If you’ve struggled with persistent back pain that won’t respond to painkillers, physical therapy, or lifestyle changes, radiofrequency ablation (RFA) could be your breakthrough solution. Unlike temporary pain masking, RFA targets the actual pain pathways causing your discomfort. This procedure offers significant pain reduction for 60-80% of appropriately selected patients, with effects lasting 6-24 months. If you’re tired of carrying that constant ache and want to reclaim your active life, understanding how RFA for back pain works could be your first step toward lasting relief.
Chronic back pain affects millions who’ve exhausted conservative treatments without finding sustainable solutions. When your daily activities become limited by persistent discomfort, RFA provides a precise, minimally invasive option that disrupts pain signals at their source. In this guide, you’ll discover exactly who qualifies for RFA, what happens during the procedure, realistic recovery timelines, and the actual success rates based on clinical evidence—not marketing claims.
Why RFA Targets Your Specific Back Pain Source

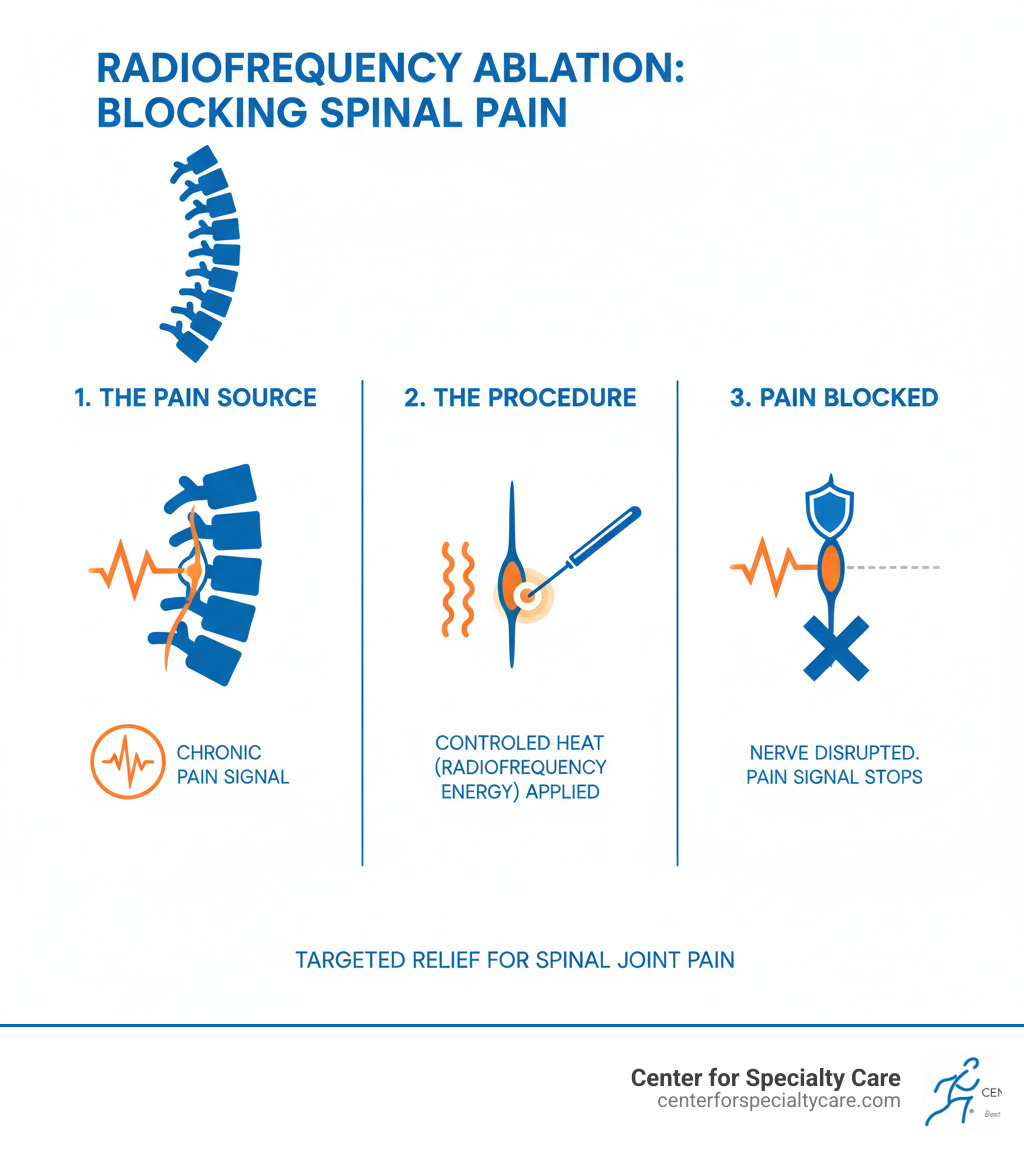
RFA works by creating controlled thermal lesions on specific nerves transmitting your pain signals. During the procedure, your pain specialist inserts a hair-thin needle guided by real-time imaging to reach the exact nerve branches responsible for your discomfort. The electrode at the needle’s tip then delivers precise radiofrequency energy, heating the tissue to 60-90°C to create a small lesion that interrupts pain transmission.
RFA specifically treats these common back pain sources:
– Lumbar facet joints – small stabilizing joints between vertebrae that commonly cause mechanical back pain
– Sacroiliac (SI) joints – where your spine connects to your pelvis, often overlooked as a pain generator
– Disc-related pain – from damaged spinal discs, though results vary between conventional and cooled RFA techniques
Unlike medications that affect your entire nervous system, RFA targets only the pain-conducting nerves while preserving motor and sensory function. This precision means you’ll experience significant pain reduction without the side effects of systemic medications. Most patients notice improvement within 1-3 weeks as the treated nerves stop sending pain signals to your brain.
Qualify for RFA: The Critical Screening Process You Must Pass
Not everyone with back pain qualifies for radiofrequency ablation. Your pain specialist uses a strict three-step screening process to ensure you’re an ideal candidate and maximize your chances of success.
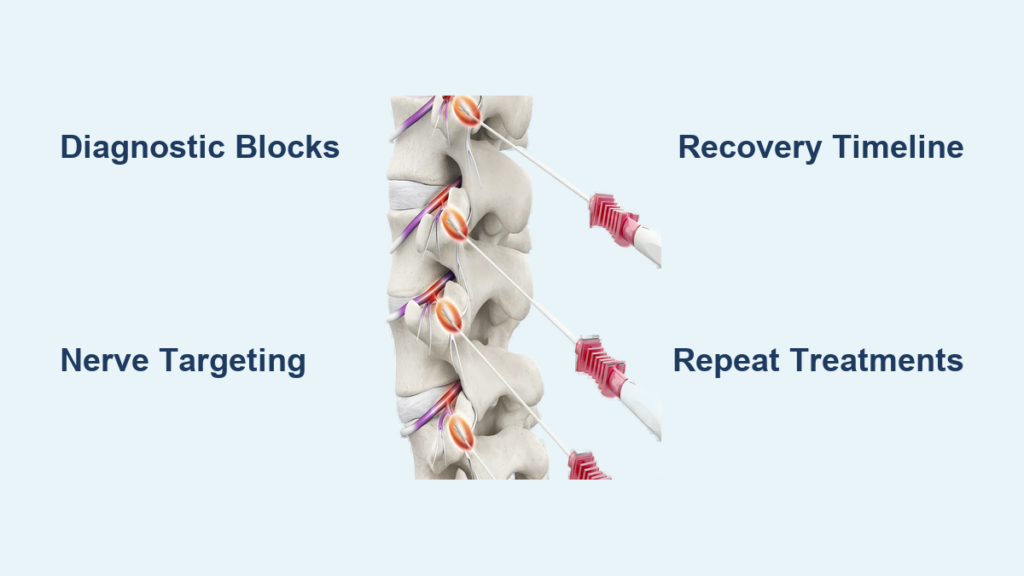
Diagnostic Nerve Blocks: Your Pain Relief Trial Run
Before approving RFA, your doctor must confirm that specific nerves cause your pain through diagnostic nerve blocks. During this test, your provider injects a local anesthetic near suspected pain-transmitting nerves. If this provides at least 50% pain relief for several hours, you’ve passed the critical test proving those nerves are your pain source.
You qualify for RFA if you meet all these criteria:
– Chronic back pain lasting 3+ months
– Failed multiple conservative treatments (physical therapy, medications)
– Positive response to diagnostic nerve block (≥50% pain reduction)
– Clear imaging showing treatable pain source (facet joint arthritis, SI joint dysfunction)
Automatic Disqualifiers That Prevent RFA
Certain conditions make RFA unsafe or ineffective. Be honest with your provider about these potential barriers:
– Active infections near the injection site
– Uncontrolled bleeding disorders or blood thinners you cannot pause
– Pregnancy
– Severe spinal instability requiring surgical intervention
– Psychological conditions affecting pain perception or treatment compliance
What to Expect During Your RFA Procedure
Your RFA session follows a carefully orchestrated sequence designed for maximum precision and safety. Understanding each step reduces anxiety and helps you prepare mentally for the experience.
Precise Needle Placement Using Advanced Imaging
You’ll lie face-down on a specialized table while your pain specialist uses fluoroscopy (real-time X-ray) or CT guidance to position a 20-22 gauge needle next to your target nerves. Before creating lesions, your doctor performs two critical tests:
– Sensory test: Low electrical stimulation confirms proximity to pain nerves
– Motor test: Ensures no movement occurs, verifying no motor nerves are affected
Creating the Pain-Interrupting Lesion
Once needle placement is confirmed, radiofrequency current heats the tip for 60-150 seconds at 60-80°C. Your provider may create multiple lesions by slightly repositioning the needle. The entire procedure takes 15 minutes to 2 hours, depending on how many nerve levels require treatment. You’ll receive local anesthetic at the injection site plus optional light sedation to keep you comfortable while remaining alert enough to respond to testing questions.
Realistic Recovery Timeline After RFA
Your recovery after RFA follows a predictable pattern with specific milestones. Knowing what to expect helps you plan activities and recognize normal versus concerning symptoms.
First 48 Hours: Critical Rest and Monitoring Period
After your procedure, you’ll rest in recovery for 30-60 minutes while staff monitors your vital signs. You cannot drive for 24 hours due to sedation effects. Most patients experience:
– Immediate soreness at injection sites (like a deep bruise)
– Temporary numbness along treated nerve pathways
– Mild swelling requiring ice packs (20 minutes on/20 off)
Activity restrictions for first 48 hours:
– No heavy lifting (nothing over 5-10 pounds)
– Avoid prolonged sitting or bending
– No strenuous exercise
– Light walking encouraged starting same day
Weeks 1-2: Managing Temporary Soreness
This phase often brings the most discomfort as inflammation peaks before subsiding. 85% of patients experience temporary pain flare-up for 1-2 weeks that responds well to:
– Ice therapy
– Over-the-counter NSAIDs
– Gentle stretching
– Short walks every 2-3 hours
Weeks 3-6: When Real Pain Relief Begins
Most patients notice significant improvement during this period as the treated nerves stop transmitting pain signals. Your first follow-up appointment at 2-6 weeks assesses your response. If you achieved 50%+ pain reduction, your provider will likely recommend starting physical therapy to strengthen supporting muscles and maximize your results.
RFA Success Rates: What Clinical Evidence Really Shows

Understanding the actual effectiveness of RFA for your specific pain source prevents unrealistic expectations and helps you make informed decisions.
Lumbar Facet Joint Pain Results
Six major studies confirm RFA’s effectiveness for facet joint pain:
– Immediate relief: 1.5-3 point pain reduction on 10-point scale
– 3-6 months: 5 of 6 studies show significant improvement versus placebo
– Duration: Average 12 months relief before nerves regenerate
Sacroiliac Joint Pain Outcomes
Two key studies demonstrate strong results for SI joint pain:
– Cohen 2008: Pain dropped from 6.1 to 2.4 on a 10-point scale within one month
– Patel 2012: Sustained 50% improvement at three months compared to control group
Discogenic Pain: Know the Difference Between Techniques
Results vary significantly based on RFA technique:
– Cooled RFA: One study showed significant 6-month improvement for disc pain
– Conventional RFA: Two studies found no benefit over placebo for discogenic pain
Managing Risks: What Could Go Wrong With RFA
While serious complications are rare, understanding potential risks helps you recognize warning signs and respond appropriately.
| Common Side Effect | Occurrence Rate | Management Strategy |
|---|---|---|
| Injection site soreness | 70-80% | Ice packs, NSAIDs |
| Temporary numbness | 40-50% | Resolves within days |
| Mild bruising | 30-40% | Self-limiting |
| Temporary pain increase | 20-30% | Short-term medication |
Seek immediate medical attention if you experience:
– Severe or worsening pain beyond typical soreness
– New weakness or numbness in legs or feet
– Fever above 100.4°F or spreading redness at injection site
– Expanding bruise or significant swelling
Cost, Insurance, and Planning for Repeat Treatments
Understanding the financial aspects of RFA prevents unpleasant surprises and helps you plan for long-term pain management.
Insurance Coverage Requirements
Most insurance plans cover RFA when specific criteria are met:
– Documentation of 3+ months of chronic back pain
– Proof of failed conservative treatments (PT, medications)
– Positive diagnostic nerve block showing ≥50% pain relief
– Prior authorization obtained before procedure
Without insurance, RFA costs $2,500-$4,000 per treated spinal level in the United States. Many pain clinics offer payment plans for self-pay patients.
When to Consider Repeat RFA
Nerves typically regenerate 6-12 months after treatment. Repeat RFA is both safe and effective if:
– Your initial procedure provided ≥50% pain relief for 6+ months
– Pain has returned to pre-procedure levels
– Diagnostic blocks remain positive
Long-term outlook: 60-80% maintain significant relief at 6-12 months, while 30-40% continue benefiting at 24 months. Patients with strong initial responses to diagnostic blocks achieve the best long-term results.
Making Your RFA Decision: Next Steps for Pain Relief
RFA for back pain isn’t a cure for underlying spine conditions, but for properly selected patients, it provides a valuable pain reduction window that enables meaningful lifestyle improvements. The critical factor determining success is proper patient selection—you must have a confirmed, treatable pain source through diagnostic nerve blocks.
Take these immediate next steps:
1. Schedule a consultation with a board-certified pain specialist
2. Request diagnostic nerve blocks if you haven’t had them
3. Review your imaging studies to confirm a treatable pain generator
4. Discuss conventional versus cooled RFA based on your specific condition
If you’ve struggled with chronic back pain that won’t respond to conservative treatments, RFA could be your pathway to reclaiming the activities you love. By targeting the actual pain pathways rather than masking symptoms, this precise procedure offers many patients months of meaningful pain reduction and improved quality of life.