That deep, relentless ache between your shoulder blades that won’t ease with stretching or massage might not be a muscle problem at all. For thousands of people each year, back pain that refuses to respond to typical treatments reveals an unexpected source: the pancreas. While most back pain originates from muscles, joints, or nerves, pancreatic conditions create a distinctive pattern of discomfort that’s often misdiagnosed for months. Understanding exactly where pancreatic back pain occurs—and how it differs from common back pain—can mean the difference between early detection and delayed treatment.
This guide maps the specific location patterns, characteristics, and warning signs that distinguish pancreatic back pain from mechanical causes. You’ll learn to recognize when that stubborn back ache deserves immediate medical attention, potentially catching serious conditions before they progress. If you’ve been experiencing persistent mid-back discomfort without clear cause, this information could be life-changing.
Mid-Back Band Pain: Your Pancreas’s Distress Signal
The pancreas sits deep in your upper abdomen, nestled behind your stomach and extending toward your spine. When pancreatic tissue becomes inflamed or develops tumors, this positioning creates a distinctive pain pattern across your upper back that follows specific anatomical boundaries.
Horizontal Pain Zone Just Below Shoulder Blades
Precise location: Pancreatic back pain most commonly appears as a horizontal band across your mid-back, centered between your shoulder blades at the level of your eighth to tenth thoracic vertebrae. This isn’t localized to one spot—it spans from one side of your back to the other, creating what patients describe as a “tight belt” of discomfort.
What to check: Stand in front of a mirror and place your hands on your hips. The pain zone typically falls just above where your hands rest, creating a continuous band of discomfort that wraps around your torso. Unlike muscle knots that you can pinpoint with your finger, this pain feels diffuse and deep.
Why it matters: This horizontal band pattern is one of the strongest indicators of pancreatic involvement. When your pain follows this specific distribution, especially when combined with upper abdominal discomfort, it creates a red flag your doctor shouldn’t ignore.
Interscapular and Sub-Scapular Pain Patterns
Between the shoulder blades: Directly in the interscapular region, pancreatic pain creates a deep, gnawing sensation that feels like it’s coming from inside your body rather than from surface muscles. You might find yourself constantly shifting positions trying to relieve pressure that won’t go away.
Under the shoulder blades: The pain frequently extends just beneath your shoulder blades, creating a dull ache that intensifies when you lie flat on your back. Many patients initially mistake this for poor posture or a pulled muscle, wasting precious time on ineffective treatments.
Key differentiator: Unlike mechanical back pain that responds to massage or stretching, pancreatic-related discomfort remains stubbornly present regardless of your position—except when you lean forward, which often provides temporary relief.
Why Your Pancreas Makes Your Back Hurt

Understanding the nerve pathways that create this referred pain helps you recognize when back pain signals pancreatic trouble rather than a simple muscle strain.
Nerve Pathways Connecting Pancreas to Back
When your pancreas becomes inflamed or develops tumors, it directly impacts the complex network of nerves running along pancreatic blood vessels. These nerves connect to the same pathways serving your mid-back region, creating referred pain that your brain interprets as coming from your back. This neurological crossover explains why you feel back pain when the problem originates deep in your abdomen.
Critical warning sign: If your back pain appears suddenly alongside upper abdominal discomfort—particularly after eating—you’re experiencing the classic front-to-back pain transmission pattern of pancreatic distress. The pain feels like it’s wrapping around your entire upper torso rather than being isolated to one area.
Positional Clues That Reveal Pancreatic Origin
Lying flat intensifies pain: Pancreatic back pain typically worsens when you lie on your back because this position increases pressure between the inflamed pancreas and your spine. Many patients discover their condition when back pain becomes severe enough to wake them at night.
Forward leaning provides relief: Leaning forward while sitting or curling into a fetal position often reduces pancreatic pain intensity. This simple test can help distinguish pancreatic pain from mechanical causes—try sitting forward in a chair for 5 minutes. If your pain noticeably decreases, pancreatic involvement becomes more likely.
Pancreatitis vs. Cancer: Location Differences That Matter

While both conditions cause back pain, specific location patterns provide crucial diagnostic clues that could accelerate your path to proper treatment.
Acute Pancreatitis Pain Patterns
Rapid onset: Pain appears suddenly in your upper abdomen and shoots through to your back within hours. The intensity matches exactly between front and back, creating what patients describe as a “hot poker” sensation straight through the torso.
Abdominal dominance: With acute pancreatitis, the upper abdominal pain remains more severe than the back component. The back pain serves as a secondary radiation rather than your primary complaint.
Widespread distribution: Inflammation can cause pain that spreads diffusely across your upper back, sometimes reaching as high as your lower neck region, creating a broader pain pattern than pancreatic cancer.
Pancreatic Cancer Pain Patterns
Back-dominant presentation: Cancer-related pain often presents primarily as back pain, with milder abdominal discomfort that patients may initially overlook. The back pain becomes your chief complaint while abdominal symptoms develop later.
Progressive worsening: Unlike acute pancreatitis, cancer-related back pain starts mild and gradually intensifies over weeks or months. The location remains consistent but the severity escalates steadily.
Specific vertebral involvement: Advanced cases may cause localized pain at specific thoracic vertebrae where tumors press directly against the spine, creating pinpoint tenderness that differs from the broader band pattern of pancreatitis.
Red Flags That Demand Immediate Medical Attention
Certain pain characteristics strongly indicate pancreatic origin rather than mechanical back problems. Don’t ignore these warning signs:
Weight Loss + Back Pain Combination
Unintended weight loss of 10+ pounds without dietary changes, combined with persistent mid-back pain, creates a high-risk scenario for pancreatic cancer. This combination occurs in over 75% of pancreatic cancer cases. If you’re losing weight while experiencing unexplained back pain, seek medical evaluation immediately.
Food-Triggered Pain Episodes
Pain that spikes dramatically after eating—especially high-fat meals—indicates pancreatic involvement. This happens because your pancreas works harder to produce digestive enzymes, putting additional stress on already compromised tissue. If your back pain consistently worsens 30-60 minutes after meals, document this pattern carefully for your doctor.
Constant, Unrelenting Pain
Unlike mechanical back pain that fluctuates with activity, pancreatic back pain maintains consistent intensity regardless of what you do. This relentless quality is one of the most telling signs—if your pain never truly eases, even during rest, it suggests organ involvement rather than musculoskeletal strain.
Position Tests to Identify Pancreatic Back Pain
You can perform simple positional tests at home to gather evidence for your doctor about potential pancreatic involvement.
The Supine Test
Lie flat on your back for 5-10 minutes. Pancreatic back pain typically intensifies significantly during this position because it increases pressure between your inflamed pancreas and spine. If your pain noticeably worsens while lying flat but improves when you sit up, this strongly suggests pancreatic origin.
The Forward Flexion Test
Sit in a chair and lean forward, resting your elbows on your knees for 5 minutes. Pancreatic pain often decreases in this position because it relieves pressure on the affected nerves. If leaning forward provides temporary relief that sitting upright doesn’t, document this pattern—it’s a valuable diagnostic clue for your physician.
Action Steps When Pancreatic Back Pain Is Suspected
If your pain matches these pancreatic patterns, taking swift, informed action can significantly impact outcomes.
Document Your Symptoms Precisely
- Track timing: Note when pain started, how it has progressed hourly/daily, and any specific triggers
- Record positional changes: Document exactly how pain responds to lying flat, sitting upright, and leaning forward
- Monitor food connections: Keep a meal-pain diary noting what you ate and pain intensity 30/60/90 minutes afterward
Seek Appropriate Medical Evaluation
Start with your primary care physician, but be prepared to advocate for specific tests. Basic X-rays won’t reveal pancreatic problems—request CT scans or MRIs if pancreatic involvement is suspected. Mention specifically: “I’m concerned this might be pancreatic back pain given the location and characteristics.”
Emergency indicators: Seek immediate care if back pain is accompanied by severe abdominal pain, persistent vomiting, inability to keep fluids down, or pain so intense you can’t find a comfortable position.
Prevention and Early Detection Strategies
While you can’t prevent all pancreatic conditions, these strategies improve early detection chances when back pain appears.
Monthly Self-Assessment Protocol
Perform these checks monthly if you have risk factors like family history, chronic alcohol use, or gallstone history:
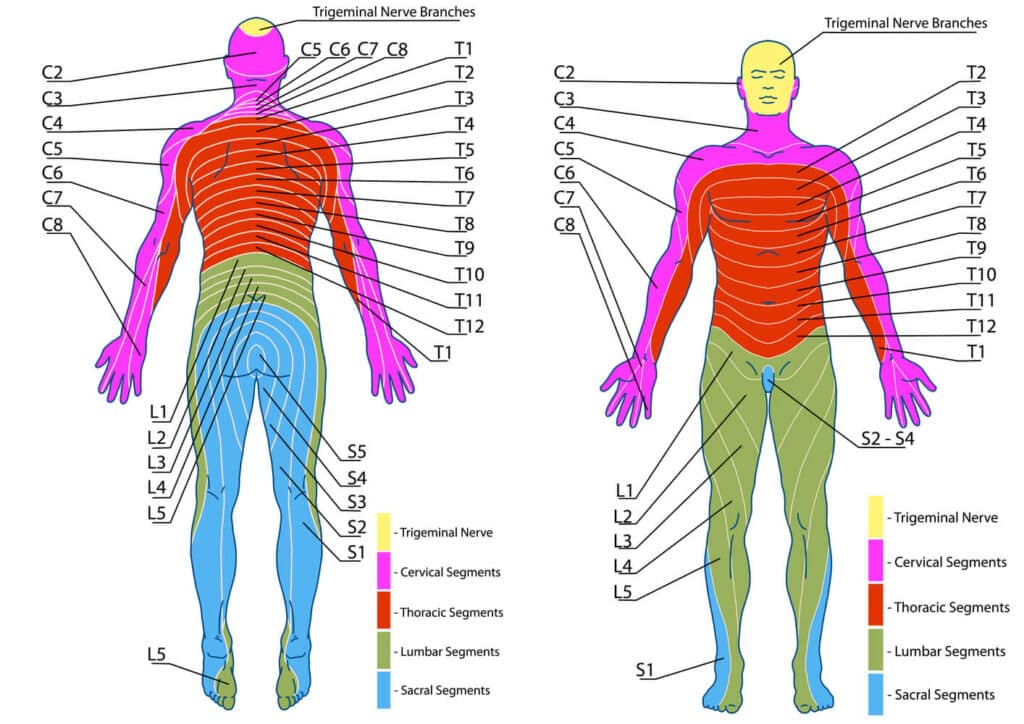
- Pain mapping: Note the exact location of any back discomfort on a body diagram
- Position testing: Assess how pain responds to lying flat versus leaning forward
- Food correlation: Track any connections between meals and pain intensity
Risk Factor Awareness
Patients over 50 with persistent mid-back pain should maintain heightened awareness of pancreatic possibilities. New-onset diabetes alongside back pain creates an urgent need for evaluation, as the pancreas regulates insulin production and tumors can disrupt this function while causing back pain.
Early recognition of these specific location patterns can lead to diagnosis at more treatable stages. If your back pain feels different from typical muscle or joint pain—particularly if it matches these specific patterns—don’t delay seeking medical evaluation. Your awareness of pancreas back pain location could be the critical factor in catching serious conditions before they progress.

