You’re not imagining it—when your lower back feels like it’s being crushed in a vice during your period, it’s more than “normal cramps.” Severe back pain with period affects 72% of women who experience menstrual discomfort, often radiating from the uterus through shared nerve pathways. If you’ve ever canceled plans because pain rated 7/10 or higher left you doubled over for more than three days, this guide delivers clinically proven strategies to reclaim your life. Stop accepting “that’s just your period” as an explanation when solutions exist.
This isn’t about enduring pain—it’s about targeted interventions. We’ll cut through medical jargon to show exactly why your back seizes up during menstruation, how to distinguish dangerous symptoms from manageable discomfort, and which relief methods work fastest based on 2025 clinical evidence.
Why Prostaglandins Are Tormenting Your Lower Back
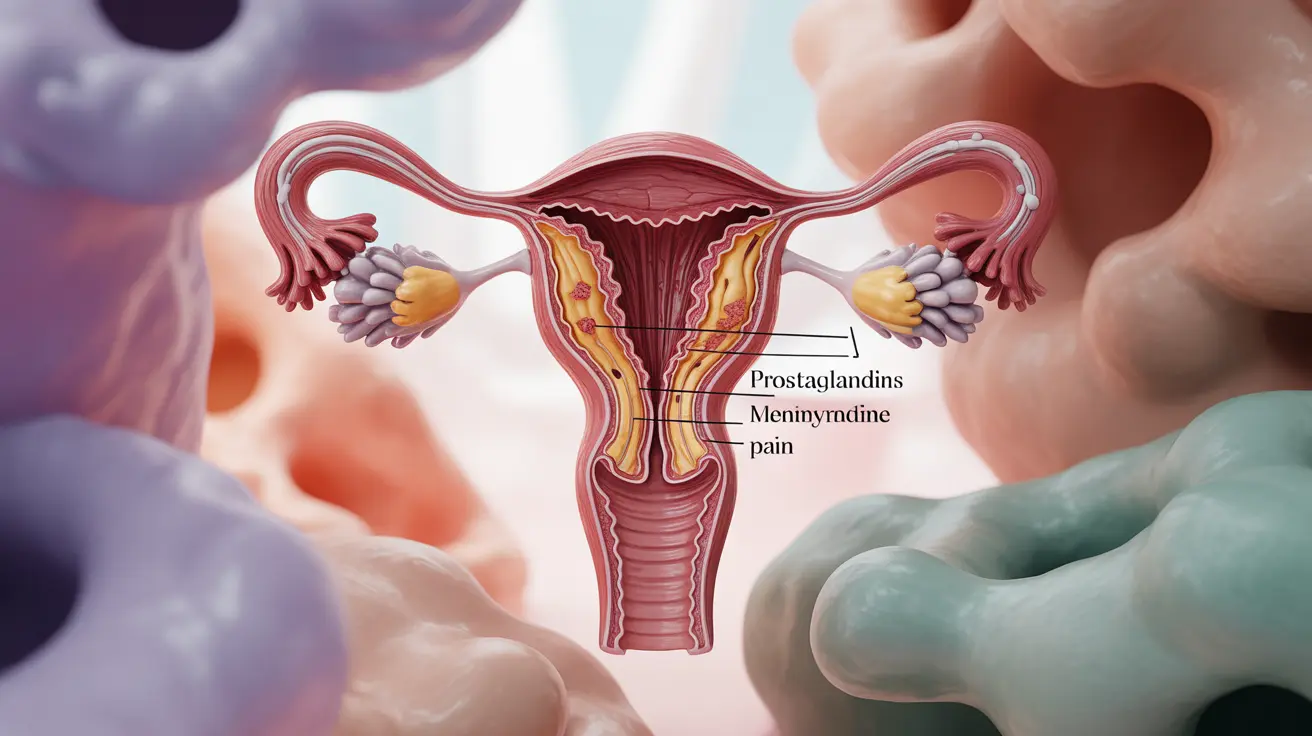
Your body’s prostaglandin surge—hormone-like substances that trigger uterine contractions—directly attacks your back muscles. When endometrial cells release excessive PGF₂α before your period starts, it causes intense uterine spasms that refer pain to your lumbar region via viscerosomatic reflexes. This inflames nerves connected to your multifidus and quadratus lumborum muscles, creating that signature deep, radiating ache.
Hormones That Lower Your Pain Tolerance
As estrogen and progesterone plummet pre-period, your pain threshold drops significantly. Simultaneously, fluid retention increases mechanical pressure on your lumbar spine—turning mild discomfort into debilitating pain. This dual assault explains why heat therapy becomes critical: it directly counteracts the muscle spasms amplified by these hormonal shifts.
Spotting Referred Pain vs. Spinal Issues
True menstrual back pain originates from uterine contractions referring discomfort through T10-L1 nerve pathways. You’ll feel a diffuse, cramp-like ache centered in your sacrum—not sharp, localized pain from a herniated disc. If leg numbness or tingling occurs only during your period and resolves afterward, it’s likely referred pain. Persistent neuropathic symptoms require spinal evaluation.
When “Normal Cramps” Signal a Medical Emergency
Mild back discomfort responding to ibuprofen within an hour falls within typical dysmenorrhea. Severe back pain with period crosses into danger territory when it meets any of these criteria:
– Pain intensifies to 7+/10 on a pain scale
– Lasts longer than 72 hours continuously
– Radiates into your legs with numbness or weakness
– Triggers vomiting, dizziness, or fainting spells
– Forces you to miss work or school for multiple days
Life-Threatening Red Flags You Can’t Ignore
Seek ER care immediately if you experience:
– Fever above 100.4°F combined with back pain (signaling possible pelvic infection)
– Loss of bladder control during menstruation (cauda equina syndrome risk)
– Sudden, excruciating pain after age 40 that worsens daily
– Vomiting blood or inability to keep fluids down
These indicate conditions like septic abortion or spinal endometriosis requiring urgent intervention.
Diagnosing the Root Cause Behind Your Agony

Primary Dysmenorrhea: The Prostaglandin Overload
This affects women without pelvic pathology, where excessive prostaglandins cause uterine ischemia. Pain begins with your period onset and typically eases within 48 hours. NSAIDs work best here—they block prostaglandin production at the source. If ibuprofen fails, you likely have secondary dysmenorrhea requiring deeper investigation.
Endometriosis: The Silent Invader
Suspect this if back pain starts 1-2 weeks before your period and includes:
– Heavy, clotted bleeding lasting >7 days
– Deep pelvic pain during intercourse
– Gradually worsening symptoms over months
– Cyclical bowel/bladder discomfort
Endometrial implants on pelvic nerves refer constant, progressive backache. Early laparoscopic excision preserves fertility and prevents nerve damage.
Adenomyosis: The Uterine Wall Invasion
When endometrial tissue grows into your uterine muscle wall, you’ll experience:
– A tender, globular uterus on exam
– Prolonged bleeding causing anemia (fatigue, shortness of breath)
– Diffuse low-back pressure throughout your entire period
– Pain persisting beyond menstrual flow
Pelvic ultrasound often shows an enlarged uterus with asymmetric walls—key for diagnosis.
20-Minute Emergency Relief Tactics
Heat Therapy Protocol That Beats Ibuprofen
Place a heating pad at 104°F on your lower back for 20 minutes (not directly on skin). Remove for 20 minutes to prevent skin damage, then repeat. A 2018 meta-analysis confirmed this cycle reduces pain as effectively as 400mg ibuprofen within 30 minutes by relaxing muscle spasms and improving blood flow. Skip hot baths—they dilate blood vessels and may increase cramping.
NSAID Timing: Your Secret Weapon
Never wait for pain to peak. Start NSAIDs 1-2 days before your period begins:
– Ibuprofen: 400-600mg every 6-8 hours (max 2400mg/day)
– Naproxen: 500mg twice daily
– Mefenamic acid: 500mg initial dose, then 250mg every 6 hours
Taking them early blocks prostaglandin synthesis before inflammation peaks. If you miss this window, combine with heat for faster relief.
TENS Unit Setup for Instant Nerve Interruption
Set your TENS unit to 80-100 Hz frequency. Place electrodes on either side of your spine at waist level (L4-L5 vertebrae). Run for 30 minutes—studies show this reduces pain by 30-40% when paired with NSAIDs by disrupting pain signals. Keep units charged; this is your fastest non-drug option.
Long-Term Fixes That Actually Work

Hormonal Treatments: Beyond Birth Control Pills
While combined oral contraceptives (20-35μg ethinyl estradiol) suppress ovulation for 80% of women, try these if they fail:
– Levonorgestrel IUD: Provides 5 years of continuous relief with minimal systemic hormones
– Progestin-only pills: Ideal for migraine sufferers sensitive to estrogen
– Elagolix: GnRH antagonist for endometriosis (prescription-only)
Critical tip: Allow 3-4 cycles for hormonal treatments to reach full effect—don’t quit prematurely.
Physical Therapy Moves to Do Daily
Perform these during and between periods:
– Cat-Cow stretch: On hands and knees, alternate arching and rounding your spine (10 reps)
– Pelvic tilts: Lie flat, press lower back into floor while tightening abs (15 reps)
– Seal stretch: Lie prone, lift chest while keeping hips down (hold 30 seconds)
These counteract prostaglandin-induced muscle tension. Consistency matters—do them 5 minutes daily, not just during pain flares.
Prevent Flare-Ups Before They Start
Anti-Inflammatory Diet Swaps That Reduce Pain
Stop feeding inflammation:
– Eat daily: Fatty fish (salmon/mackerel), spinach, blueberries
– Ditch: Processed sugars, excess salt, and alcohol (they worsen fluid retention)
– Supplement smart: 400mg magnesium + 100mg vitamin B1 daily (proven to lower pain scores)
Hydrate with 2+ liters of water—dehydration concentrates prostaglandins in your bloodstream.
Exercise That Targets Menstrual Back Pain
Avoid high-impact workouts during painful days. Instead:
– Swim or walk 15 minutes daily (boosts endorphins without jarring)
– Practice yoga poses like Child’s Pose (kneeling, arms extended forward) for 5 minutes
– Never skip strength training: 2 weekly sessions of core work prevents back strain
Smoking cessation is non-negotiable—nicotine increases prostaglandin production by 25%.
Track Symptoms to Unlock Your Personal Cure
The 30-Second Daily Pain Diary
For 2-3 cycles, log:
– Pain start/end time (note if it begins before bleeding)
– Location (low back? radiating to legs?)
– Severity (0-10 scale)
– What relieved it (e.g., “heat for 20 min = 3-point drop”)
This reveals patterns your doctor might miss—like pain consistently worsening after caffeine.
When to Demand Advanced Testing
If NSAIDs + heat fail after 3 cycles, insist on:
1. Pelvic ultrasound (screens for fibroids/adenomyosis)
2. MRI if endometriosis is suspected (ultrasound often misses it)
3. Laparoscopy if symptoms persist—still the gold standard for diagnosis
Never accept dismissal of severe back pain with period as “normal.” Document everything.
Your 5-Day Pain Prevention Plan
| Cycle Day | Critical Actions |
|---|---|
| Day -2 | Start NSAIDs + apply heat 20 min |
| Day 1 | Take magnesium, do Cat-Cow stretches |
| Day 2 | Use TENS unit if pain >5/10 |
| Day 3 | Assess if pain resolves; if not, call gynecologist |
| Day 4+ | Review diary; adjust next cycle’s plan |
Stop Suffering—Your Back Pain Isn’t Normal
Severe back pain with period is your body signaling imbalance—not weakness. Start tonight: set a reminder to take magnesium, charge your TENS unit, and track tomorrow’s pain level. If discomfort disrupts your life for more than three days, demand investigation for endometriosis or adenomyosis. Early intervention prevents nerve damage and preserves fertility. You deserve relief that works—begin your symptom diary now and reclaim your cycle.