That persistent ache radiating from your lower back into your hips isn’t something you should just “live with.” If you’ve tried general back pain advice that worked for your male colleagues but does nothing for your specific discomfort, there’s a reason. Women’s bodies process pain differently, and the combination of lower back and hip pain often stems from factors unique to female anatomy and physiology.
Unlike generic back pain guides that ignore gender differences, this resource addresses why your pain might flare before your period, worsen after pregnancy, or resist standard treatments. Millions of women experience this dual-site pain, yet too many receive dismissive responses when seeking help. Understanding the distinct female factors at play is the first step toward meaningful relief.
Female-Specific Pain Patterns You Should Recognize

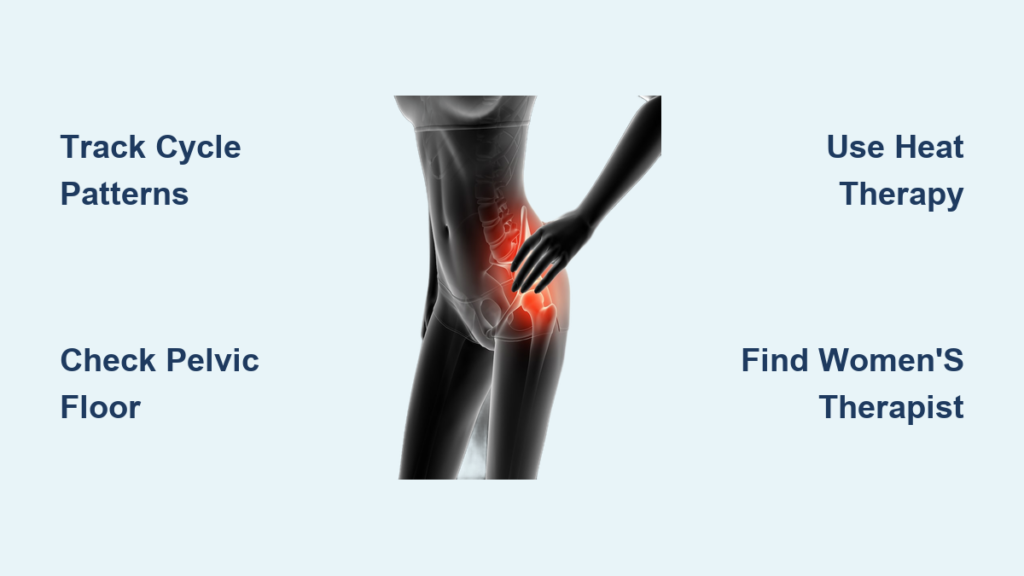
Tracking Your Pain Cycle Correlations
Your pain likely follows patterns tied to your menstrual cycle that standard pain charts ignore. Many women experience intensified discomfort during ovulation and menstruation when hormonal fluctuations affect tissue stability. Instead of tracking pain on a generic calendar, document symptoms alongside your cycle phases for two full months. Note whether pain increases when ligaments naturally loosen during high-estrogen periods—this correlation often gets overlooked in standard evaluations.
Postural Stress Points Unique to Women
Daily activities create different stress patterns in female bodies due to wider pelvic structures and center of gravity differences. Carrying bags on one shoulder, wearing certain footwear, or sitting in office chairs designed for male proportions can trigger or worsen pain in ways that don’t affect men. Pay attention to which positions provide genuine relief versus those that seem neutral but actually strain your specific anatomy. Women often unknowingly adopt compensatory postures that create secondary pain patterns.
Understanding Pain Quality Differences
Sharp, localized pain often indicates specific joint involvement, while diffuse aching usually signals broader muscular strain. Women frequently experience referred pain from pelvic structures that feels like standard back pain but requires completely different treatment. Document whether your pain changes with bladder or bowel activity—this crucial detail helps distinguish between musculoskeletal issues and potential gynecological causes that standard back exams miss.
Why Standard Treatments Often Fail Women

Hormonal Influences on Tissue Response
Estrogen directly affects collagen production throughout your body, including ligaments supporting your spine and hips. During high-estrogen phases, these tissues become more elastic, potentially creating joint instability that triggers pain. This explains why some women experience increased discomfort mid-cycle when standard treatments seem less effective. Women’s connective tissue also responds differently to therapeutic exercises due to these hormonal fluctuations.
The Pelvic Floor Connection Most Providers Overlook
Your pelvic floor muscles directly connect to lower back and hip structures through shared fascial lines. Childbirth, chronic straining, or even certain exercise routines can create imbalances that manifest as back and hip pain. Many women discover their “back problem” actually originates from untreated pelvic floor dysfunction—a connection that requires specialized assessment most general practitioners don’t perform.
Structural Changes That Persist Post-Pregnancy
Even years after delivery, your body retains adaptations from pregnancy that affect pain patterns. The hormone relaxin causes permanent changes in ligament laxity for some women, while abdominal separation creates lasting core stability issues. These structural differences mean standard postpartum recovery timelines often don’t apply, leaving women confused when pain persists beyond the “expected” recovery period.
Getting the Right Diagnosis: A Woman’s Roadmap
Creating a Pain Journal That Actually Helps Providers
Standard pain scales often fail to capture the complexity of female lower back and hip pain. Your symptom log should include: pain intensity relative to menstrual cycle phase, specific movements that trigger relief (not just worsening), and whether symptoms change with bladder/bowel activity. Note any correlation between pain levels and hormonal contraception use—this detail provides crucial diagnostic clues many providers miss during brief appointments.
Questions to Ask During Your Physical Exam
Most standard back examinations don’t assess female-specific structural considerations. Request evaluation of sacroiliac joint function, hip rotation range of motion, and pelvic alignment—issues that disproportionately affect women. Ask specifically about piriformis syndrome testing, as this common female pain generator often mimics disc problems. A thorough assessment should include both standing and weight-bearing positions to identify functional imbalances.
When Standard Imaging Doesn’t Tell Your Story
X-rays frequently appear normal in women with significant pain because many female-specific causes involve soft tissues rather than bone structure. If initial imaging shows “nothing wrong” but your pain persists, discuss whether ultrasound or MRI might better visualize pelvic floor muscles, hip labrum, or reproductive organs. Women’s pain often originates in structures that don’t show on basic X-rays, requiring more targeted imaging approaches.
Immediate Relief Strategies That Respect Female Physiology
Heat Therapy Protocol for Women’s Pain Patterns
Apply heat to both lower back and hips simultaneously for 15-20 minutes using a large heating pad or warm bath. Women’s pelvic structures often have reduced circulation due to anatomical positioning, making heat particularly effective for increasing blood flow to these areas. Use this protocol 2-3 times daily during acute flare-ups, but avoid during heavy menstrual bleeding when increased circulation might worsen discomfort.
Targeted Stretching That Works With Your Cycle
Focus on hip flexors, piriformis, and gluteal muscles that commonly tighten in women due to pelvic alignment. Hold each stretch for 30-45 seconds while breathing deeply to activate your parasympathetic nervous system. Time your stretching according to your cycle—gentler during menstruation when ligaments are naturally looser, more active during follicular phase when joints are more stable. This approach prevents overstretching during vulnerable times.
Positioning Techniques for Female Sacroiliac Relief
Lie on your back with knees bent and place a pillow between your knees to maintain hip alignment. This position decompresses the sacroiliac joints that commonly become irritated in women due to wider pelvic structure. Use this position for 10-minute breaks throughout your day, especially after prolonged sitting. Women’s SI joints respond particularly well to this simple alignment adjustment that’s rarely suggested in generic back pain advice.
Long-Term Solutions Beyond Generic Advice

Finding a Women’s Health Physical Therapist
Seek practitioners specializing in female pelvic and musculoskeletal health—not just general physical therapists. Effective treatment should include manual therapy for sacroiliac dysfunction, pelvic floor muscle coordination training, and movement re-education addressing female-specific biomechanics. These specialists understand how pregnancy history, menstrual cycle, and hormonal status affect treatment response—knowledge most general therapists lack.
Core Strengthening That Actually Helps Women
Traditional core exercises frequently worsen female back pain by over-recruiting hip flexors instead of targeting deep stabilizers. Focus on transverse abdominis activation combined with pelvic floor coordination—this integrated approach builds true core stability without straining vulnerable structures. Women typically need slower progression in strength training due to hormonal influences on tissue adaptation, so patience with gradual loading is essential.
Hormonal Considerations in Pain Management
Discuss with your healthcare provider whether hormonal contraceptives might be contributing to or helping your pain. Some women find relief with continuous cycling methods that minimize hormonal fluctuations, while others need to avoid synthetic hormones entirely. Track your pain patterns relative to any hormonal interventions—this personalized data provides more insight than general medical guidelines that don’t account for individual variation.
When to Seek Specialized Care: Red Flags for Women
Symptoms That Require Immediate Attention
Seek prompt medical evaluation for pain accompanied by bowel or bladder changes, unexplained weight loss, or progressive leg weakness. Women often dismiss these warning signs as “normal” when they actually indicate conditions requiring urgent intervention. Pain that wakes you from sleep or prevents basic self-care activities like putting on shoes signals mechanical dysfunction needing specialized assessment.
Identifying the Right Specialist for Female Pain
Choose providers with documented experience in female musculoskeletal issues. Ask potential practitioners specifically about their approach to pregnancy-related pain, menstrual cycle influences, and pelvic floor dysfunction. The right specialist understands how these female-specific factors require treatment modifications that standard protocols ignore. Don’t settle for practitioners who dismiss your pain as “just part of being a woman.”
Your lower back and hip pain isn’t an inevitable burden of womanhood—it’s a signal that your unique anatomy needs specialized attention. By recognizing how female physiology affects pain patterns and treatment response, you can move beyond generic advice that doesn’t work. Start with the positioning techniques today, then build a personalized plan that respects your body’s natural rhythms. Most importantly, trust your experience when standard approaches fail—your pain deserves solutions designed specifically for the female body.