Eight in ten adults will endure disabling lower back pain during their lifetime, with 20% trapped in chronic agony exceeding three months. When weeks of physical therapy, NSAIDs, and steroid injections no longer cut it, you face a critical decision: which lower back pain medical procedure actually fixes your specific pain source? This isn’t about generic “back pain solutions”—it’s about matching your MRI findings and failed treatments to precise interventions like the Intracept® procedure for vertebrogenic pain or MILD decompression for spinal stenosis. You’ll discover exactly which diagnostic tests insurers require, recovery timelines that impact your work schedule, and why 64% of patients with Modic changes achieve lasting relief from a 60-minute outpatient procedure.
Forget one-size-fits-all approaches. Your path depends entirely on pinpointing the pain generator—whether it’s a herniated disc compressing nerves, arthritic facet joints, or bone-marrow inflammation visible only on MRI. We cut through the confusion with evidence-based comparisons of every option, from radiofrequency ablation to spinal fusion, so you can demand the right lower back pain medical procedure instead of wasting months on treatments doomed to fail.
Why 577 Million People Now Seek Lower Back Pain Medical Procedures
Global lower back pain cases exploded from 377 million in 1990 to 577 million by 2017, with 16 million Americans unable to complete daily tasks due to chronic pain. This surge stems from aging populations, sedentary lifestyles, and critical gaps in early intervention. Crucially, 20% of acute cases evolve into chronic pain when conservative care isn’t tailored to the root cause—like missing Modic changes on MRI that indicate vertebrogenic pain. If your pain persists beyond six weeks despite physical therapy and medications, procedural intervention becomes medically necessary to prevent permanent disability.
MRI Must Confirm Modic Changes for Intracept Eligibility
Your spine specialist won’t approve the Intracept® procedure without clear MRI evidence of Modic type 1 or 2 changes—bone-marrow edema at vertebral endplates signaling nerve inflammation. Unlike standard X-rays or CT scans that only show bone structure, MRI is non-negotiable for diagnosing this specific pain generator. If your imaging report mentions “endplate signal abnormalities,” demand clarification; misdiagnosis leads to failed procedures.
Why Diagnostic Nerve Blocks Predict Procedure Success
Before permanent interventions, targeted nerve blocks act as your pain roadmap:
– Positive facet block → 75% chance radiofrequency ablation will work
– Relief from sacroiliac injection → confirms SI joint as target
– No improvement after epidural → rules out nerve root compression
Skip this step, and you risk irreversible procedures for the wrong pain source. Insurers now require documented block results before approving ablation or Intracept.
Skip This Step and Your Procedure Will Fail: The 6-Week Non-Operative Mandate
Medicare and private insurers universally require documented failure of six weeks of conservative care before approving any lower back pain medical procedure. This isn’t bureaucracy—it’s evidence-based protocol. Your treatment log must show:
- 4+ weeks of physical therapy focusing on core strengthening and McKenzie extensions
- Trials of 2+ NSAIDs (e.g., ibuprofen → prescription meloxicam)
- At least one epidural or facet injection with recorded outcomes
Why Muscle Relaxants Sabotage Long-Term Recovery
While short-term muscle relaxants (like cyclobenzaprine) ease acute spasms, prolonged use beyond two weeks weakens core stabilizers—delaying procedural readiness. Taper off under medical supervision to avoid rebound pain that disqualifies you from time-sensitive interventions like MILD decompression.
Intracept Procedure: How Radiofrequency Ablation Erases Vertebrogenic Pain
FDA-approved exclusively for vertebrogenic pain (ICD-10 code M54.5 added October 2021), the Intracept® procedure destroys inflamed basivertebral nerves inside vertebrae using precise 85°C radiofrequency energy. Unlike spinal fusion, it preserves motion and leaves future options open—critical for active patients under 60.
Your 60-Minute Procedure Timeline
- Conscious sedation + local anesthetic (no general anesthesia)
- Fluoroscopy-guided needle insertion through a 3mm incision
- 15-minute nerve ablation via curved cannula targeting the vertebral body
- Immediate discharge with only mild soreness at the site
Recovery reality: Return to desk work in 48 hours but avoid lifting >10 lbs for 7 days. Full pain relief peaks at 3 months as inflammation subsides—64% report >50% improvement at 1 year, with benefits lasting 6+ years in studies.
MILD Decompression: Fixing Spinal Stenosis Without Fusion
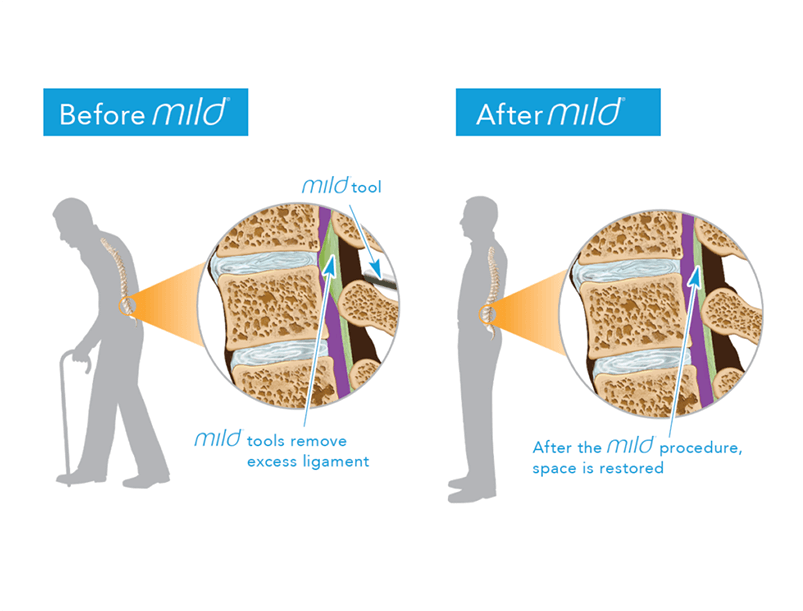
For stenosis caused by thickened ligamentum flavum, the MILD® procedure removes excess tissue through a 5mm incision—no implants, no fusion. Ideal for patients over 65 who can’t tolerate major surgery, it restores walking capacity in hours.
Why Standing Tolerance Jumps From 8 to 56 Minutes
By decompressing the spinal canal, MILD directly addresses neurogenic claudication:
– Day-of-procedure: Walk 50% farther without leg cramping
– Week 2: Begin physical therapy to rebuild endurance
– Month 3: 88% avoid further surgery at 5-year follow-up
Skip this if you have prior spine surgery at the same level—scar tissue blocks safe instrument access.
Microdiscectomy vs. Fusion: Choosing Your Surgical Lifeline
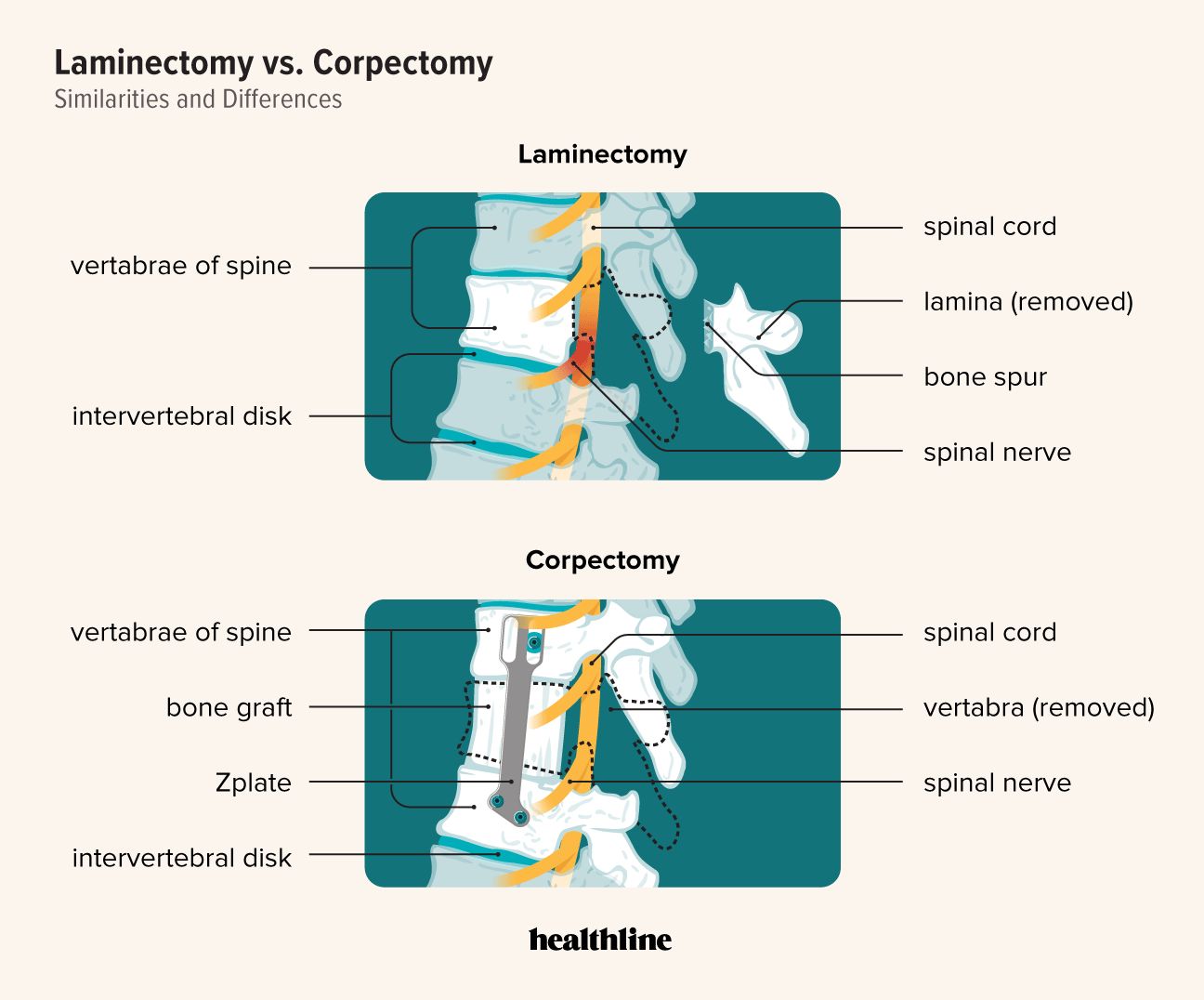
When herniated discs cause unremitting sciatica or “foot drop,” surgery becomes urgent. But choosing wrong risks failed back syndrome (20-40% of cases).
Critical Decision Points
- Microdiscectomy (2-6 week recovery): Only for contained disc fragments pressing one nerve root. Red flag: Don’t choose if MRI shows multilevel stenosis.
- Spinal fusion (3-6 month recovery): Reserved for spondylolisthesis or instability. Warning: 30% lose 50% spinal flexibility long-term.
- Artificial disc replacement (4-month recovery): Preserves motion but banned for osteoporosis or arthritis.
Never proceed without documented neurological deficits—insurers deny fusion for pure pain without objective findings.
Avoid These 3 Insurance Denial Traps for Lower Back Pain Procedures
70% of initial Intracept and MILD claims get denied despite Medicare coverage. Beat the system by:
- Including Modic change codes (M46.81, M54.5) in every claim—vague “low back pain” diagnoses get rejected
- Submitting physical therapy logs showing 6+ weeks of documented care
- Using ASC facility codes (not hospital outpatient) to slash costs by 40%
Appeal denials within 30 days with your specialist’s imaging report highlighting procedure-specific criteria.
Your 6-Week Roadmap From Procedure to Pain-Free Living
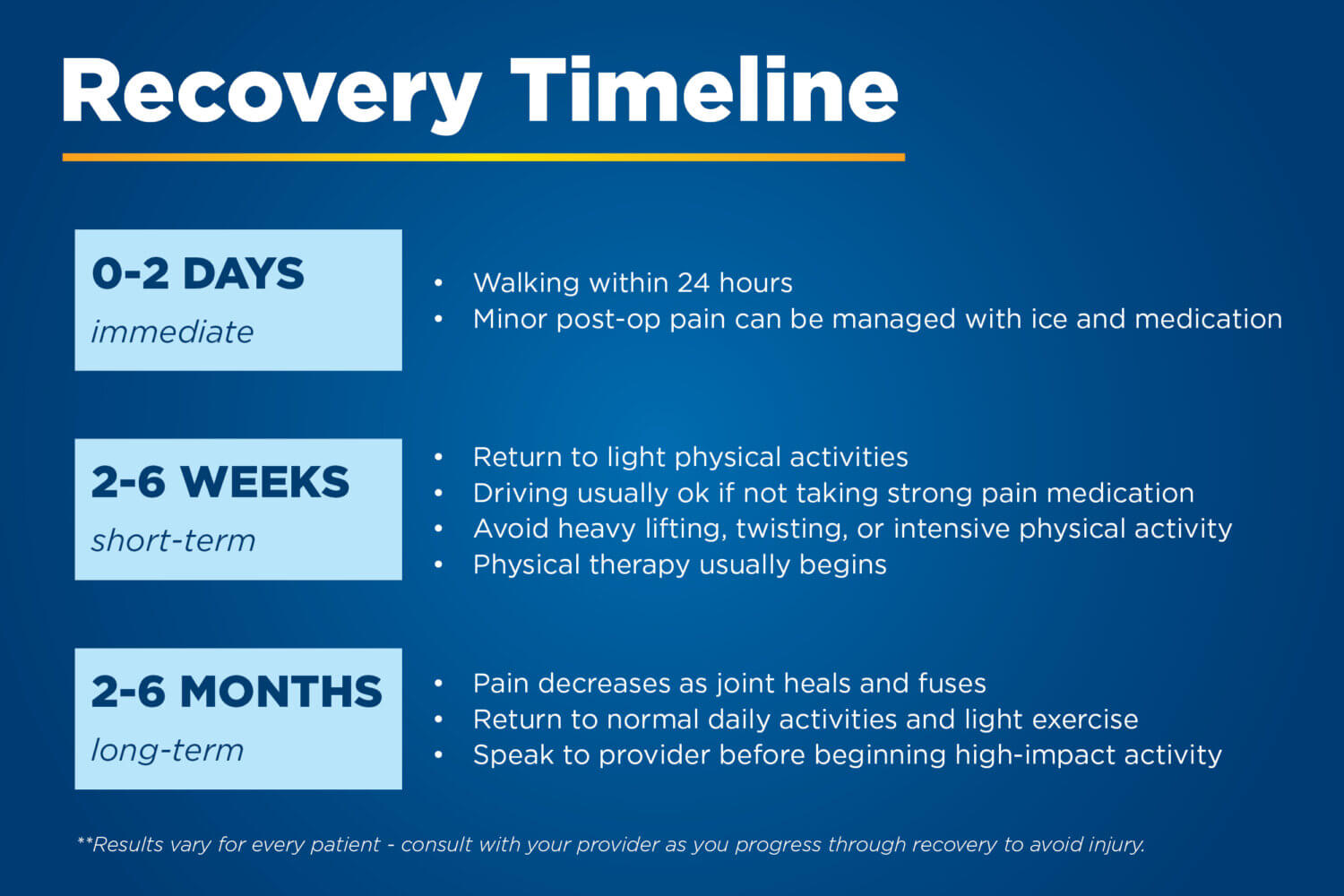
Skip structured rehab, and even successful procedures fail. Follow this timeline:
| Timeline | Critical Actions | Pitfalls to Avoid |
|---|---|---|
| Days 1-3 | Ice site 20 mins/hour; walk 5 mins hourly | Driving or bending >90° |
| Week 1 | Start PT with pelvic tilts; no lifting >5 lbs | Opioid overuse (triggers rebound pain) |
| Weeks 2-4 | Gradual extension exercises; monitor for infection | Returning to heavy labor too soon |
| Month 2+ | Sport-specific drills; lifelong core maintenance | Skipping maintenance PT (recurrence jumps 60%) |
Pro tip: Combine post-procedure PT with aquatic therapy—it cuts recovery time by 30% while protecting healing tissues.
Next-Gen Procedures to Demand in 2024: Intracept Gen 2 and Closed-Loop SCS
While biologics like stem cells remain unproven, two breakthroughs deliver now:
- Intracept Gen 2: Cuts procedure time to 30 minutes with dual-probe ablation—available at 200+ U.S. centers by Q3 2024.
- Closed-loop spinal cord stimulators: Auto-adjust settings when you stand/walk, eliminating manual programming.
Demand these if standard radiofrequency ablation failed you—the tech reduces repeat procedures by 50%.
Final Note: Vertebrogenic pain with Modic changes now has a targeted solution in Intracept, while MILD offers stenosis relief without fusion’s risks. Your success hinges on matching MRI findings to the exact procedure—skip diagnostic blocks or rush surgery, and failure is likely. Partner with a multidisciplinary spine center that combines imaging expertise, procedural precision, and rehab science. If your pain persists beyond six weeks of conservative care, armed with this roadmap, you’ll demand the right lower back pain medical procedure instead of settling for temporary fixes.