgery can cause permanent damage. Progressive leg weakness that worsens daily also warrants immediate evaluation.
Measuring Functional Disability for Surgical Candidacy
Your daily function serves as the ultimate measure for determining surgical necessity. When pain prevents basic activities like lifting your child, grocery shopping, or sleeping more than two consecutive hours, surgery becomes increasingly likely. Surgeons evaluate whether your pain significantly limits essential life activities despite appropriate conservative care. If you find yourself canceling plans regularly or needing daily pain medication just to function, these are strong indicators that low back pain surgery deserves serious consideration.
Minimally Invasive Procedures That Target Specific Pain Sources
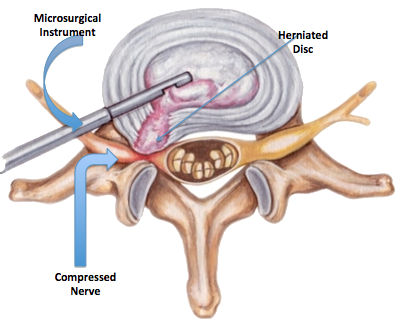
Decompression Surgeries for Nerve Pressure Relief
Microdiscectomy targets herniated discs pressing on nerves by removing only the damaged disc portion through a small incision. This outpatient procedure typically allows return to light activities within one week, with most patients experiencing immediate relief from radiating leg pain (sciatica). Laminectomy removes bone or tissue compressing nerves in spinal stenosis cases, now frequently performed as same-day surgery using minimally invasive techniques that reduce recovery time from weeks to days.
Spinal Fusion Options for Structural Instability
Lumbar fusion joins vertebrae to eliminate painful motion segments, most commonly addressing the L4-L5 area experiencing the greatest wear. The posterior approach accesses your spine through the back, while anterior lumbar interbody fusion (ALIF) approaches from the abdomen for potentially easier recovery. Lateral approaches offer alternatives for complex cases, with modern techniques using advanced implants and biologics to enhance healing. Ideal candidates include those with spondylolisthesis (vertebral slippage), spinal fractures, or significant degenerative changes.
Motion-Preserving Alternatives to Traditional Fusion
Artificial disc replacement offers an alternative for degenerative disc disease by maintaining spinal motion while replacing damaged discs. This approach potentially reduces stress on adjacent segments and typically allows shorter hospital stays than fusion. Posterior motion devices address spinal stenosis or mild spondylolisthesis while preserving natural movement through minimally invasive implants. For sacroiliac joint dysfunction, SI joint fusion provides targeted relief with same-day discharge options.
Essential Pre-Surgery Considerations Most Patients Overlook
Comprehensive Pre-Operative Evaluation Process
Before scheduling low back pain surgery, you’ll undergo thorough medical clearance including blood tests, imaging, and cardiac evaluation. Your surgeon should explain the specific procedure, expected outcomes, potential risks, and realistic recovery timeline in detail. Obtaining a second opinion from another spine specialist is strongly recommended—particularly since low back pain often requires multidisciplinary assessment to ensure surgery addresses the true pain source.
Mental Health’s Surprising Impact on Surgical Outcomes
Research consistently shows patients with positive mental outlooks experience better surgical results. Those who feel more in control of their health report higher satisfaction and faster recovery. Addressing anxiety, depression, or unrealistic expectations before low back pain surgery significantly improves outcomes—consider consulting a pain psychologist if you’re experiencing significant emotional distress related to chronic pain.
Lifestyle Factors That Make or Break Your Recovery
Your overall health dramatically affects surgical complexity and healing. Smoking cessation is critical—nicotine reduces blood flow to healing tissues, doubling complication risks. Diabetes management must be optimized before surgery, as uncontrolled blood sugar impairs healing. Weight management before surgery reduces strain on your healing spine and lowers complication risks. Committing to these lifestyle changes 6-8 weeks pre-surgery substantially improves your surgical outcome.
Realistic Recovery Expectations by Procedure Type
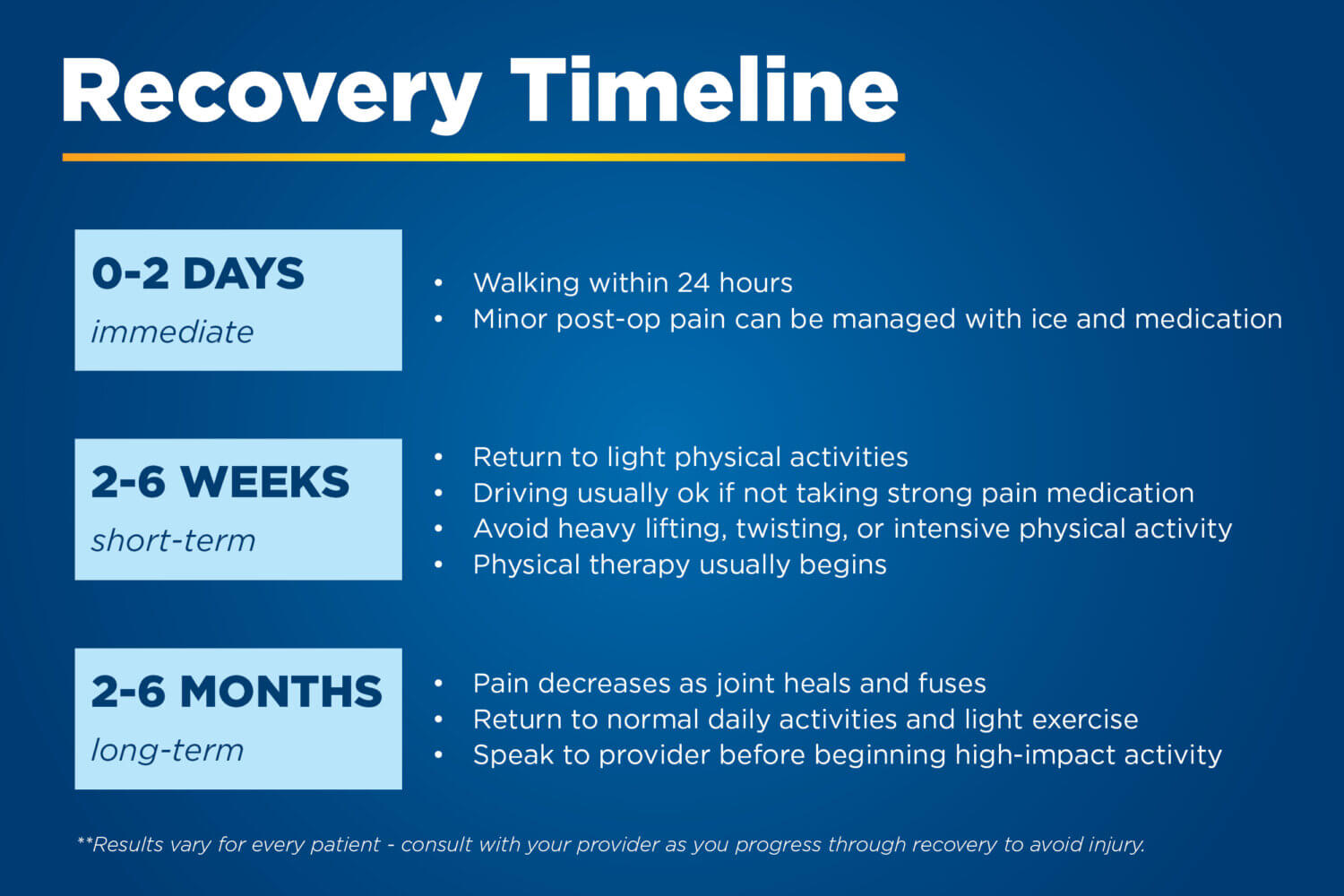
Procedure-Specific Healing Timelines
Microdiscectomy patients often return home the same day and resume light activities within one week, though full nerve healing may take months. Lumbar fusion requires overnight hospitalization with 3-12 months for complete bone healing, though most daily activities resume within 6-8 weeks. Artificial disc replacement typically allows faster return to normal activities than fusion, with many patients driving within 2 weeks and returning to desk jobs in 3-4 weeks.
Postoperative Care Protocol Checklist
Your recovery team will provide detailed instructions including:
– Pain management: Medication schedules with gradual tapering plans
– Activity modifications: Strict “no bending, lifting over 5 pounds, or twisting” rules for initial weeks
– Support devices: Proper use of back braces, shower stools, and supportive pillows
– Physical therapy: Progressive strengthening starting with walking and gentle stretching
– Lifestyle restrictions: No smoking, driving restrictions for 2-6 weeks, and gradual activity increases
Warning Signs Requiring Immediate Medical Attention
Monitor for complications needing urgent care: fever over 101°F, increasing incision pain, redness or swelling at surgical site, changes in bowel or bladder function, or new numbness in the genital area. These symptoms could indicate infection or neurological complications requiring prompt intervention to prevent permanent damage.
Critical Limitations of Low Back Pain Surgery You Must Understand
The Imaging-Pain Disconnect Problem
Even advanced MRI scans can’t always pinpoint pain sources—many people have bulging discs visible on imaging but experience no pain whatsoever. Conversely, some patients with severe pain show minimal imaging changes. This disconnect between imaging findings and symptoms complicates surgical decisions, which is why your functional limitations and specific symptoms matter more than imaging results alone.
Managing Realistic Pain Relief Expectations
Critical reality: Low back pain surgery relieves leg pain more effectively than back pain itself. Many patients continue experiencing some back discomfort even after successful procedures. Surgery addresses structural problems causing nerve compression, but doesn’t eliminate all pain sensations—particularly if pain has become chronic and centralized in your nervous system.
Bulging Disc Misconceptions That Lead to Unnecessary Surgery
Bulging discs represent normal age-related changes present in most adults over 30. Their appearance on imaging doesn’t automatically indicate surgical need—many require no treatment whatsoever. The presence of a bulging disc without corresponding neurological symptoms rarely justifies low back pain surgery. Don’t let imaging findings alone drive your surgical decision without thorough clinical correlation.
Modern Surgical Advances Revolutionizing Recovery
Minimally Invasive Techniques That Reduce Recovery Time
Contemporary low back pain surgery emphasizes smaller incisions, reduced operative time, and faster recovery through muscle-sparing approaches. Robotic assistance provides enhanced precision during complex procedures, while advanced biologics accelerate bone healing in fusion cases. These innovations have transformed many major spine surgeries from multi-day hospital stays to outpatient procedures.
Technology Integration Enhancing Surgical Outcomes
Navigation systems offer real-time guidance during surgery, improving accuracy and reducing complications. Intraoperative neuromonitoring detects potential nerve stress before damage occurs, enhancing safety. Motion-preserving technologies continue evolving as viable alternatives to traditional fusion, potentially reducing long-term complications while maintaining spinal function.
Key Takeaway: Low back pain surgery provides meaningful relief for carefully selected patients with confirmed structural problems and significant functional limitations. Success depends on realistic expectations, proper patient selection, and commitment to recovery protocols—not just the surgical procedure itself. Remember: the goal isn’t perfect pain elimination, but meaningful improvement in your ability to function and enjoy life. Work closely with your spine specialist to determine if surgery aligns with your specific condition, lifestyle, and recovery goals—only after exhausting conservative treatments and confirming your specific problem will benefit from surgical intervention.