Waking up to searing pain that starts in your lower back and shoots down both legs can be terrifying. This dual-leg sensation isn’t the typical sciatica most people experience—it’s a rarer, more complex condition that demands immediate attention. While standard sciatica usually affects one leg, bilateral symptoms may signal serious spinal involvement that requires precise diagnosis and targeted treatment.
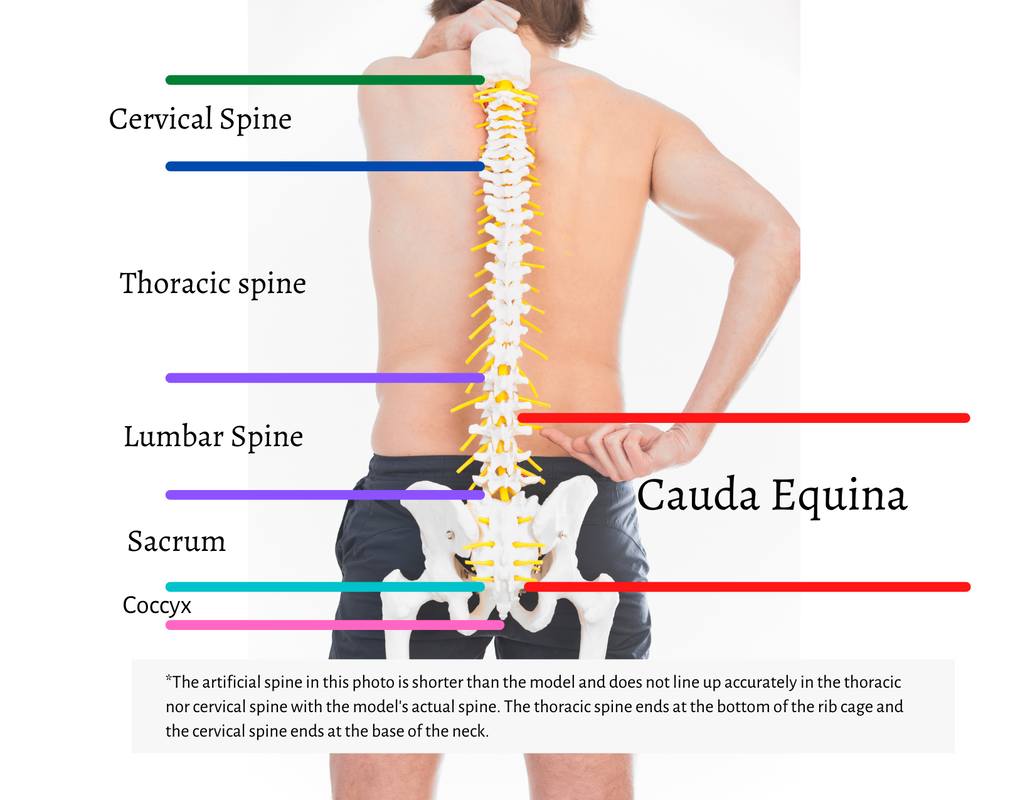
Understanding what’s happening in your body is the first step toward relief. The sciatic nerves, each as thick as your thumb, run from your lower spine through your hips and down each leg. When both nerves become compressed or irritated simultaneously, the resulting pain can range from a dull ache to an electric shock sensation that makes walking nearly impossible. If you’re experiencing lower back pain that radiates down both legs, recognizing this pattern is critical for getting the right treatment before permanent nerve damage occurs.
Why Bilateral Leg Pain Demands Immediate Medical Attention
Lower back pain radiating down both legs represents a medical red flag that requires prompt evaluation. While approximately 40% of Americans experience sciatica in their lifetime, the bilateral presentation affects only a small percentage of cases and often indicates more extensive spinal involvement than single-leg sciatica.
Critical Differences Between Unilateral and Bilateral Sciatica
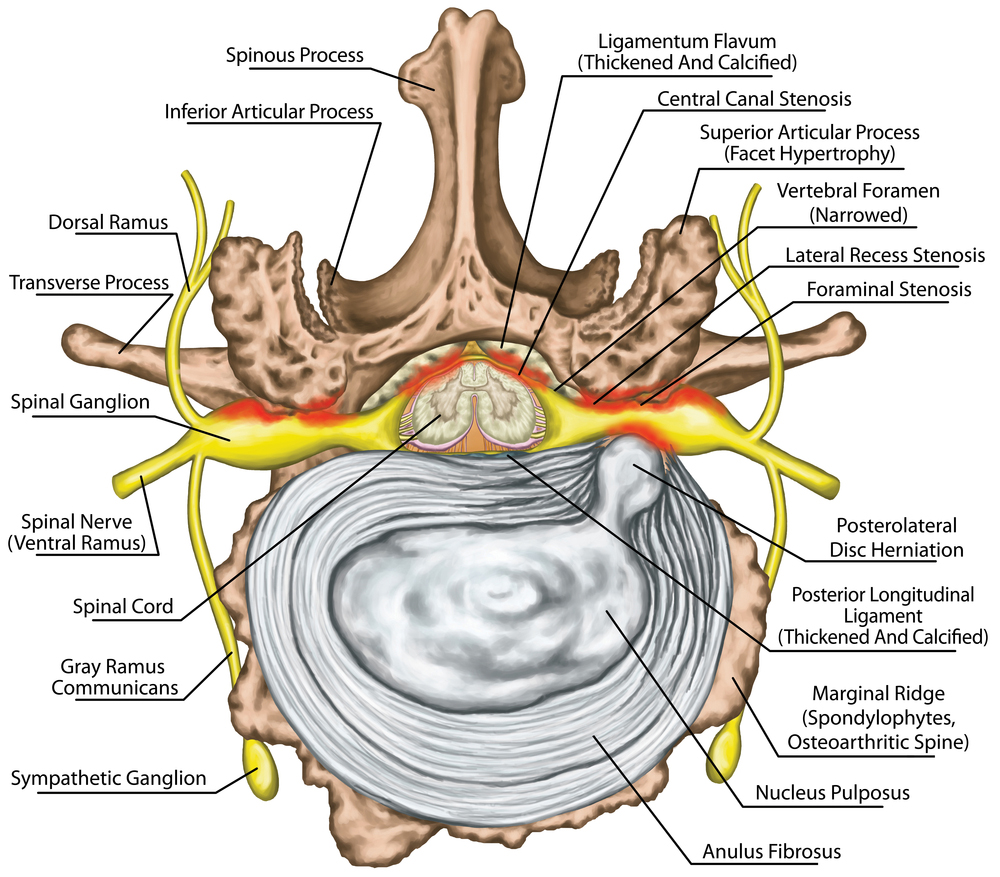
The key distinction lies in the location and extent of nerve compression. Unilateral sciatica typically stems from a single herniated disc pressing on one nerve root, while bilateral symptoms often point to central spinal canal narrowing affecting multiple nerve roots simultaneously. This central compression can result from large disc herniations, severe spinal stenosis, or other conditions that narrow the entire spinal canal rather than isolated nerve pathways.
Warning signs requiring urgent assessment:
– Symmetrical pain patterns affecting both legs equally
– Simultaneous numbness in both feet or toes
– Progressive weakness making standing or walking difficult
– Loss of reflexes in both knees or ankles
Ignoring these symptoms can lead to permanent nerve damage, with research showing treatment delayed beyond six months significantly reduces the likelihood of complete recovery.
Pinpointing the Exact Cause of Your Dual-Leg Pain
Identifying the specific mechanism behind your lower back pain radiating down both legs determines the most effective treatment path. The bilateral nature of your symptoms narrows the potential causes to those affecting the central spinal canal where multiple nerve roots converge.
Central Disc Herniation: The Most Common Culprit
When a large disc herniation occurs in the lower lumbar spine (typically L4-L5 or L5-S1 levels), it can protrude directly backward into the spinal canal, compressing multiple nerve roots simultaneously. Unlike smaller herniations that affect individual nerves, these central protrusions create pressure across the entire canal.
What to look for:
– Pain that worsens with sitting or bending forward
– Symptoms that improve when lying flat
– Numbness patterns following specific dermatomes in both legs
– Possible loss of bowel or bladder control in severe cases
Advanced Spinal Stenosis: The Gradual Onset Threat
Severe narrowing of the spinal canal—often from bone spurs, thickened ligaments, or degenerative changes—can compress nerve roots on both sides. This condition typically develops slowly over years but may cause sudden bilateral symptoms when reaching critical narrowing.
Key indicators:
– Pain that intensifies with walking or standing
– Relief when leaning forward (like pushing a shopping cart)
– Progressive leg weakness during activity
– “Neurogenic claudication” – leg pain that forces you to stop walking
Emergency Warning Signs You Can’t Ignore
Certain symptoms accompanying your lower back pain radiating down both legs require immediate medical intervention. Missing these red flags could result in permanent neurological damage.
Cauda Equina Syndrome: The Surgical Emergency
This rare but devastating condition occurs when multiple nerve roots in the lower spine become severely compressed. While uncommon, it represents a true medical emergency requiring surgical intervention within 24-48 hours to prevent permanent disability.
Must-act-now symptoms:
– Saddle anesthesia – numbness in your groin, inner thighs, or buttocks
– Bladder dysfunction – difficulty starting urination or complete incontinence
– Bowel control loss – unexpected fecal incontinence
– Severe leg weakness – legs suddenly giving way or difficulty lifting feet
Don’t wait to see if these symptoms improve—they require immediate emergency department evaluation.
Diagnostic Process That Actually Finds the Source
Accurate diagnosis of bilateral leg pain requires specific testing protocols that distinguish between central and peripheral nerve compression. Your healthcare provider will use a combination of clinical assessment and imaging to pinpoint the exact cause.
Specialized Physical Examination Techniques
The straight leg raise test, performed on both legs, helps determine which nerve roots are affected and the severity of compression. During this test, your provider will slowly raise each leg while you lie flat, noting when pain begins. Bilateral positive tests strongly suggest central spinal canal involvement rather than isolated nerve compression.
Other critical assessments:
– Gait analysis – observing how you walk reveals neurological compromise
– Reflex testing – checking knee and ankle reflexes on both sides
– Sensory mapping – identifying precise numbness patterns in both legs
– Muscle strength evaluation – detecting subtle weakness in both lower extremities
Essential Imaging Studies for Bilateral Symptoms
MRI provides the clearest view of soft tissues, revealing disc herniations, spinal stenosis, or nerve compression patterns. For bilateral symptoms, your radiologist will specifically examine the central spinal canal width and look for evidence of multi-level nerve root compression.
CT myelogram may be ordered if you can’t have an MRI, combining contrast dye with CT scanning to visualize nerve compression. X-rays alone are insufficient for diagnosing the cause of bilateral leg pain but can reveal structural issues like spondylolisthesis that might contribute to your symptoms.
Targeted Treatment Strategies Based on Severity
Your treatment path depends on the specific cause and severity of your lower back pain radiating down both legs. A precise diagnosis allows for tailored interventions that address the actual source of your bilateral symptoms.
Conservative Treatment Protocol for Mild Cases
For less severe bilateral symptoms without neurological deficits, a structured conservative approach often succeeds:
First 48 hours:
– Rest in comfortable positions (avoid prolonged bed rest)
– Apply ice for 20 minutes every 2 hours
– Use over-the-counter anti-inflammatory medications
Weeks 1-2:
– Begin gentle stretching exercises
– Start walking short distances as tolerated
– Continue heat/ice therapy based on response
Weeks 3-6:
– Gradual return to normal activities
– Physical therapy for core strengthening
– Consider epidural steroid injections if pain persists
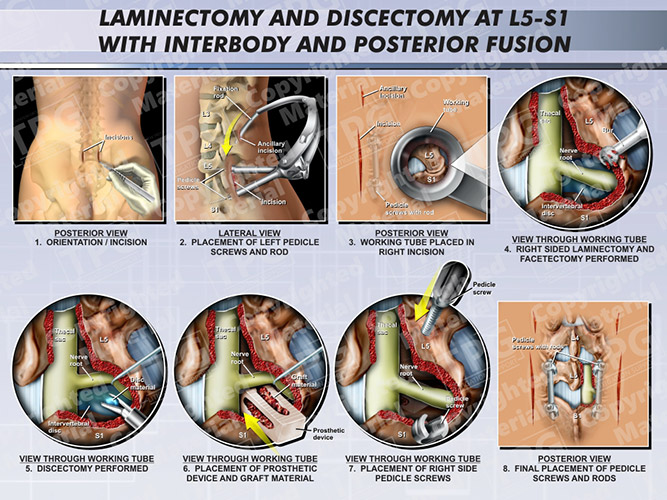
When Surgery Becomes Your Best Option
Surgical intervention for bilateral sciatica becomes appropriate when:
– Conservative measures fail after 6-8 weeks
– Progressive neurological deficits appear
– Evidence of significant nerve compression exists on imaging
– Daily activities become impossible due to pain
Effective surgical procedures:
– Microdiscectomy – removes herniated disc fragments through a small incision
– Laminectomy – removes portions of vertebra to create more space for nerves
– Foraminotomy – widens the openings where nerves exit the spine
Preventing Future Episodes Through Smart Daily Habits
Once your acute symptoms improve, preventing recurrence requires specific lifestyle modifications that address the underlying causes of your bilateral leg pain.
Workplace Adjustments That Make a Difference
Position your computer screen at eye level to prevent forward head posture. Use a chair with proper lumbar support and take standing breaks every 30 minutes. Consider a sit-stand desk to vary your position throughout the day—this simple change can reduce spinal pressure by up to 30% compared to sitting continuously.
Essential office modifications:
– Keep feet flat on the floor or footrest
– Maintain a 90-degree angle at hips and knees
– Avoid crossing legs while seated
– Use armrests to prevent shoulder hunching
Safe Exercise Strategies for Long-Term Relief
Focus on exercises that strengthen your core without stressing your spine. Proven effective activities include:
– Swimming (especially backstroke)
– Stationary cycling with proper posture
– Walking on flat surfaces
– Modified yoga poses avoiding forward bends
Immediately stop these movements:
– Heavy deadlifts or squats
– Toe touches or deep forward bends
– High-impact activities like running
– Twisting movements with load
Emergency Preparedness Plan for Sudden Worsening
Create an action plan for symptom exacerbation. Keep emergency contact information readily available, including your healthcare provider’s after-hours number. Understand which urgent care facilities have spine specialists available. Prepare a go-bag with comfortable clothes, medications list, and insurance information for unexpected ER visits.
Immediate response protocol:
1. Assess for red flag symptoms (bladder issues, saddle numbness)
2. Contact healthcare provider or go to ER immediately
3. Document symptom onset and progression details
4. Avoid driving yourself if experiencing leg weakness
Bottom line: Lower back pain that radiates down both legs represents a medical concern requiring prompt evaluation due to potential central spinal canal involvement. While most sciatica cases affect only one leg, the bilateral presentation demands thorough investigation to rule out serious conditions like cauda equina syndrome. Early diagnosis and appropriate intervention offer the best chance for complete recovery and prevention of long-term complications. Remember that treatment delayed beyond six months significantly reduces the likelihood of good outcomes—don’t wait when both legs are affected. Your path to relief begins with understanding the specific cause of your symptoms and taking targeted action based on professional medical guidance.

