That sharp stab when lifting your newborn or the constant throb during nighttime feedings isn’t just “normal exhaustion”—it’s postpartum back pain affecting up to 45% of new mothers within the first two months. While often dismissed as inevitable, this discomfort transforms simple caregiving tasks into painful ordeals that strain your recovery and steal precious bonding moments. The good news? Most women find significant relief within three to six months through specific, evidence-based strategies. This guide delivers actionable solutions to identify your pain source, implement immediate relief, and rebuild strength so you can care for your baby without wincing.
Why Your Postpartum Back Pain Isn’t “Just Hormones”
Relaxin’s Lingering Joint Instability
Your body continues producing relaxin for up to six weeks after delivery—keeping pelvic ligaments unnaturally loose and sacroiliac joints unstable. This hormone, crucial for childbirth, creates a “wobbly foundation” where joints shift during everyday movements like standing from a nursing chair. Combine this with plummeting estrogen and progesterone levels that reduce muscle tone, and your spine loses critical support exactly when you’re lifting 8-12 pound weights (your baby!) dozens of times daily.
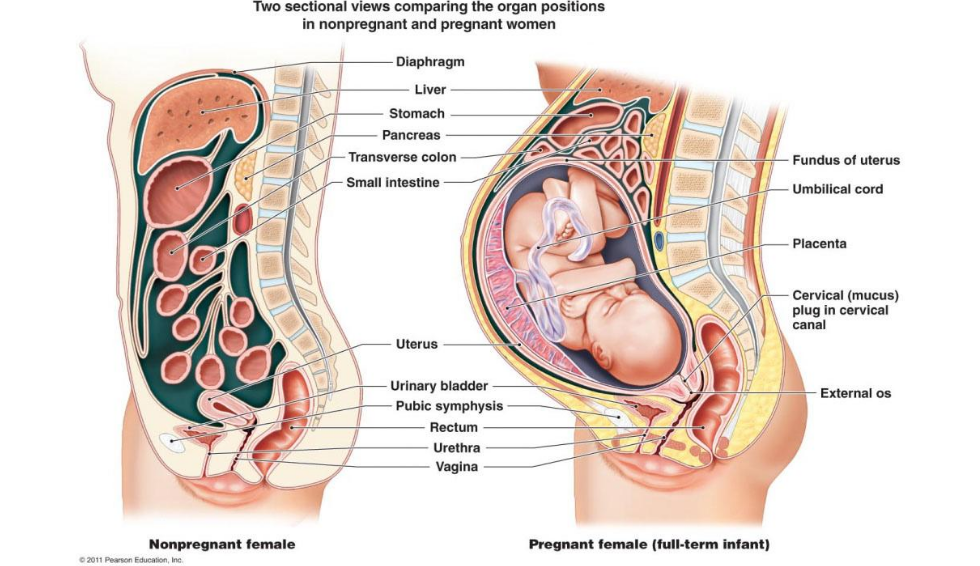
Pregnancy’s Lasting Physical Impact
Your expanding uterus forced an exaggerated forward tilt in your lower spine (lumbar lordosis) that strained back muscles for months. Now, weakened abdominal muscles—often separated (diastasis recti)—and fatigued pelvic floor muscles fail to stabilize your core. Visual cue: Notice if your lower back arches excessively when standing or if you struggle to engage your abs when sitting up. This compromised foundation transfers all lifting stress directly to vulnerable spinal joints.
Baby Care Movements That Worsen Pain
Repetitive motions like bending over a low changing table or hunching forward during breastfeeding create cumulative trauma. Critical mistake: Cradling your baby with one hip while reaching for supplies forces uneven spinal loading. Do this 30+ times daily with already unstable joints, and pain becomes inevitable. Prioritize modifying these movements immediately—they’re the fastest path to relief.
Pinpoint Your Specific Pain Pattern

Sacroiliac Joint Pain: The “Hip Out of Place” Feeling
This sharp, one-sided ache in your lower back or buttock worsens when standing on that leg or transitioning from sitting. Self-test: Press fingers firmly over the dimples at your belt line. If you consistently pinpoint one spot (Fortin finger test), it’s likely sacroiliac dysfunction—accounting for 15-25% of postpartum back pain cases. Avoid twisting motions like reaching across the bed to grab diapers.
Tailbone Trauma From Delivery
Difficult vaginal births can bruise, fracture, or dislocate your coccyx, causing searing pain when sitting or rising. Pro tip: Use a donut-shaped cushion with an open center to relieve pressure. If pain persists beyond 8 weeks, request an X-ray to rule out fracture—especially if you had forceps or vacuum delivery.
Upper Back Strain From Breastfeeding Posture
Hunching over your baby with rounded shoulders strains weakened thoracic muscles. Visual cue: Check if you have “text neck” (head jutting forward) while nursing. This posture compresses cervical discs and triggers tension headaches. Always position baby at breast height using supportive pillows—not by lowering yourself to the crib.
When to Call Your Doctor Immediately
Emergency Warning Signs
Seek urgent care if you experience:
– Leg numbness or weakness (like foot drop when walking)
– Loss of sensation in your inner thighs or genital area
– Bowel/bladder incontinence (can’t feel when you need to go)
– Fever with back pain (sign of infection)
– Pain that intensifies daily instead of gradually improving
Smart Timeline for Non-Emergency Care
Schedule an appointment if pain:
– Prevents you from carrying your baby comfortably after 6 weeks
– Wakes you nightly beyond 8 weeks postpartum
– Persists past the 3-month mark despite home care
Early intervention prevents temporary strain from becoming chronic pain. Don’t wait until the 6-month pediatric checkup.
Instant Relief Tactics for Sleep-Deprived Moms
Pain-Reducing Position Swaps
Breastfeeding hack: Place a rolled towel under your sitting bone on the painful side to level your pelvis. Keep feet flat on a stool so knees sit higher than hips—this reduces lumbar strain by 30%. Diaper change fix: Raise the table to hip height. If stuck with a low surface, kneel on one knee instead of bending at the waist.
Heat vs. Cold: Exactly When to Use Each
- Acute sharp pain (first 48 hours): Apply cold packs for 10 minutes every 2 hours to reduce inflammation. Wrap in thin cloth to avoid skin damage.
- Chronic dull ache: Use heating pads on low for 15-20 minutes before nursing or lifting baby. Warning: Never sleep with a heating pad—nerve damage risk increases dramatically in fatigued new moms.
Breastfeeding-Safe Pain Relief
- First-line: Acetaminophen (Tylenol) every 6 hours as directed—safe for milk supply.
- Second-line: Ibuprofen 400mg every 8 hours (max 1200mg/day) after confirming with your OB. Pro tip: Take 30 minutes before painful activities like long feedings.
- Avoid: Aspirin or naproxen without explicit provider approval—they transfer more readily to breastmilk.
Core Recovery Exercises: Week-by-Week Plan
First 14 Days: Gentle Reconnection
Diaphragmatic breathing (do hourly): Lie on back with knees bent. Place hands on lower ribs. Inhale to expand ribs sideways (not belly), exhale slowly while drawing navel toward spine. This reactivates deep core muscles without strain. Key: Stop if you feel pelvic pressure—indicates overexertion.
Pelvic floor pulses: While breathing out, gently lift pelvic floor muscles (like stopping urine flow) for 3 seconds. Release fully. Do 10 reps, 5x/day. Critical: Never hold your breath—this increases abdominal pressure.
Weeks 3-6: Build Foundational Strength
Supported bridges: Lie with knees bent, feet flat. Place a pillow under hips. Lift pelvis 2 inches while exhaling, engaging glutes. Hold 5 seconds. Do 2 sets of 8 daily. Progression: Remove pillow when pain-free for 3 days.
Wall angels: Stand with back against wall, feet 6 inches forward. Press lower back, upper back, and head to wall. Slide arms up and down like a snow angel. Do 2 sets of 10 daily to counteract breastfeeding hunch.
Beyond Week 6: Functional Movement
Bird-dog on forearms: On hands and knees, lower to forearms. Extend opposite arm and leg straight without tilting hips. Hold 5 seconds. Do 2 sets of 8/side. Warning: Skip if you have diastasis recti wider than 2 fingers.
Heel slides: Lie on back, knees bent. Slowly slide one heel out until leg is straight, then back. Do 10 reps/side to improve hip mobility without straining the back.
Professional Treatments Worth Pursuing

Physical Therapy Secrets for New Moms
Specialized therapists use biofeedback sensors to show you exactly how to engage weakened transverse abdominis muscles during baby lifts. They’ll also teach “hip hinge” mechanics—bending at the hips, not waist—to protect your spine during 100+ daily pickups. Insurance tip: Most plans cover 6-12 visits postpartum—request a referral at your 6-week checkup.
Evidence-Based Complementary Care
- Myofascial release massage: Focuses on pelvic floor and hip flexors (not deep tissue) to reduce referred back pain. Verify therapist’s prenatal/postpartum certification.
- Acupuncture: Studies show 50% pain reduction in 8 weeks for sacroiliac dysfunction when needles target specific meridians near the sacrum.
- Chiropractic: Only seek practitioners certified in Webster Technique—they use low-force adjustments safe for relaxed ligaments.
Prevention Tactics for Long-Term Relief
Must-Have Ergonomic Gear
- Baby carriers: Choose structured hip seats (not pouch slings) with waist belts that transfer baby’s weight to your pelvis—not shoulders. Look for “ergonomic” certification.
- Nursing stations: Use a glider with lumbar roll and footrest. Place baby’s head at your nipple height using Boppy pillows—never lean forward.
- Strollers: Opt for ones with adjustable handle heights so you stand tall while pushing.
Safe Return-to-Exercise Protocol
Critical timeline: Wait 12-16 weeks before running or jumping—even if your OB clears exercise at 6 weeks. First, master these milestones:
1. Pain-free walking 30+ minutes
2. Holding modified plank 45 seconds
3. No urine leakage when coughing
Start with elliptical or swimming before adding impact. Red flag: Any pelvic pressure during exercise means stop immediately.
Weight Management That Supports Healing
Modest weight loss (0.5-1 lb/week) reduces mechanical stress on lumbar discs. Breastfeeding-friendly approach: Prioritize protein at every meal (keeps milk supply stable) and add 10-minute post-feeding walks. Avoid restrictive diets—they slow tissue repair.
Your Realistic Recovery Roadmap
Most new moms experience 70% improvement in postpartum back pain within 12 weeks by consistently applying these strategies. Full resolution typically takes 3-6 months, but persistent pain beyond 6 months often responds to targeted physical therapy. Key factors: Women with pre-pregnancy back issues or higher BMI may need 8-10 weeks longer—but starting early prevents chronicity. Remember: Your body performed a miracle. Honor its healing process with patience, smart modifications, and professional support when needed. Every pain-free moment you reclaim is time you can truly enjoy with your baby.