That persistent ache that migrates from your left flank to your right—then back again—can feel like a cruel game of spinal whack-a-mole. You’re not imagining it. Lower back pain that moves from side to side affects thousands of people, creating confusion about what’s really happening in your lumbar region. Unlike stationary back pain that stays put, this traveling discomfort often signals deeper biomechanical imbalances requiring specific interventions. Understanding why your pain shifts sides is the critical first step toward finding lasting relief.
This isn’t just random discomfort—shifting lower back pain follows predictable patterns based on your unique anatomy and movement habits. Most people waste months trying generic back pain remedies that fail because they don’t address the asymmetrical nature of this condition. The good news? With targeted strategies that match your specific pain pattern, you can break the cycle within weeks. Let’s explore exactly what’s happening when your lower back pain keeps changing sides and the evidence-based solutions that actually work.
Why Your Lower Back Pain Jumps Between Sides

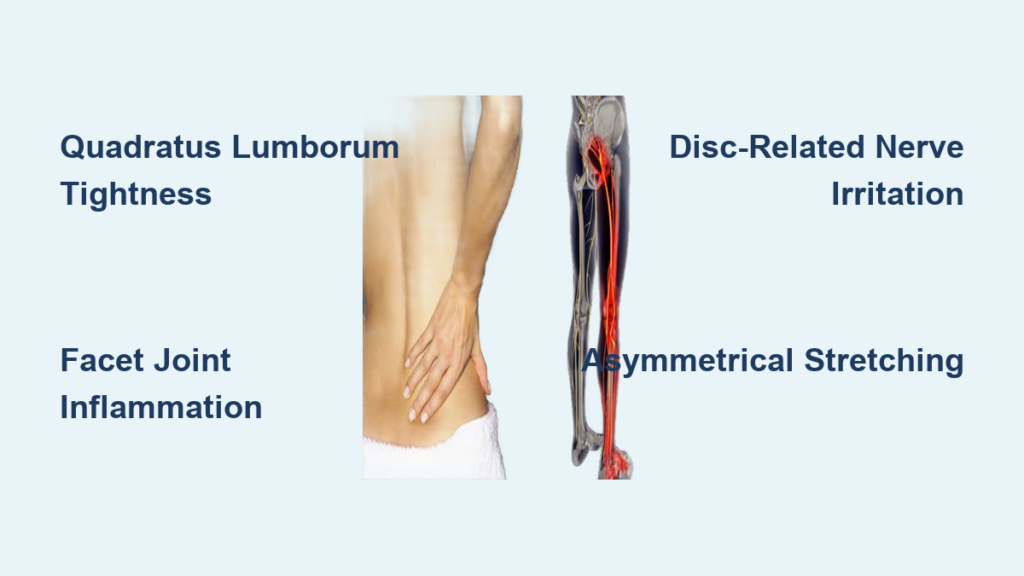
Quadratus Lumborum Trigger Points Creating Shifting Pain
Your quadratus lumborum—a deep muscle connecting your pelvis to ribs—acts like a puppeteer controlling spinal stability. When this muscle develops trigger points on alternating sides, it creates referral patterns that make pain appear to move. Asymmetrical sitting habits or favoring one leg while standing causes one side to tighten while the other weakens, creating a tug-of-war effect. The resulting pain often shifts sides as your body compensates for the imbalance during different activities. Morning stiffness on one side that switches to the other by afternoon typically indicates this muscular pattern.
Facet Joint Inflammation Patterns That Switch Sides
Your lumbar facet joints (those small hinges at the back of your spine) can become inflamed unevenly due to arthritis or repetitive stress. When the left L4-L5 joint flares up one week and the right L3-L4 joint becomes irritated the next, you experience true side-to-side migration of pain. Pain that worsens with backward bending but improves when leaning forward often signals facet joint involvement. This pattern commonly affects people who spend long hours at desks with poor posture, as the sustained spinal extension gradually irritates different joints.
Disc-Related Nerve Irritation That Alternates Sides
Bulging or degenerating discs don’t always stay centered. As disc material shifts or inflammation spreads, nerve irritation can jump between the left and right nerve roots exiting your spine. This creates a unique situation where bending forward might trigger left-sided pain one day, while twisting movements bring right-sided discomfort the next. Unlike muscular pain, disc-related shifting pain often radiates slightly into the buttocks and may intensify when sitting for prolonged periods.
Critical Warning Signs That Demand Medical Attention
Emergency Red Flags with Moving Back Pain
While most shifting lower back pain responds well to conservative treatment, certain symptoms require immediate evaluation:
- Progressive leg weakness that worsens daily
- Saddle numbness in the groin or inner thigh area
- Bowel or bladder changes combined with back pain
- Fever with severe night pain that disrupts sleep
These symptoms indicate potential nerve compression or infection requiring urgent medical intervention. Don’t wait—if you notice these signs, seek emergency care within 24 hours.
Movement Patterns That Reveal Your Specific Cause
Pay close attention to what triggers your pain shifts:
- Morning pain that eases with movement = inflammatory cause like facet joint arthritis
- Pain increasing throughout the day = muscular fatigue pattern
- Pain with specific movements like twisting = joint dysfunction
- Pain changing with position changes = disc involvement
Tracking these patterns in a simple journal helps identify effective treatments faster. Note which activities trigger shifts and how long symptoms last after each episode.
Immediate Home Relief Techniques That Target Shifting Pain
Precise Heat and Cold Application Protocol
Heat works best for muscle-related shifting pain:
– Apply moist heat (heating pad wrapped in damp towel) to the currently painful side
– Use for 15-20 minutes, 3-4 times daily during acute flares
– Focus on the area between your hip bone and spine
Cold therapy better addresses joint inflammation:
– Apply ice pack for 10 minutes to the most tender bony area
– Use a barrier like thin cloth to prevent skin damage
– Repeat every 2 hours as needed for sharp, localized pain
Targeted Asymmetrical Stretching Routine
Quadratus Lumborum Stretch for Current Pain Side:
– Stand with painful side near wall
– Raise arm overhead and lean away from wall
– Hold 30 seconds, repeat 3 times (do only on currently painful side)
Multifidus Activation Exercise:
– Lie on back, knees bent
– Gently draw belly button toward spine
– Hold 10 seconds without holding breath
– Perform 10 repetitions daily
Cat-Camel Mobilization:
– On hands and knees
– Slowly arch and round your back
– Focus on smooth, controlled motion
– 2 sets of 10 repetitions
Professional Treatments That Actually Resolve Shifting Pain

Physical Therapy Protocols That Address the Root Cause
Effective physical therapy for moving lower back pain targets asymmetrical weaknesses. Core stabilization exercises focusing on transverse abdominis and multifidus muscles show 60-80% success rates for resolving shifting pain patterns. Therapists use specific assessments to determine which side needs strengthening versus stretching.
Critical manual therapy techniques include:
– Joint mobilization for restricted spinal segments
– Soft tissue release for tight quadratus lumborum
– Nerve gliding exercises if radicular symptoms present
– Gait retraining to correct movement compensations
Precision Injection Approaches
Trigger point injections provide immediate relief for muscular causes. Using ultrasound guidance, clinicians inject small amounts of anesthetic into specific muscle knots on the currently painful side.
Diagnostic facet joint injections serve dual purposes:
– Confirming which joint is causing pain
– Delivering anti-inflammatory medication precisely
– Providing diagnostic information for long-term treatment planning
Daily Habits That Prevent Pain from Jumping Sides
Asymmetrical Ergonomic Adjustments
Workstation setup:
– Keep monitor directly in front of you to prevent twisting
– Use lumbar support that maintains natural spinal curve
– Alternate leg positions when standing at desks
– Set phone reminders to change positions every 30 minutes
Sleep positioning:
– Side sleeping: Use thick pillow between knees for alignment
– Back sleeping: Place small pillow under knees
– Avoid stomach sleeping—creates torque on lumbar spine
– Rotate pillow placement weekly to prevent favoring one side
Movement Break Strategies That Reset Your Spine
Implement micro-break protocol:
– Every 30 minutes: stand and shift weight side-to-side
– Every hour: walk 2 minutes with exaggerated heel-to-toe motion
– Every 2 hours: perform 5 minutes of gentle spinal twists
Walking technique that prevents shifting pain:
– Focus on even weight distribution between feet
– Engage core muscles lightly during movement
– Swing arms naturally to counterbalance spinal rotation
– Take conscious “reset steps” when pain begins shifting
Progressive Exercise Plan That Stops the Cycle
Foundation Building (Weeks 1-2)
Dead Bug Exercise:
– Lie on back, arms up, knees bent 90 degrees
– Slowly extend opposite arm and leg while maintaining core engagement
– Focus on keeping lower back pressed to floor
– 2 sets of 10 each side daily
Single-Leg Balance Training:
– Stand on one foot for 30 seconds
– Progress to eyes closed when stable
– Do 3 repetitions per side
– Perform daily to improve proprioception
Functional Strength (Weeks 3-4)
Side Plank Progression:
– Start on knees, progress to full side plank
– Ensure straight line from head to feet
– Hold 20-30 seconds each side
– Build to 3 sets daily
Hip Hinge Training:
– Practice bending at hips while maintaining neutral spine
– Use dowel along back for immediate feedback
– Master bodyweight pattern before adding resistance
– 3 sets of 15 repetitions daily
Long-Term Prevention Strategies That Keep Pain from Returning
Asymmetrical Maintenance Routine
Weekly self-assessment:
– Check for differences in side-to-side flexibility
– Note any new movement restrictions
– Adjust exercises based on current pain pattern
– Spend extra time on the side showing weakness
Monthly habit adjustments:
– Rotate your computer monitor position
– Alternate which leg you put through pants first
– Change which side you carry bags
– Switch sleeping positions weekly
When to Seek Advanced Care
Consider specialist evaluation if:
– No improvement after 4 weeks of consistent home care
– Pain significantly impacts daily activities like dressing or driving
– New neurological symptoms develop
– Sleep disruption becomes severe
Interdisciplinary approaches combining physical therapy, pain management, and psychological support show best outcomes for chronic shifting back pain. Specialists can identify subtle movement patterns you might miss on your own.
Bottom line: Shifting lower back pain responds best to targeted, asymmetrical treatment. By understanding whether your pain stems from muscles, joints, or discs, you can choose the most effective combination of stretches, exercises, and lifestyle modifications. Most people see significant improvement within 4-6 weeks using these evidence-based strategies. The key is recognizing that your pain moves for specific reasons—and treating those reasons directly rather than applying generic back pain remedies that ignore the shifting pattern. Track your progress, adjust based on which side is currently affected, and you’ll break free from the cycle of side-switching discomfort.