You slide into your desk chair feeling perfectly fine—then 45 minutes later, a sharp ache grips your lower back. The moment you stand to grab coffee, the pain vanishes. Sit back down? It returns instantly. If this cycle sounds familiar, you’re not imagining things. Lower back pain when sitting but not standing affects 70% of office workers and drivers, yet most suffer silently, thinking it’s “just part of the job.” The truth? Your spine isn’t broken—it’s being crushed by physics. This guide reveals exactly why sitting triggers pain while standing relieves it, along with immediate fixes you can implement before lunchtime.
Why Sitting Crushes Your Lumbar Discs

Sitting isn’t passive—it’s a high-stress position that overloads your lumbar discs by 40–50% compared to standing. When you sink into your chair, gravity forces your pelvis backward, flattening your spine’s natural inward curve. This “posterior pelvic tilt” shifts weight onto passive structures like ligaments and discs instead of your core muscles. Now add slouching: that extra 90° forward bend multiplies disc pressure to nearly double standing levels, forcing jelly-like disc material toward nerve roots. Meanwhile, your hip flexors shorten like tightened cables, pulling your pelvis into anterior tilt and straining spinal joints. Within 20 minutes, blood flow to supporting muscles drops 30%, starving tissues of oxygen and accelerating micro-tears.
How Your Chair Turns Against You
That “comfortable” reclined position? It’s a trap. Sitting at 120° (common in lounge chairs) increases disc pressure 40% more than upright sitting. Even “ergonomic” chairs fail if lumbar support doesn’t match your spine’s unique inward curve. Without it, your discs bear 220 lbs of compressive force per hour—like stacking cinder blocks on a sponge.
Why Standing Feels Instant Relief
Standing automatically reactivates your glutes and core, restoring spinal alignment. Your pelvis tilts forward, reinstating the lumbar curve that cushions discs. Blood flow surges 50% to starved muscles, flushing out pain-inducing metabolic waste. This isn’t magic—it’s biomechanics working as designed.
3-Minute Pain Relief Tactics for Your Next Meeting
Reset Your Spine With Micro-Movements
Stand every 30 minutes for 90 seconds—no walking required. Simply:
1. Pelvic tilts: Stand tall, gently arch lower back (anterior tilt), then flatten against wall (posterior tilt). Repeat 5x.
2. Hip hinges: Place hands on desk, push hips backward while keeping spine straight. Hold 10 seconds.
Why it works: These reactivate inhibited glutes and relieve disc pressure in under 2 minutes.
Create Instant Lumbar Support
Fold a towel into a 4″ cylinder and wedge it at the inward curve of your lower back. Critical detail: Position it 2 inches above your belt line—not in the hollow of your back. This maintains natural lordosis, reducing disc load by 25%. No towel? Roll your sweater sleeve—it’s more effective than most $300 “ergonomic” cushions.
Targeted Desk Stretches That Actually Work
Do these seated without drawing attention:
– Seated figure-4 stretch: Cross right ankle over left knee, gently lean forward until you feel hip release. Hold 30 seconds.
– Chair cat-cow: Place hands on knees, arch spine upward (cat), then dip chest while lifting tailbone (cow). Repeat 8x.
Pro tip: Pair with deep exhales—this triggers parasympathetic response to reduce pain signals.
Pinpoint Your Exact Pain Cause (Before It Worsens)
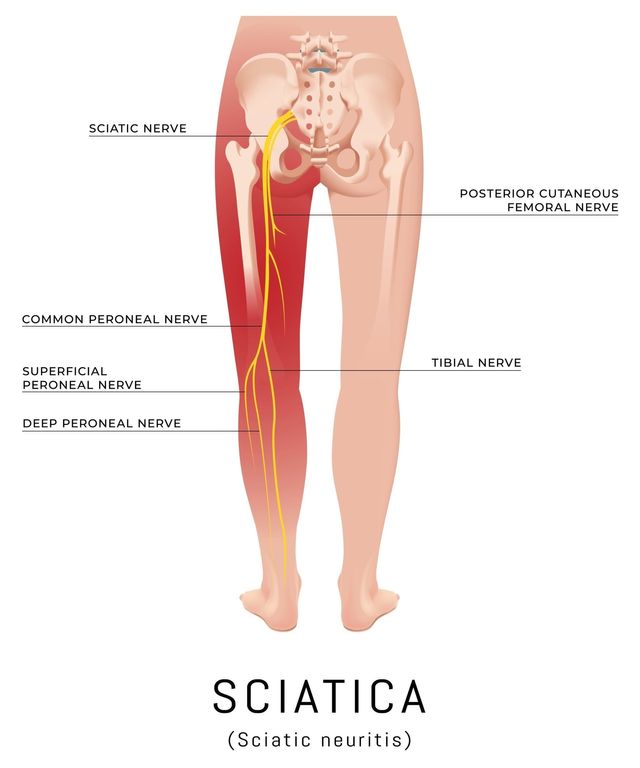
Central Ache vs. Shooting Pain: What It Means
- Dull ache centered in lower back: Classic discogenic pain from prolonged compression. Fixes posture first.
- Pain shooting below the knee: Nerve involvement (sciatica or herniated disc). Requires professional assessment within 2 weeks.
- Buttock pain worsened by sitting: Piriformis syndrome—your sciatic nerve is being strangled by a tight hip muscle.
Emergency Warning Signs You Can’t Ignore
Seek immediate care if you experience:
– Numbness in inner thighs/groin (like sitting on a saddle)
– Sudden foot weakness (tripping on stairs)
– Loss of bladder control
These indicate cauda equina syndrome—a spinal emergency requiring surgery within 48 hours.
Transform Your Workspace in 10 Minutes
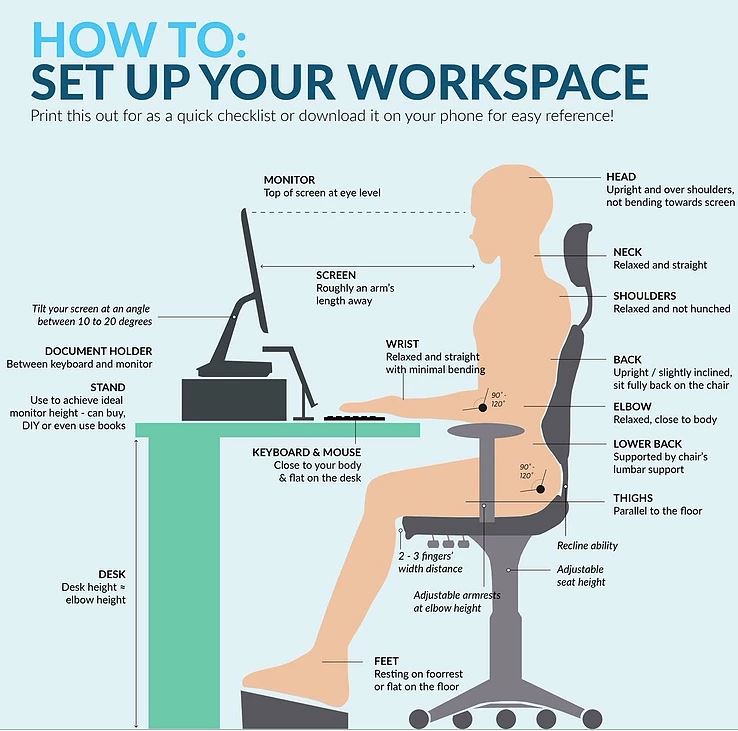
Chair Hacks That Beat $500 “Ergonomic” Models
- Lumbar lock: Use a rolled yoga mat instead of flimsy cushions—it won’t collapse under pressure.
- Foot elevation: If feet dangle, stack books under a stool. Knees must be level with hips.
- Monitor height: Rest laptop on inverted cardboard box so top screen edge aligns with your eyebrows.
Test: Sit with arms relaxed at 90°. If shoulders hike toward ears, lower your desk.
The 40% Pressure-Reduction Trick
Stand for just 15 minutes hourly using a $20 laptop riser on your kitchen counter. This slashes cumulative disc pressure by 40%—more effective than any chair. Standing desk users report 62% less sitting pain within 2 weeks. No budget? Alternate sitting on an exercise ball (20 mins) and your chair.
Your First 72-Hour Pain-Reduction Plan
Day 1: Break the Cycle
- Every 30 minutes: Stand and perform 5 pelvic tilts against a wall.
- After lunch: 3 sets of glute bridges (lie on floor, lift hips while squeezing glutes).
- Before bed: Place pillow between knees if side-sleeper (prevents spinal twist).
Day 2: Activate Dormant Muscles
- Morning: 2-minute plank (on knees if needed) to wake up transverse abdominis.
- Commute: Perform seated hip flexor stretches at red lights (kneel in passenger seat, shift pelvis forward).
- Work: Set phone alarm labeled “SPINE RESET” every 45 minutes.
Day 3: Sustain the Gains
- Replace coffee breaks with 90-second walking breaks—circulation is your best painkiller.
- Ditch sit-ups: They increase disc pressure 40% more than crunches. Stick with dead bugs instead.
- Track progress: Note pain levels hourly in your notes app. Most see 50% improvement by Day 3.
Critical Mistakes That Make Sitting Pain Worse
Don’t over-rely on heating pads—they relax muscles but weaken core stability long-term. Use heat only for acute stiffness after movement. Never skip foot support: Dangling feet increase disc pressure 20% by straining hamstrings. Avoid “ergonomic” chairs with fixed lumbar curves—they force unnatural alignment if mismatched to your spine. Worst offender? Waiting for pain before moving. By the time you feel discomfort, micro-damage is already done.
When to Call a Specialist (Not Google)
See a physical therapist if:
– Pain persists beyond 14 days despite position changes
– You need to take NSAIDs daily just to function
– Standing longer than 20 minutes now causes new pain
Red flag: If sitting pain wakes you at night, this indicates inflammatory pathology needing urgent imaging. Most cases resolve in 6-8 weeks with targeted core rehab—no drugs or surgery required.
Your spine wasn’t designed for static sitting—it craves dynamic movement. By implementing just one change today (set that 30-minute timer!), you disrupt the pain cycle before it starts. Remember: standing doesn’t “fix” your back—it simply stops the crushing force sitting creates. Pair strategic movement with lumbar support, and you’ll reclaim pain-free workdays. The real solution isn’t avoiding sitting—it’s sitting smarter. Start now: place that towel roll behind your lower back and reset your posture. Your next meeting will feel different.

