You’re halfway through your work shift when a familiar ache creeps into your lower back. By hour six, that dull throb has become a sharp stab with every step. If this scenario sounds painfully familiar, you’re among the 619 million people worldwide currently battling lower back pain—80% of whom experience it specifically when standing. This guide delivers actionable solutions backed by clinical evidence, helping you understand why standing triggers pain and exactly how to stop it.
Most cases stem from mechanical issues that respond well to targeted interventions. When you stand, your lumbar spine bears 60% of your upper body weight, compressing discs and fatiguing muscles designed for intermittent loading. Within just two hours, intervertebral discs lose 20% of their fluid volume, reducing shock absorption and increasing nerve compression risk. The good news? 97% of lower back pain when standing is mechanical and self-limiting with proper management.
Why Standing Turns Your Spine Against You
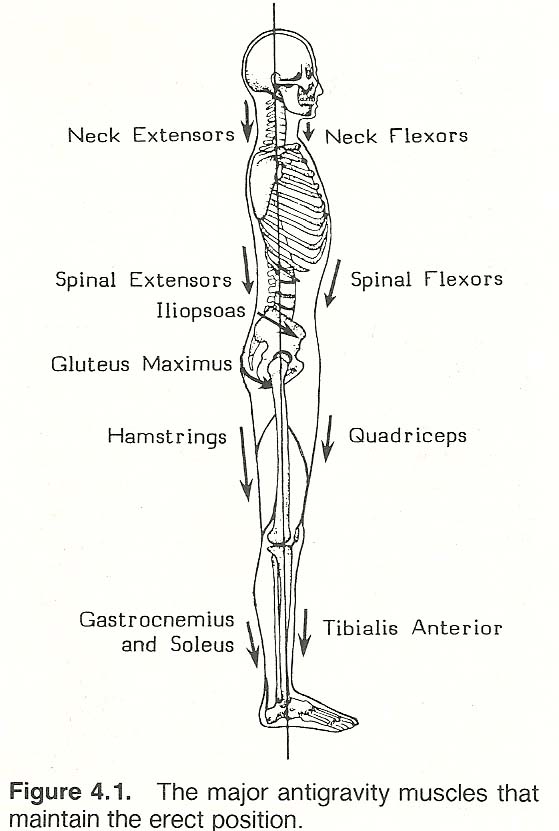
Standing transforms gravity from a neutral force into a compressive enemy. Your paraspinal muscles contract continuously to maintain upright posture, triggering fatigue within minutes. Hard surfaces worsen this by eliminating natural shock absorption, while locked knees and poor alignment multiply spinal stress. Research shows 50% of healthy volunteers develop temporary low-back pain after two hours of standing due to muscle exhaustion—a precursor to chronic issues.
Critical biomechanical chain reaction:
– Pelvic misalignment shifts weight distribution unevenly
– Intervertebral discs thin under sustained vertical load
– Nerve roots get compressed in narrowed spinal spaces
– Compensatory postures strain hip flexors and hamstrings
Muscle Fatigue vs. Disc Damage: Spot the Difference
Muscle strain pain (70% of cases) feels like:
– Central aching or throbbing in the lower back
– Tenderness when pressing on the affected area
– Radiating discomfort to buttocks but rarely past knees
– Relief when changing positions or applying heat
Disc-related pain warns with:
– Sharp, electric sensations shooting below the knee
– Tingling or numbness in legs increasing with upright posture
– Morning stiffness that improves with movement
– Worsening pain when bending backward (unlike muscle pain)
90-Second Posture Reset Protocol
Immediate corrections to stop pain mid-stand:
1. Unlock your knees: Maintain a micro-bend to reduce lumbar compression
2. Engage deep core: Gently draw navel toward spine without holding breath
3. Stack alignment: Position ears directly over shoulders over hips
4. Shift weight: Alternate pressure between feet every 30 seconds
5. Tuck pelvis: Tilt backward slightly to restore natural lumbar curve
Pro tip: Set phone alarms every 20 minutes. When they chime, perform the “standing pelvic tilt”—gently rock hips forward and backward 5 times while maintaining soft knees. This dynamic movement prevents static fatigue better than rigid posture holds.
Targeted 5-Minute Standing Stretches
Standing Hamstring Release
Place one heel on a low step or stool, keeping your knee straight. Hinge forward from hips (not waist) until you feel tension in the back of your thigh. Hold 30 seconds while breathing deeply—never force the stretch. Repeat twice per leg. Tight hamstrings pull your pelvis into posterior tilt, directly straining the lower back during standing.
Hip Flexor Opener
Step one foot back into a gentle lunge, keeping your front knee aligned over ankle. Tuck your pelvis backward until you feel a stretch along the front of your back hip. Hold 30 seconds per side. This counteracts the shortened hip flexors from prolonged standing that tilt your pelvis forward and compress lumbar discs.
Standing Child’s Pose
Feet hip-width apart, fold forward at hips with knees slightly bent. Let arms hang heavy or rest hands on thighs. Breathe into your lower ribs for 45 seconds. This decompresses vertebrae while maintaining blood flow—critical for pain relief when you can’t sit down.
Workstation Fixes That Actually Work
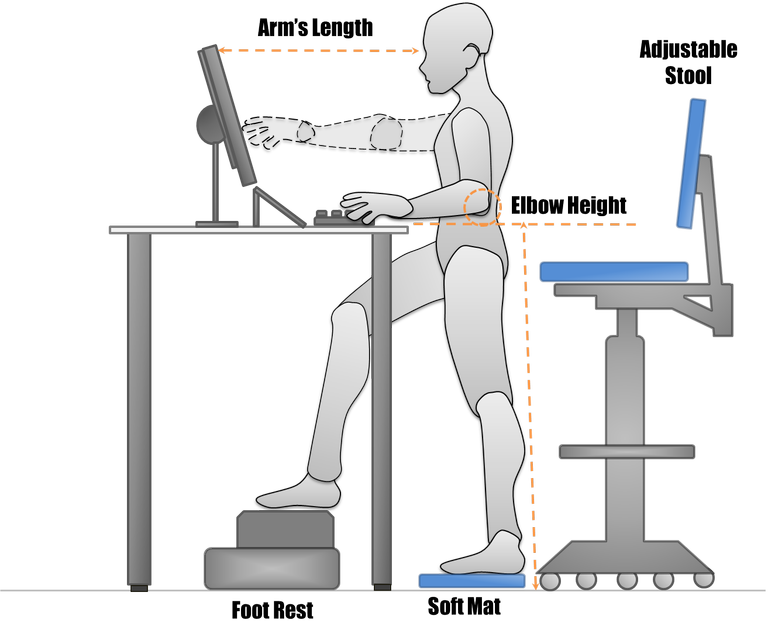
Anti-Fatigue Mat Protocol
Place ¾-inch thick mats directly under your primary standing zone. Replace them every 6-12 months as compressed material loses shock absorption. Stand with feet shoulder-width apart to maximize stability—narrow stances increase spinal load by 25%. For added benefit, shift weight between feet every 5 minutes while standing on the mat.
Footrest Rotation System
Use a 6-8 inch stool to elevate one foot periodically. Alternate feet every 20 minutes to change pelvic tilt angles and relieve disc pressure. This simple technique reduces nerve root compression by allowing intermittent spinal decompression—proven to decrease pain intensity by 40% in standing workers.
Surface Height Calibration
Adjust work surfaces so elbows form 90-degree angles when typing. Keyboards should sit at hip level with monitors at eye height. Incorrect heights force forward head posture, increasing cervical strain that cascades down to your lower back. Test your setup: if you catch yourself jutting your chin forward while working, your screen is too low.
Shoe Selection Criteria That Prevent Pain
Choose footwear with:
– Moderate arch support (neither flat nor excessive)
– Memory foam or gel midsole cushioning
– Heel height under 2 inches to avoid pelvic tilt
– Replace every 6-9 months or 300-500 miles
Immediately eliminate:
– Completely flat shoes (flip-flops, ballet flats)
– High heels over 2 inches
– Worn-out soles with visible compression
Footwear directly impacts spinal alignment. Shoes without cushioning transmit 30% more ground impact force to your lumbar spine during standing. Opt for athletic shoes with rocker soles—they mimic natural gait mechanics even when stationary.
Core Strengthening Circuit for Standing Endurance
Daily 10-minute routine (do before work):
1. Bird-dog: 3 sets of 10 reps per side (improves spinal stability)
2. Side planks: 3×30 seconds per side (targets obliques that prevent swayback)
3. Dead bugs: 2 sets of 15 reps (trains deep core without spinal flexion)
4. Glute bridges: 3 sets of 15 (activates posterior chain to support lumbar spine)
Progression rule: Add 5 seconds to holds weekly. Strong glutes and core muscles reduce disc compression by 50% during standing—making this the single most effective long-term solution for lower back pain when standing.
Heat vs. Ice Protocol Decoded
Acute Pain (First 48 Hours)
Apply ice packs wrapped in thin towels for 15 minutes on, 45 minutes off. Repeat 3-4 times daily to reduce inflammation from sudden muscle strain. Never apply ice directly to skin—frostbite risk increases significantly on inflamed tissues.
Chronic Pain (After 48 Hours)
Use moist heat for 20 minutes twice daily. Heat relaxes hypertonic muscles and improves blood flow to stiff joints. Best method: take a warm bath with Epsom salts while performing seated pelvic tilts—this combines thermal therapy with gentle mobilization.
Emergency Warning Signs Requiring Immediate Action
Go to ER Now If You Experience:
- Loss of bladder/bowel control with back pain
- Numbness in groin or inner thighs (“saddle anesthesia”)
- Leg weakness causing frequent tripping
- Severe pain after falls or trauma
Schedule Doctor Within 1 Week For:
- Pain persisting beyond 6 weeks despite home care
- Nighttime pain disrupting sleep
- Radiating leg numbness worsening daily
- Unexplained weight loss with back symptoms
These red flags indicate possible cauda equina syndrome, infection, or tumor—accounting for less than 2% of cases but requiring urgent intervention.
Pain Prevention Checklist
Daily non-negotiables:
– [ ] Micro-breaks every 20 minutes (walk 30 seconds)
– [ ] Posture checks using phone timer alerts
– [ ] Morning/evening hamstring stretches
– [ ] Rotate footwear to avoid repetitive strain
– [ ] Core activation before prolonged standing
Weekly maintenance:
– [ ] Clean anti-fatigue mats to maintain cushioning
– [ ] Test workstation alignment with mirror
– [ ] Track pain patterns in symptom journal
– [ ] Increase exercise duration by 10%
Consistency matters most: Those performing daily core exercises reduce recurrence risk by 70% compared to passive stretching alone.
Immediate relief strategy: When pain strikes, immediately sit or lie supine for 10 minutes while applying heat. Then walk short distances—movement prevents stiffness better than prolonged rest. For long-term resolution, combine workstation adjustments with the 10-minute core circuit. Most standing-related back pain improves dramatically within 6 weeks using these evidence-based strategies, but 20% of cases persist without proper intervention. Your spine thrives on movement variation, not static perfection—small, consistent changes create lasting relief where you stand.

