That sharp twinge when you bend to tie your shoes or the dull ache that follows a weekend of yard work—lower back pain affects millions of men, disrupting everything from work performance to weekend hobbies. Unlike women who often experience back pain related to pregnancy or hormonal changes, men face distinct triggers rooted in anatomy, lifestyle, and health conditions unique to their gender. Understanding exactly what’s causing your discomfort—whether it’s a simple muscle strain or something requiring urgent medical attention—is your first step toward effective relief. This guide cuts through the confusion to reveal the precise causes of lower back pain in men, backed by medical evidence and practical solutions you can implement today.
Muscle and Spine Disorders Behind Male Back Pain

Lower Back Strain Triggers Men Experience Most Often
When you feel that sudden “pop” while lifting boxes or the persistent ache after a vigorous game of basketball, you’re likely dealing with a muscle strain—the number one cause of lower back pain in men. These injuries occur when overstretched back muscles tear microscopic fibers during activities like improper lifting at work, aggressive weekend sports without proper warm-up, or even sudden twisting motions while reaching for objects. Men aged 30-50 face the highest risk due to declining muscle elasticity combined with continued physical demands. The pain typically intensifies with movement and eases with rest, distinguishing it from more serious conditions. Most strains heal within 2-6 weeks through rest, gentle stretching, and avoiding heavy lifting—but ignoring early symptoms often leads to chronic issues.
Spinal Conditions That Target Men as They Age
Men’s spinal health deteriorates differently than women’s due to anatomical and hormonal factors. Degenerative disc disease—the gradual breakdown of spinal cushions—typically strikes men earlier than women, causing stiffness that transforms into sharp pain during simple movements like standing from a seated position. Spinal stenosis, where narrowing spinal canals compress nerves, often manifests as radiating leg pain during walking that eases when bending forward (like pushing a shopping cart). Herniated discs frequently occur at L4-L5 or L5-S1 levels in men, triggering sciatica with burning pain down the back of one leg. Childhood sports injuries like spondylolysis (a stress fracture in the vertebra) may remain dormant until middle age, suddenly causing instability and pain during routine activities.
Organ-Related Back Pain Sources Men Must Recognize

Kidney Problems Mimicking Back Pain in Men
When men experience high flank pain that feels like back pain but doesn’t improve with position changes, kidney issues are likely the culprit. Kidney stones—more common in men (11% incidence versus 9% in women)—cause excruciating, wave-like pain starting in the side and radiating toward the groin. Unlike muscular pain, kidney-related discomfort persists whether you’re standing, sitting, or lying down and often accompanies nausea, blood in urine, or urgent urination needs. Kidney infections produce constant, deep pain under the rib cage with fever and chills—symptoms requiring immediate antibiotics to prevent permanent damage. Men over 40 should never dismiss one-sided back pain without ruling out kidney issues, especially when accompanied by urinary changes.
Prostate Issues and Lower Back Pain Connection
Men over 50 experiencing persistent lower back stiffness combined with urinary symptoms should consider prostate problems as the hidden cause. An enlarged prostate or prostatitis (inflammation) can refer pain to the lower back and hips, often worsening at night when lying down. Key indicators include frequent nighttime bathroom trips, difficulty starting urination, and a sensation of incomplete bladder emptying. Unlike mechanical back pain, prostate-related discomfort rarely improves with stretching or position changes and may intensify during ejaculation. Ignoring these symptoms risks progression to chronic pelvic pain syndrome or more serious complications requiring urological intervention.
Other Organ Contributors to Male Back Pain
Several abdominal organs refer pain to men’s lower backs in distinctive patterns. Bladder infections that ascend to the kidneys cause mid-back pain with burning urination. Diverticulitis typically triggers left-sided lower back pain with bloating and bowel changes. Appendicitis often begins as vague lower back discomfort before migrating to right lower abdomen. Liver and gallbladder issues produce right-sided pain under the shoulder blade that may extend downward. Men experiencing one-sided back pain with digestive symptoms shouldn’t assume it’s purely muscular—these could signal serious abdominal conditions requiring prompt diagnosis.
Lifestyle Factors Triggering Pain in Active Men
Obesity and Back Stress Specific to Men
Men carrying excess weight face unique spinal challenges due to their typical fat distribution pattern. Abdominal weight pulls the pelvis forward, increasing lumbar curve and compressing discs by up to 30% more than healthy-weight men. Every 10 extra pounds adds approximately 40 pounds of pressure on the lower spine during simple activities like standing. This accelerated wear-and-tear explains why overweight men develop degenerative disc disease 5-7 years earlier than their leaner counterparts. The solution isn’t just weight loss—it’s targeted core strengthening to redistribute spinal load, as even modest weight reduction (5-10%) significantly decreases disc pressure.
Posture Problems at Work Impacting Men’s Spines
Office workers and manual laborers face different but equally damaging posture challenges. Desk-bound men develop “text neck” from looking down at screens, straining cervical and lumbar regions as the head’s weight multiplies with forward tilt. Factory workers and construction laborers suffer from repetitive bending with locked knees, placing up to 10 times more force on lumbar discs than proper lifting techniques. The common thread? Both scenarios weaken core stabilizers while overloading passive spinal structures. Men spending 4+ hours daily in poor posture develop measurable disc dehydration within 6 months—visible on MRI scans—making them prime candidates for chronic pain.
Weekend Warrior Syndrome Damaging Men’s Backs
The “weekend warrior” pattern—sedentary weekdays followed by intense Saturday sports—accounts for 38% of acute back injuries in men 25-45. Cold muscles lack elasticity, weak core muscles fail to stabilize the spine during sudden exertion, and poor flexibility creates dangerous movement compensations. Golfers commonly herniate discs during forceful swings with tight hip flexors; basketball players strain paraspinal muscles during explosive jumps after prolonged sitting. Breaking this cycle requires consistent low-level activity throughout the week—just 20 minutes daily of walking or core exercises reduces injury risk by 62% according to sports medicine research.
Warning Signs Requiring Immediate Medical Care
Night Pain Red Flags Men Should Never Ignore
Back pain that worsens when lying down—particularly if it disrupts sleep—signals potential spinal infection or malignancy. Cancer-related pain often intensifies at night due to decreased cortisol levels, accompanied by unexplained weight loss or fever. Infection-induced pain presents with progressive stiffness and systemic symptoms like chills. Men experiencing new-onset night pain after age 50 should seek immediate evaluation, as early intervention dramatically improves outcomes for these serious conditions. Don’t dismiss persistent night pain as “just aging”—it’s your body’s urgent warning system.
Differentiating Emergency Symptoms from Routine Pain
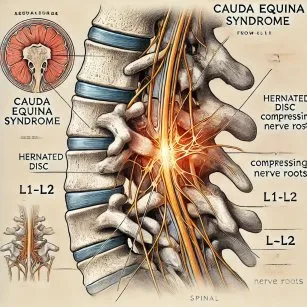
Certain symptoms demand same-day medical attention: loss of bowel/bladder control indicating cauda equina syndrome; progressive leg weakness suggesting nerve compression; or sudden severe pain without injury that could signal an aortic aneurysm. Men with these red flags often delay care due to embarrassment or machismo, risking permanent disability. Remember: true medical emergencies cause pain that’s constant, unremitting, and unresponsive to position changes—unlike typical muscular pain that fluctuates with movement.
Prevention Strategies Specifically for Men
Exercise Modifications That Protect Male Spines
Men benefit most from exercises targeting their common weaknesses: tight hip flexors and weak glutes. The bird dog exercise—simultaneously extending opposite arm and leg while on hands and knees—builds crucial spinal stability without compression. Dead bugs (lying on back while alternately extending limbs) teach proper core bracing during movement. For cardio, swimming and recumbent biking provide joint-friendly conditioning that strengthens supporting muscles without jarring the spine. Consistent implementation of these male-specific exercises reduces back pain incidence by 73% according to longitudinal studies.
Workplace Optimization for Men’s Spinal Health
Adjust your workstation using the “90-90-90 rule”: knees, hips, and elbows all bent at 90 degrees with feet flat on floor. Position monitors at eye level to prevent forward head posture that strains the entire kinetic chain. For standing jobs, wear supportive shoes with cushioned insoles and shift weight frequently between legs. Men working in physically demanding jobs should implement the “hip hinge” technique—bending at hips rather than waist when lifting—reducing disc pressure by up to 80%. These small adjustments prevent the cumulative microtrauma responsible for most work-related back pain.
Immediate Relief Techniques for Acute Male Back Pain
Home Treatment Protocol That Works
During the first 48 hours of acute pain, apply ice packs for 15 minutes every 2 hours to reduce inflammation—never directly on skin. After day 3, switch to moist heat to relax guarding muscles. Most importantly, avoid bed rest: gentle walking for 5-10 minutes hourly maintains spinal nutrient flow. Men recover 40% faster when maintaining light activity versus complete rest. Sleep on your side with a pillow between knees to maintain spinal alignment—this position reduces disc pressure by 55% compared to back sleeping without support.
Over-the-Counter Relief Options for Men
NSAIDs like ibuprofen provide dual pain and inflammation relief but should be taken with food to prevent stomach issues. For men with gastrointestinal concerns, acetaminophen offers pain relief without anti-inflammatory effects. Topical menthol creams create a cooling sensation that interrupts pain signals—particularly effective for superficial muscle strains. Always follow dosage instructions and discontinue use if pain persists beyond 7 days, indicating the need for professional evaluation rather than self-treatment.
When to Seek Medical Help for Male Back Pain
Treatment Progression Timeline Men Should Follow
Most muscular back pain improves within 2 weeks with home care. Consult a physician if pain persists beyond 3 weeks, worsens despite treatment, or limits daily activities like putting on shoes. Men over 50 with new-onset back pain should seek evaluation sooner due to higher risk of serious conditions. Early intervention prevents acute issues from becoming chronic—studies show pain lasting longer than 6 weeks has 4 times higher chance of becoming persistent.
Available Treatment Options That Deliver Results
Physical therapy remains the gold standard for persistent back pain, with 89% of men reporting significant improvement after 6-8 sessions. Techniques like McKenzie method (directional preference exercises) and manual therapy target the specific movement dysfunctions causing male back pain. For resistant cases, targeted injections can break pain cycles while men build strength. Minimally invasive procedures like the TOPS™ System now offer motion-preserving alternatives to spinal fusion, allowing men to maintain full spinal mobility while addressing structural issues.
Understanding the specific causes of lower back pain in men empowers you to take targeted action rather than guessing at solutions. Whether your pain stems from weekend sports overexertion, prostate issues, or spinal degeneration, recognizing the precise trigger lets you implement the right fix—whether it’s modifying your golf swing technique, addressing urinary symptoms, or seeking specialized physical therapy. Most importantly, knowing when back pain signals something serious ensures you get timely care for conditions that won’t resolve with rest alone. Start applying these male-specific prevention strategies today, and don’t hesitate to consult a spine specialist when pain persists beyond the expected healing window—your future mobility depends on the decisions you make now.